Infection Control Biological Substances Incident Protocol
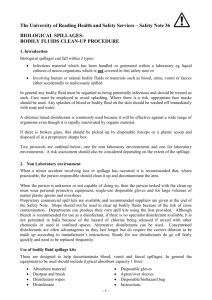
advertisement

Beechdale Health Centre Infection Control Biological Substances Incident Protocol Document Control A. Confidentiality Notice This document and the information contained therein is the property of Beechdale Health Centre. This document contains information that is privileged, confidential or otherwise protected from disclosure. It must not be used by, or its contents reproduced or otherwise copied or disclosed without the prior consent in writing from Beechdale Health Centre. B. Document Details Classification: Author and Role: Organisation: Document Reference: Current Version Number: Current Document Approved By: Date Approved: C. internal ARUN VENUGOPAL AND JANE SMITH, PM AND PN Beechdale Health Centre Icbsip1 1 Arun Venugopal 16.10.2012 Document Revision and Approval History Version 1 Doc. Ref – Date 16.10.2012 Version – Version Created By: Version Approved By: Arun and Jane Arun and Jane Filename: Infection Control Biological Substances Incident Protocol Comments Created from IQ CQC original Page 1 of 5 Definition For the purposes of this protocol, the term biological substances relates to any fluid generated by the body. For example: Blood; Vomit; Sputum / saliva; Urine; Breast milk; Wound drainage; Faecal matter. This list is not exhaustive, but merely an illustration of the variety of fluids produced by the body. Aim This protocol is intended to give guidance for staff members when dealing with general incidents involving accidental spillage of, or exposure to biological substances, in order to maintain the highest possible standards of infection control. Spillages This section outlines the procedures that should be taken following any spillage, large or small. Please note that only clinical staff should be involved in the clean-up of any spilled biological substance. Administrative and secretarial staff should inform one of the clinical team if they become aware of a spillage of this nature. Blood Small spills on hard surfaces, objects or equipment – should be wiped using a paper towel soaked with sodium hypochlorite 10,000 ppm (1%) solution. Suitable hand PPE (not necessarily sterile) should be worn, and the PPE and towels should be discarded into a yellow clinical waste bag for incineration. A Practice Blood Spillage Kit containing the necessary items is to be found room 10. Hypochlorite solutions are corrosive, so treat the affected surface (post-cleaning) by rinsing with clean water, then drying thoroughly. Large spills on hard surfaces, objects or equipment – should be treated with absorbent, chlorinereleasing granules (e.g. Sodium Dichloroisocyanurate). This treatment ensures that the active disinfecting agent is in contact with any present micro-organisms in the entire spill, and also limits the spread of the blood to a smaller area. Liquid disinfectants should not be used as they will only encourage the spread of the spill and will not successfully achieve homogeneous mixing and effective disinfection. Doc. Ref – Version – Filename: Infection Control Biological Substances Incident Protocol Page 2 of 5 Do not use more than quarter of a container of granules, and try to make sure the area is well ventilated as the granules will release chlorine vapour when they come into contact with the spillage. A Practice Blood Spillage Kit containing the necessary items is to be found room 10 The following protocol should be used: Cordon-off the area where the large spillage has taken place (Wet Floor signs work well); Staff member(s) involved in the clean-up should use appropriate PPE (gloves, apron); Sprinkle the Sodium Dichloroisocyanurate (or equivalent) granules evenly until the entire spillage is covered. Leave undisturbed for two minutes; After this period apply more granules if there is more blood left than originally thought. Leave for an additional two minutes; Once total absorption has taken place, use a disposable scoop to collect the granules, and dispose of them and the scoop in a yellow clinical waste sack; Any remaining traces should be removed with paper towels soaked with Sodium Hypochlorite 10,000 ppm (1%) solution; Add the towels to the clinical waste sack, along with the gloves and then apron; Rinse the area / equipment with general-purpose liquid detergent and clean water; Finally, ensure hands are thoroughly washed and dried. Spillages onto absorbent surfaces – will be most effectively cleaned using hot water and liquid detergent, along with disposable cloths and paper towels. PPE should be worn for this process, with all waste to be discarded into a yellow clinical waste sack. If the spillage has been onto clothing, this should be dealt with as per separate policy – “Laundering of Linen, other Fabric Materials and Uniforms”. Spillages onto skin or into mouth or eyes Intact skin – blood should be washed off immediately using plenty of warm water and soap. Pay great attention to under the fingernails. Broken skin – wash the blood from affected area with plenty of warm water and soap, then encourage the wound to bleed. Mouth / eye contact – wash / rinse the affected area with plenty of warm water. For all blood contact with skin / mouth / eyes, contact your Practice’s Occupational Health support facility for advice (or local A&E department if Occ. Health not available), report the incident to the Practice manager and complete an incident report form (note the nature of the incident and source of the potentially contaminated blood). Other Bodily Fluids There is a much lower chance of a blood-borne virus being transmitted through bodily fluids other than blood. Regardless of whether a patient is known, or suspected to have a blood-borne virus, spilled body fluids should always be treated according to the procedures described in the section on blood spillage. As per the procedure for large blood spills; do not use more than quarter of a container of granules, and try to make sure the area is well ventilated as the granules will release chlorine vapour when they come into contact with the spillage. Never use chlorine granules for urine. Doc. Ref – Version – Filename: Infection Control Biological Substances Incident Protocol Page 3 of 5 Notifying the CQC of Serious Injury to a person who uses the Service The principal GP or Practice Manager at the Practice is responsible for notifying the CQC without delay about events that lead to: Serious injury to any person who uses the service. An injury requiring treatment by a healthcare professional to avoid death or serious injury. These serious injuries include: Injuries that lead to or are likely to lead to permanent damage – or damage that lasts or is likely to last more than 28 days – to: A person’s sight, hearing, touch, smell or taste Any major organ of the body (including the brain and skin) Bones Muscles, tendons, joints or vessels Intellectual functions, such as Intelligence Speech Thinking Remembering Making judgments Solving problems. Injuries or events leading to psychological harm, including: Post-traumatic stress disorder Other stress that requires clinical treatment or support Psychosis Clinical depression Clinical anxiety The development after admission of a pressure sore of grade 3 or above that develops after the person has started to use the service (European Pressure Ulcer Advisory Panel Grading) Any injury or other event that causes a person pain lasting or likely to last for more than 28 days Any injury that requires treatment by a healthcare professional in order to prevent: Death Permanent injury Any of the outcomes, harms or pain described above. Where the Registered Person is unavailable, for any reason, practice nurse will be responsible for reporting the serious injury to the CQC. There is a dedicated Notification form for this type of incident. The form is contained in the Outcome 20 document “Notification of Other Incidents – Outcome 20 Composite Statements and Forms” Doc. Ref – Version – Filename: Infection Control Biological Substances Incident Protocol Page 4 of 5 Major Accidents On rare occasions it is possible that the Practice may have to deal with multiple casualties as the result of a major accident or incident. Whilst the pressure on services at this time will be extraordinary, it is important not to forget the basics on infection control, including essential PPE, cleaning protocols, safe-handling of needles and sharps, ensuring all Practice staff are up-to-date with essential immunisations (e.g. Hepatitis B). During a situation such as this there will be a great potential for the spillage of blood or other bodily fluids and possible risk of infection to staff members, either from injured people, or from receptacles and floor spillages. Remember that the safety of patients and staff members is always paramount in every procedure that is undertaken. Patient Bleeds There are often small patient bleeds from minor procedures (e.g. inoculations, taking of specimens, treatment of wounds). Additionally, there are instances of other accidental patient bleeds (e.g. nosebleeds, grazing from falls). The risk of infection from the handling and treatment of such cases will be minor, providing the usual PPE and actions protocols are performed. Staff members should always wear protective gloves and a liquid repellent apron when treating a bleeding patient. If there are any spillages of blood either onto skin, surfaces or equipment, the protocols within this document should be followed. Doc. Ref – Version – Filename: Infection Control Biological Substances Incident Protocol Page 5 of 5