ECG Rhythm Interpretation Workbook
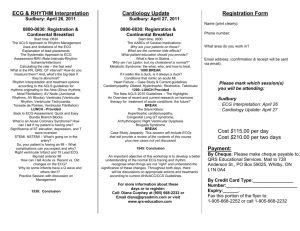
advertisement

Arrhythmia Interpretation Workbook for FY1 Doctor’s By Dr Christopher McAloon Introduction Learning Objectives On completion of this workbook and the session you should be able to: 1. Correctly recognise and action lifethreatening ECG’s. 2. Correctly analyse and interpret common tachy/bradyarrhythmias ECG’s. 3. Correctly recognise different types of tachyarrhythmias 4. Correctly recognise different types of Bradyarrhythmia’s What the workbook does not do? The workbook is designed to work through interpreting and recognising different ECG rhythm, not the entire 12 lead ECG. In clinical practice this is a continuum, but is beyond the purpose of the workbook. Purposely the book does not include ischaemic ECG’s. Contents 1. How to use this book 2. Reading rhythm strips 3. The Advanced Life Support (ALS)Approach 4. Life-threatening ECG’s 5. Tachyarrhythmia’s 6. Bradyarrhythmia’s 7. Continued Learning 8. Evaluation form 1. How to use this book The workbook will challenge you to interpret different rhythms in a systematic manner. The ECG’s will become more challenging as you become more confident in interpretation. Additional reading may be required to supplement your knowledge. The interactive key will guide you through successfully using the workbook. Interactive Key: Important Further reading required Exercise to be completed 2. Reading rhythm strips We all have our own system for reading 12 lead ECG’s. Take a moment to think about your system to reading ECG’s. Are there any limitations with your system? If you have a system that you are happy with please use it in the workbook. 3. The ALS Approach The ALS course teaches a very quick and easy six questions to be asked to interpret rhythms (not whole ECG’s): 1. Is there electrical activity? 2. What is the ventricular (QRS) rate? 3. Is the QRS rhythm regular or irregular? 4. Is the QRS complex width normal or prolonged? 5. Is there atrial activity present? 6. Is the atrial activity related to ventricular activity, if so how? Using the ALS Approach interpret this ECG. Figure 1. ECG gentleman fit and well. 1. Is there electrical activity? Yes / No 2. What is the ventricular (QRS) rate? QRS rate can be calculated many ways. One way is: One big square on the horizontal axis of an ECG is 0.2 seconds (5 big square is 1 second) Count the number QRS complexes in 6 seconds (30 large squares) Multiply by 10 = No beats/ minute 3. Is the QRS rhythm regular or irregular? Sometimes this is obvious from distance! Mark out the R waves on piece of paper; are the R wave intervals regular? 4. Is the QRS complex width normal (narrow) or prolonged (Broad)? Narrow less than 0.12 seconds/ 3 small squares Broad > greater than 0.12 sec/ 3 small squares 5. Is there atrial activity present? Yes/ No This question purely asks to look at the presence of P waves only. 6. Is the atrial activity related to ventricular activity, if so how? Look to see how / if at all the P wave is associated with the QRS complex Is the interval (PR) consistent with every P wave and following QRS? Is there any relationship at all? If so what? If not what is the atrial rate? What rhythm does Figure 1. ECG demonstrates? Figure 1 Interpretation 1. Is there electrical activity? Yes 2. What is the ventricular (QRS) rate? 50 beats per minute 3. Is the QRS rhythm regular or irregular? Regular 4. Is the QRS complex width normal or prolonged? Narrow 5. Is there atrial activity present? Yes 6. Is the atrial activity related to ventricular activity, if so how? Yes – Sinus Rhythm This is a narrow complex, sinus bradycardia, which is regular. 4. Life – Threatening Rhythms There are rhythms we must be able to recognise as doctors immediately. Firstly though before we even look at the ECG, we MUST look at the patient. Case 1. Man has an ECG Case 2. Man has an ECG Both Cases have the same ECG tracing, but which is the life threatening rhythm? Case 1 is caused by the Pneumatic drill and the trace is picking up the vibrations. Using the ALS Approach describe these rhythms: Are they life threatening? If it is would you shock the patient? Case 3. Collapsed man Case 4. Collapsed Woman. Case 5. Chest pain then collapse. Answers Case 3. No electrical activity activity, collapsed man. Asystole (check patient – leads could be disconnected!) Yes this is life threatening. Non-shockable. Case 4. Broad complex, Regular Tachycardia, No atrial activity. Concordant activity, regular. Supported if fusion/ capture beats. Ventricular Tachycardia Life-threatening rhythm, if clinically indicated patient needs to be shocked! Case 5. There is electrical activity, with irregular QRS complexes, tachycardia approx. 150-180 bpm, No atrial activity. Disconcordant QRS complexes Ventricular Fibrillation. Life threatening rhythm. Needs to be shocked. The following page supplements the Cardiac Arrest (life threatening rhythms) management, but further reading is required here. 5. Tachyarrhythmia’s Let’s get ourselves in the Tachy mood…. What do you know? What pulse rate defines tachycardia? What is a Narrow QRS complex? What is a Broad QRS complex? Can you think of rhythms that cause regular Narrow Complex Tachycardia’s? Can you think of rhythms that cause irregular Narrow Complex Tachycardia? Can you think of rhythms that cause Broad Complex Tachycardia? Tachyarrhythmias Tachycardia is > 100 bpm. All of us can increase our heart rate, for example when we exercise. This is physiological and is called Sinus Tachycardia. This is not an arrhythmia. There are other tachycardia’s which are caused by different rhythms, many of which are pathological. It can be very difficult to immediately diagnose as the ECG is going so fast. Using the ALS approach, we can interpret it first and then make a diagnosis. We broadly classify tachyarrhythmias first as Narrow or Broad (QRS duration). If it is broad in almost all occasions the tachycardia originates in the ventricles below the Bundle of His. We have already encountered these rhythms Ventricular Tachycardia/ Fibrillation. Rarely Broad Complex Tachycardia’s a can originate above the ventricle e.g. SVT with aberrancy – having a bundle branch block pattern. (this is beyond the remit of the book). Narrow Complex Tachycardia (NCT) originate from atrial myocardium or the AV junction. These are also called supraventricular tachycardia (SVT). These can be subclassified as regular or irregular. NCT Regular: Atrial Tachycardia, AV-Nodal-Re-entrantTachycardia (AVNRT), AV re-entry Tachycardia (AVRT), Atrial Flutter with fixed block. Sounds complicated, but management essentially the same! NCT Irregular: Atrial Fibrillation, Atrial Flutter with variable block. The following flow chart demonstrates management of SVT based on interpretation. Clinically you do not need to work out the exact cause for the arrhythmia, but what the rhythm is e.g. Regular NCT. The questions to ask are: 1. What is the patient like? (Are they stable?) 2. The ALS Approach questions What is you interpretation of these ECG’s? Are they stable clinically? What would you do next? Case 6. Young man with palpitations. Well. Case 7. Man well with dizziness. Stable. Case 8. Elderly patient with SOB. Stable. Case 9. Middle aged patient blacked out. BP 60/20. Answers Case 6. NCT regular at a rate of 150 bpm. No P waves. Patient stable – no indication for shock. Carotid sinus massage/ Valsava manoeuvre. Adenosine challenge (in no contraindication). Consider B Blocker Case 7. NCT regular, rate 150 bpm, 2 P waves to 1 QRS. Atrial Flutter 2:1. If uncertain: Patient stable – no indication for shock. Carotid sinus massage/ Valsava manoeuvre. Adenosine challenge (in no contraindication). Case 8. NCT irregular. Rate 150 bpm. No P waves seen. Atrial Fibrillation with fast ventricular response. Patient stable. Dependent patient, B-Blocker / Digoxin. Case 9. BCT, Rate 150 bpm. Ventricular Tachycardia likely. Patient unstable – But has a pulse. Not cardiac arrest yet! Indication for urgent shock. 5. Bradyarrhythmia’s Bradycardia is when the QRS rate is less than 60 bpm. Bradycardia can be physiological, for example during sleep, in athletes and as a response to certain medication (B Blocker). Pathological bradycardia can result from malfunction of the SA node or from partial/ complete failure of atrioventricular conduction. This may require a pacemaker. Bradyarrthymias can be life threatening and can proceed Cardiac arrest. There are different Bradyarrthymias; the majority are referred to as heart block, which refer to partial or complete blockage of the AV conduction. Type 1 Heart block Consistent prolongation PR interval (>0.2 seconds), can be physiological Type 2 Heart block Mobitz Type 1 prolongation after each successive P wave, until a drop beat Mobitz Type 2 Intermittent non-coducted P waves without prolongation. Can result 2:1, 3:1 block Complete Heart Block No association between P waves and QRS complexes. QRS can be Broad. Malfunction of the SA node as in sick sinus syndrome can lead to ‘junction rhythms’ or ‘escape rhythms’. Atrial Fibrillation may also present as ‘slow AF’. And this may or may not be related to rate limiting medication. We will not explore this any further and focus on the Heart Blocks, but it is worth being aware of them. Using the ALS approach to rhythm Interpretation, decide which heart block is demonstrated in the ECG’s shown Case 10. Case 11. Case 12. Answers Case 10. Bradycardia at 50bpm, narrow complexes, regular (no drop beats). There are P waves and they are associated with the QRS complexes. There are 2 P waves to each QRS complex. Type 2 Heart Block with a 2:1 block. Case 11. Bradycardia at 60 bpm. Narrow complexes, regular (no drop beats). Atrial activity present. One P wave to one QRS complex. PR interval prolonged on consistent interval. Type 1 Heart Block. Case 12. This is a difficult ECG. The QRS intervals have a rate of 50bpm. The QRS complexes are regular. The QRS complexes are Broad. Initially the P waves seem to have varying prolongation to the QRS complexes. Could it be Type 2 Heart Block (Mobitz 1)? No, the P waves are regular and not conducting to the ventricles. The other clue is the QRS width is Broad. Complete Heart Block. Management of Bradycardia depends if the patient is stable. This algorithm details how to evaluate Bradyarrthymias in terms of acute management. 6. Continued Learning I hope you enjoyed using this workbook and you feel more confident interpreting rhythms in the clinical setting. The key to developing confidence is to keep practicing looking at different rhythms. A reference list is available at the end of the book for further reading. Please complete the evaluation to allow us to assess the usefulness of the workbook and what could be done to improve it in the future. 7. Evaluation Please could you take a minute to complete the evaluation? The form is completely anonymous, please be honest. 1, What trainee level are you? 2, What specialities have you performed rotations? For each statement please circle a rating and please add any addition comments. 3, The ‘Emergency Rhythm Interpretation’ Workbook was relevant to my clinical practice. 1 – Strongly Agree; 2-agree; 3 – neutral; 4-disagree; 5strongly disagree 4, The ‘Emergency Rhythm Interpretation’ Workbook was helpful to my clinical practice. 1 – Strongly Agree; 2-agree; 3 – neutral; 4-disagree; 5strongly disagree 4, I now feel more confident recognising and interpreting life threatening rhythms. 1 – Strongly Agree; 2-agree; 3 – neutral; 4-disagree; 5strongly disagree 5, I now feel more confident recognising and interpreting tachyarrhythmia’s 1 – Strongly Agree; 2-agree; 3 – neutral; 4-disagree; 5strongly disagree 6. 6, I now feel more confident recognising and interpreting Bradyarrhythmia’s 1 – Strongly Agree; 2-agree; 3 – neutral; 4-disagree; 5strongly disagree 7, I will use the ALS approach to interpreting rhythms in my own clinical practice. 1 – Strongly Agree; 2-agree; 3 – neutral; 4-disagree; 5strongly disagree 8, The information in the workbook was pitched at the right level. 1 – Strongly Agree; 2-agree; 3 – neutral; 4-disagree; 5strongly disagree 9, The ‘Emergency Rhythm Interpretation’ Workbook was easy to use. 1 – Strongly Agree; 2-agree; 3 – neutral; 4-disagree; 5strongly disagree 10, What would you do to improve the workbook? 11, Would you recommend the workbook to a friend? References 1, Resuscitation Council (UK) Cardiac monitoring, electrocardiography, and rhythm recognition. Advanced Life Support. Sixth edition. Kent: TT Litho Printers, pp71-88 2, Deakin CD, Nolan JP, Soar J, Sunde K, Koster R, Smith GB, Perkins GD. 2010. European Resuscitation Council Guidelines for Resuscitation 2010 Section 4. Adult Advanced Life Support. Resuscitation. 81 (2010); pp.1305 - 1352