Lung Transplant
advertisement

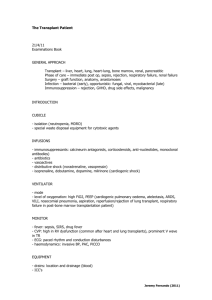
Lung Transplant Presentation 1 Sir, this patient has a bilateral lung transplant as evidenced by presence of a median sternotomy scar associated with normal underlying respiratory findings. The patient has a wrist tag indicating that he is a lung transplant patient. Chest excursion is normal with a normal percussion note, vesicular breath sounds and vocal resonance. Trachea is central and apex beat is not displaced. Hence there are no signs to suggest underlying rejection of the transplanted lung. Patient’s respiration rate is 14 bpm and there are no sign of respiratory distress or failure. Peripheral examination was normal. There was no evidence of nicotine staining, clubbing or short stature. Patient is not Cushingoid with no steroid purpura or thin skin to suggest chronic steroid use. There is also no hypertrichosis or gum hypertrophy to suggest cyclosporine adverse effects. In summary, this patient has bilateral lung transplant and is clinically well currently. The likely underlying causes a. Young patient – Cystic fibrosis, AAT, primary pulmonary hypertension, Eisenmenger (heart-lung transplant) b. Old patient – COPD, IPF and bronchiectasis (always bilateral) Presentation 2 Sir, this patient has a left lung transplant as evidenced by a left lateral thoracotomy scar with a tag indicating that he is a lung transplant patient. There is reduced chest excursion bilaterally with normal precussion note. Auscultatory findings include fine late inspiratory crepitations of the left hemithorax a/w normal vocal resonance, suggesting bronchiolitis obliterans syndrome post transplant. Trachea is central and apex beat is not displaced. There are complications of pulmonary hypertension, cor pulmonale ad polycythaemia. He is also in respiratory distress with a respiratory rate of 24 bpm with use of accessory muscles of respiration. Clinically he is in repsiratory failure and is oxygen dependent on INO2 2L/min; there is no central cyanosis and no signs of CO2 retention such as flapping tremors of the hands or a bounding pulse. In terms of aetiology: Examination of the right hemithorax showed presence of ILD/COPD with features of a. fine late inspiratory crepitations which are Velcro-like, clubbing b. prolonged expiratory phase with ronch and hyperresonance on percussion of the right hemithorax and loss of liver dullness, nicotine staining Steroid toxicity and cyclosporin toxicity. In summary, this patient has a left lung transplant for an underlying ILD. There are complications of pulmonary hypertension and cor pulmonale and is clinically in respiratory failure. There also signs to suggest bronchiolitis obliterans syndrome with signs of chronic steroid usage and cyclosporine usage. Questions What are the indications for lung transplant? Cardiopulmonary o Primary pulmonary hypertension o Eisenmenger’s (heart-lung transplant) Chronic Lung Conditions o Restrictive pulmonary disease - ILD o Obstructive pulmonary disease – COPD, AAT o Suppurative – Bronchiectasis (must be bilateral tplt), Cystic fibrosis o Sarcoidosis What are the contraindications for lung transplant? Disease specific guidelines Includes o Age o Comorbidities: Absence of concomitant disease that shortens life expectancy (HIV, Hep B) o Contraindications to surgery/GA (recent MI) o Smoking, alcoholic, poor social support What are the complications? Graft dysfunction (reperfusion edema in the first week) Airway complications – dehiscence, stenosis or bronchomalacia Rejection o Acute – lymphocytic inflammation, adjust steroid and immune suppression o Chronic – alloimmune inflammatory and non-alloimmune fibroproliferative; bronchiolitis obliterans syndrome Infection o CMV – ganciclovir o Aspergillus o Bacterial – pneumonia (Ps aeuroginosa) How would you manage? Multidisciplinary, regular follow up, transplant coordinator 3 drug maintenance o Calcineurin inhibitors (Cyclosporin or tacrolimus) o Purine synthesis antagonist ( AZA or MMF) o Steroid CMV and PCP prophylaxis