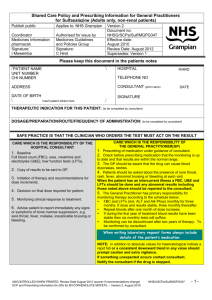
(adults only, non-renal patients).
advertisement
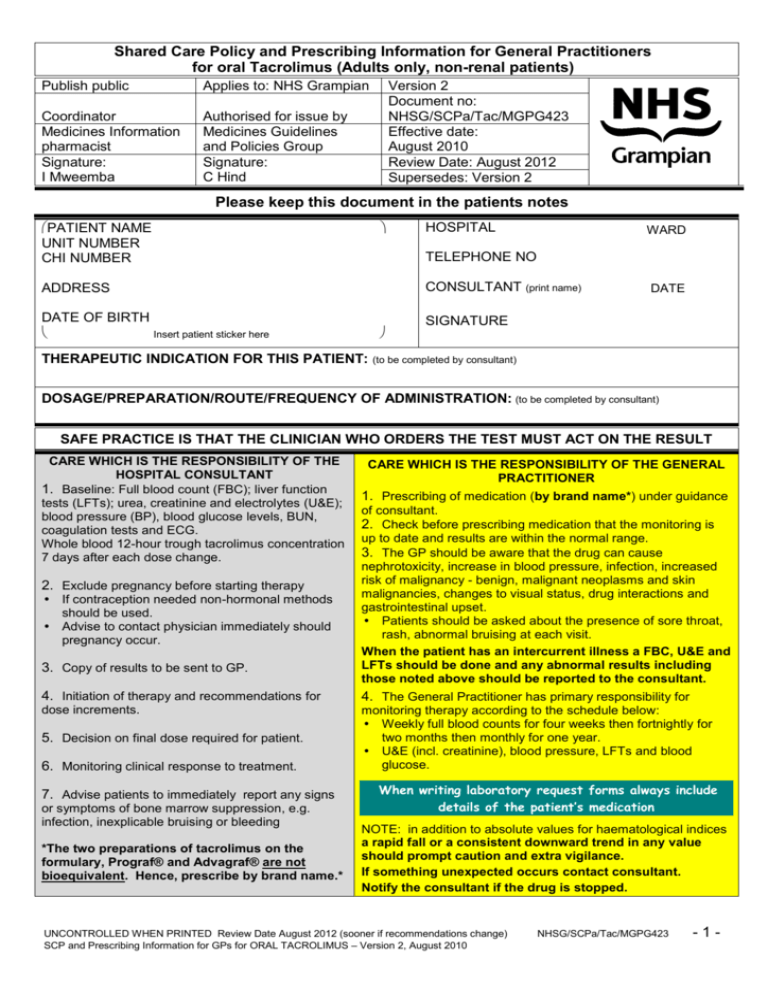
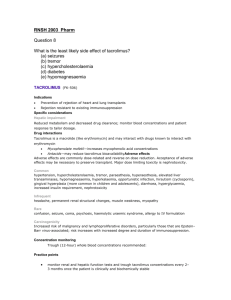
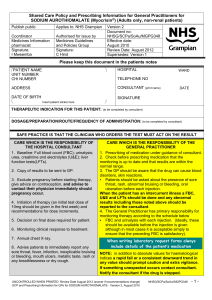
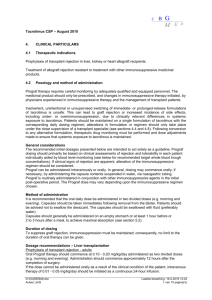
Shared Care Policy and Prescribing Information for General Practitioners for oral Tacrolimus (Adults only, non-renal patients) Publish public Applies to: NHS Grampian Coordinator Medicines Information pharmacist Signature: I Mweemba Authorised for issue by Medicines Guidelines and Policies Group Signature: C Hind Version 2 Document no: NHSG/SCPa/Tac/MGPG423 Effective date: August 2010 Review Date: August 2012 Supersedes: Version 2 Please keep this document in the patients notes PATIENT NAME UNIT NUMBER CHI NUMBER HOSPITAL WARD TELEPHONE NO CONSULTANT (print name) ADDRESS DATE OF BIRTH Insert patient sticker here THERAPEUTIC INDICATION FOR THIS PATIENT: DATE SIGNATURE (to be completed by consultant) DOSAGE/PREPARATION/ROUTE/FREQUENCY OF ADMINISTRATION: (to be completed by consultant) SAFE PRACTICE IS THAT THE CLINICIAN WHO ORDERS THE TEST MUST ACT ON THE RESULT CARE WHICH IS THE RESPONSIBILITY OF THE HOSPITAL CONSULTANT 1. Baseline: Full blood count (FBC); liver function tests (LFTs); urea, creatinine and electrolytes (U&E); blood pressure (BP), blood glucose levels, BUN, coagulation tests and ECG. Whole blood 12-hour trough tacrolimus concentration 7 days after each dose change. 2. Exclude pregnancy before starting therapy If contraception needed non-hormonal methods should be used. Advise to contact physician immediately should pregnancy occur. 3. Copy of results to be sent to GP. CARE WHICH IS THE RESPONSIBILITY OF THE GENERAL PRACTITIONER 1. Prescribing of medication (by brand name*) under guidance of consultant. 2. Check before prescribing medication that the monitoring is up to date and results are within the normal range. 3. The GP should be aware that the drug can cause nephrotoxicity, increase in blood pressure, infection, increased risk of malignancy - benign, malignant neoplasms and skin malignancies, changes to visual status, drug interactions and gastrointestinal upset. Patients should be asked about the presence of sore throat, rash, abnormal bruising at each visit. When the patient has an intercurrent illness a FBC, U&E and LFTs should be done and any abnormal results including those noted above should be reported to the consultant. 4. Initiation of therapy and recommendations for 4. The General Practitioner has primary responsibility for dose increments. monitoring therapy according to the schedule below: Weekly full blood counts for four weeks then fortnightly for two months then monthly for one year. U&E (incl. creatinine), blood pressure, LFTs and blood glucose. 5. Decision on final dose required for patient. 6. Monitoring clinical response to treatment. 7. Advise patients to immediately report any signs or symptoms of bone marrow suppression, e.g. infection, inexplicable bruising or bleeding *The two preparations of tacrolimus on the formulary, Prograf® and Advagraf® are not bioequivalent. Hence, prescribe by brand name.* When writing laboratory request forms always include details of the patient’s medication NOTE: in addition to absolute values for haematological indices a rapid fall or a consistent downward trend in any value should prompt caution and extra vigilance. If something unexpected occurs contact consultant. Notify the consultant if the drug is stopped. UNCONTROLLED WHEN PRINTED Review Date August 2012 (sooner if recommendations change) SCP and Prescribing Information for GPs for ORAL TACROLIMUS – Version 2, August 2010 NHSG/SCPa/Tac/MGPG423 -1- Shared Care Policy and Prescribing Information for General Practitioners for oral Tacrolimus (Adults only, non-renal patients) ABNORMAL MONITORING RESULT ACTION TO BE TAKEN WBC <4.0 x 109/L Withhold until discussed with consultant Neutrophils <2.0 x 10 /L Withhold until discussed with consultant Platelets <150 x 10 /L Withhold until discussed with consultant Potassium >5.0mmol/L Withhold until discussed with consultant Creatinine rises ≥30% from baseline Discuss with consultant >2-fold rise in ALT or Alk Phos (from upper limit of reference range) Withhold until discussed with consultant 9 9 For specific product information please consult the current summary of product characteristics (http://emc.medicines.org.uk/) and the BNF (http://www.bnf.org/bnf/) Other information Live vaccines should be avoided in patients taking tacrolimus. Single pneumococcal vaccination and annual influenza vaccine should be given. Tacrolimus capsules should be swallowed whole with plenty fluid, preferably on an empty stomach at least one hour before or 2-3 hours after a meal. There are a number of drug interactions that must be considered when a new drug is prescribed please refer to Summary of Product Characteristics, BNF or contact Medicines Information. Some important interactions to consider include the following: Do not give with ciclosporin due to increased risk of nephrotoxicity. Grapefruit and grapefruit juice should not be taken at the same time as tacrolimus. Potassium sparing diuretics and potassium salts should be used with caution due to hyperkalaemia. Significantly increased tacrolimus blood levels have been noted with the following drugs that inhibit CYP3A4 – ketoconazole, fluconazole, itraconazole, voriconazole, erythromycin and HIV Protease inhibitors. Caution also advised with weaker CYP3A4 inhibitors, e.g. omeprazole and nifedipine. Inducers of CYP3A4 shown to decrease the blood levels of tacrolimus – rifampicin, phenytoin, phenobarbitone and St John’s Wort. Methylprednisolone has been reported to increase and decrease tacrolimus plasma levels. Enhanced nephrotoxicity has been observed, following the administration of either of the following drugs in conjunction with tacrolimus – amphotericin B or Ibuprofen. As tacrolimus may alter the metabolism of steroid-based contraceptive agents, particular care should be exercised when deciding upon contraceptive measures. Pregnancy Discuss with consultant. Contra-indicated in pregnancy. Effective contraception required during treatment, tacrolimus capsules alter the metabolism of oral contraceptives, non-hormonal methods should be used. Advise to contact their physician immediately should pregnancy occur. Breast-feeding Discuss with Aberdeen Maternity Hospital. Manufacturer advises avoid. Responsibilities of GPs undertaking monitoring A GP agreeing to monitor tacrolimus should: Ensure that the relevant monitoring requirements are undertaken at the correct frequency. Ensure that the test results are checked for any abnormality as soon as the results are available. Ensure abnormal results are acted upon. Only continue to prescribe tacrolimus if it is being satisfactorily monitored. Contact the consultant in the event of a drug reaction or monitoring abnormality or anything you are unhappy about. Be alert for any of the known adverse reactions. ** The patient should be encouraged to ensure blood tests are taken at the correct intervals. ** UNCONTROLLED WHEN PRINTED Review Date August 2012 (sooner if recommendations change) SCP and Prescribing Information for GPs for ORAL TACROLIMUS – Version 2, August 2010 NHSG/SCPa/Tac/MGPG423 -2-