NORTHPOINTE BEHAVIORAL HEALTHCARE SYSTEMS
advertisement

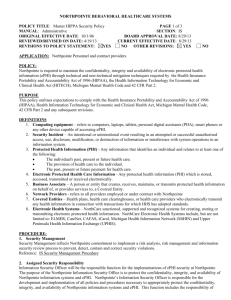
NORTHPOINTE BEHAVIORAL HEALTHCARE SYSTEMS POLICY TITLE: Access to Continuum of Services – Adults MANUAL: Clinical ORIGINAL EFFECTIVE DATE: 10/2/95 REVIEWED/REVISED ON DATE: 4/16/15 REVISIONS TO POLICY STATEMENT: YES NO PAGE: 1 of 3 SECTION: Entry to Care BOARD APPROVAL DATE: 9/26/13 CURRENT EFFECTIVE DATE: 5/1/15 OTHER REVISIONS: YES NO APPLIES TO: This policy applies to all eligible individuals seeking services. POLICY: It is the policy of Northpointe Behavioral Healthcare Systems to make services available to all residents of the State of Michigan and specified contractual individuals without discrimination as to physical or mental disability, race, color, religion, nation origin, sex (within the limitations of the homes to accommodate residents of different sexes), age, marital status, ability or inability to pay, sexual orientation, political affiliation, cultural background or those with limited English proficiency. NorthCare Network’s Access Systems function as the front doors for all Michigan residents and is expected to be available, accessible and welcoming to all individuals on a telephone and a walk-in basis. All residents of Michigan and specified contractual individuals are offered equal access to appropriate and necessary behavioral health services via 24 hour crisis support and referral. Individuals calling for mental health services or supports will be provided timely and welcoming access to eligibility screening. Northpointe Behavioral Healthcare Systems' goal is to guarantee individuals accessibility to an appropriate integrated system of care, honoring the individual’s choices, including service providers, and preferences as negotiated in the person-centered planning and self-determination process. Northpointe Behavioral Healthcare Systems maintains standards for access to services in accordance with Michigan Department of Community Health (MDCH) and NorthCare guidelines and consistent with accreditation standards. Standards have been developed for emergent and routine accessibility of services and to meet medical necessity criteria. Northpointe Behavioral Healthcare Systems' leaders consider the needs of the populations served, available resource, strategies, and settings for delivery of service when making care available to those who need it, providing the care in a continuous manner and using care settings appropriate to individual needs and requests. There are channels of communication among the service providers in order to facilitate the stability, continuity, and comprehensiveness of services to an individual, and are monitored via review of Performance Indicators There is ongoing supervision of direct service personnel that addresses issues of ethics, legal aspects of clinical practices, professional standards, clinical documentation, and cultural competency issues. PURPOSE: Northpointe’s policy is to ensure timely access to appropriate and necessary specialty mental health services and intellectual/developmental disability supports for all eligible individuals, and are supported in exercising choice as to the provider of services, to the extent possible and appropriate. DEFINITIONS: Denying or Limiting Services – In the processing of requests for initial and continuing authorizations of services, any decision to deny a service authorization or to authorize a service in an amount, duration, or scope that is less than requested, must be made by a healthcare professional who has appropriate clinical expertise in treating the enrollee’s condition or disease. Reference 42 CFR 434 Subpart D 438.210(b) (3). Health Care Professional – The staff who are eligible to provide Medicaid services are listed in the Michigan Department of Community Health Medicaid Provider Manual, Chapter for Mental Health/Substance Abuse, Section 2.4. Service Authorization Request – Means a managed care enrollee/guardian’s request for the provision of a service. Reference 42 CFR 431.201. Limited English Proficiency (LEP): An individual with limited English proficiency will be provided assistance in an alternative language format. This could include oral language translation; sign language; and other types of assistance necessary to fully understand how to access and utilize services. It is not recommended that an individual utilize a family member or friend as a language interpreter. If an individual does choose a family member or friend, staff will document this choice. NORTHPOINTE BEHAVIORAL HEALTHCARE SYSTEMS POLICY TITLE: Access to Continuum of Services – Adults MANUAL: Clinical ORIGINAL EFFECTIVE DATE: 10/2/95 REVIEWED/REVISED ON DATE: 4/16/15 PAGE: 2 of 3 SECTION: Entry to Care BOARD APPROVAL DATE: 9/26/13 CURRENT EFFECTIVE DATE: 5/1/15 PROCEDURES: All individuals requesting services from Northpointe during normal business hours will be connected to the NorthCare Centralized Access and Eligibility department for screening and an initial assessment will be scheduled if appropriate. Eligibility is determined following the face-to-face intake assessment. Any service recipient or individual acting on behalf of a service recipient may call Northpointe after hours for emergent and urgent care via local crisis support and referral systems. All providers have the responsibility to assess the need for Limited English Proficiency assistance at the time of access. NBHS defines two acuity levels and access standards for each level: Emergent Situations: Those clinical presentations which involve real and imminent danger to self or others and which require immediate diagnosis and treatment. Assessment and disposition to be completed within 3 hours. Routine: Those situations in which the individual presents as relatively stable and able to function in their current environment, but may require services to improve functioning in one or more settings and/or to alleviate emotional distress, and/or to address significant behavioral disturbances. Assessment to be provided within 14 days of initial request. Initial Request for Services: When a service recipient, legal guardian, or responsible party acting on behalf of an individual initiates a request for services, individuals are asked to identify whether or not they are calling regarding a crisis or urgent matter, and if identified as an emergent situation, are immediately diverted to a crisis support staff member. If the call is identified as a routine request for services, the initial telephone screening completed by NorthCare, identifies service recipient demographics, referral information (including whether or not the individual is referred by a primary EPSDT screener) and collects information for reporting purposes. They will determine potential funding sources and determine an individual’s eligibility for Medicaid specialty services and supports, Healthy Michigan, MI Child (through age 18), and General Fund. The individual who is eligible for Specialty Mental Health services is then scheduled for a bio-psychosocial assessment (i.e. intake) at the appropriate Northpointe office. Those not eligible for Specialty mental Health services will be referred to a provider in their community. The clinical information gathered at the time of initial assessment (either when scheduled face-to-face or when screened by clinical staff) includes an assessment of clinical condition(s) and/or presence of an intellectual/developmental disability or substance abuse concern, addresses degree of functional impairment across settings, determines degree of risk, assesses the individual’s strengths and supports, and determines intensity of service needs. When either case management or supports coordination services are indicated, the provider shall inform individuals of all available options in their area and allow them to choose their provider to the extent possible and appropriate. If the assessment including appropriate Level of Functioning tools indicates that ongoing services are appropriate, an initial treatment plan is developed, the individual is then scheduled with the appropriate service provider to begin treatment (within 14 days of the initial assessment if services are indicated) and to develop an individual plan of service within 45 days of the initial assessment. These assessments and service assignments, when indicated, are made according to the MDCH eligibility criteria and service selection guidelines. These criteria help to ensure consistent application across the region in eligibility determinations for all behavioral health, case management, and supports coordination services, using NorthCare’s Clinical Management Criteria outlined in the Utilization Management Plan. Once a level of care is determined for the individual, the NorthCare Benefit Plan is used to guide the selection of medically necessary services. The Northcare Access unit often handles calls from Medicaid recipients seeking services from another CMHSP other than their own Home Board. In these cases, the Access screener will first determine if the caller meets the eligibility criteria for CMHSP services. If the caller does meet the criteria, an appointment is scheduled with the Home Board, which is responsible for completing an initial assessment and an initial Plan of Service and making arrangements as appropriate with the other CMHSP. If an individual is reluctant to work with the Home Board, the Access staff may refer the individual to recipient rights or suggest the individual bring along an advocate to the initial assessment, or suggest the individual meet with a peer NORTHPOINTE BEHAVIORAL HEALTHCARE SYSTEMS POLICY TITLE: Access to Continuum of Services – Adults PAGE: 3 of 3 MANUAL: Clinical SECTION: Entry to Care ORIGINAL EFFECTIVE DATE: 10/2/95 BOARD APPROVAL DATE: 9/26/13 REVIEWED/REVISED ON DATE: 4/16/15 CURRENT EFFECTIVE DATE: 5/1/15 support specialist prior to the assessment, to ensure that the desires and concerns of the individual are expressed. Referrals to other community resources in lieu of specialty health services and supports are documented. If the individual is denied services, an appropriate referral and an Action notice is provided to the individual, which includes specific contact information and instructions on individual's rights to appeal or to request a second opinion. Staffs who are denying services must meet the criteria given in the definition section above. Action Notices are tracked for regional trending and patterns. Individuals seeking outpatient substance abuse services will be encouraged to initiate access directly at the outpatient Medicaid provider of their choice within the NorthCare provider network. The providers are listed in the NorthCare Customer Handbook. Co-occurring services will be available to individuals who meet the criteria for Specialty Mental Health services. When appropriate, an on-site visit to Northpointe programs may be provided to the person to be served/legal guardian. Exclusion Criteria: Northpointe maintains access to services in accordance with Michigan Department of Community Health (MDCH), NorthCare and accreditation standards. Individuals from out of state; individuals who request services we do not provide; and individuals (except HAB Waiver) who are rated as mild to moderate in severity of mental illness are referred to other appropriate community resources. Individuals must meet medical necessity and are transitioned to meet independent status as clinically indicated. Medicaid individuals from NorthCare service regions may obtain office based services at any CMH in the NorthCare Network. Individual calling for substance abuse services. Individuals seeking routine outpatient services are encouraged to initiate access directly with the outpatient provider of their choice or call Northcare Access. Individuals seeking intensive outpatient or residential treatment may access services by contacting the NorthCare Access