The clinical evaluation of the Datex Ohmeda GE S/5 Monitor`s Non
advertisement

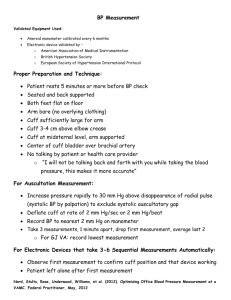
The clinical evaluation of the Datex Ohmeda GE S/5 Monitor’s Non Invasive Blood pressure (E-PRESTN) module and the optimal placement of measurement cuff on the anaesthetized dog. Drs. R.C. Wienesen Student-number: 0356972 October 2008 - March 2009 Supervisors Division Anaesthesiology, Dept Clinical Sciences of Companion Animals, FVM, UU R. Sap Drs. L.C. Akkerdaas Contents Abstract 3 Introduction 4 Invasive Arterial Blood Pressure measurement 4 Non Invasive methods 5 Goals of this study 7 Materials and Methods 8 Results 10 Discussion 15 Conclusions 17 Clinical relevance 18 Acknowledgements 19 Appendix 20 References 25 2 Abstract Objective 1 To evaluate the Datex Ohmeda GE S/5 Non Invasive Blood Pressure module in comparison to the standard invasive arterial blood pressure (IABP) technique in anaesthetized dogs. Objective 2 To determine optimal cuff position and site for the noninvasive system on the patient. Objective 3 To assess the effect of different anesthetic protocols (methadone-isoflurane, dexmedetomidine-propofol and dexmedetomidine-alfaxalone) on the performance of the Datex Ohmeda GE S/5. Study design A prospective study. Animals. Thirty-two client owned dogs undergoing a variety of surgical procedures. Methods Three different anesthetic protocols were used. Invasive blood pressure was measured using either the femoral or dorsal pedal artery. For oscillometric noninvasive blood pressure (ONIBP) measurement, the cuff was placed at the contra lateral limb during the surgical procedure when possible, otherwise the tail base was used. Recordings were made pre-, per- and post operative. The tail base and front limb O-NIBP measurements were continued post operatively. Statistical analysis of the Invasive Arterial Blood Pressure (IABP) and O-NIBP data was performed using a (modified, percentual) Bland Altman analysis. An ANOVA was used to compare the different protocols. Result 1 The Datex Ohmeda GE S/5 O-NIBP produced highly variable results for all blood pressure measurements. The least variable results came from the Mean Arterial Pressure (MAP) for all measurement-sites. Result 2 The most reliable site for O-NIBP measurements is the tail base followed by the hind limb. The front limb is less accurate. Result 3 The number of failures in order to obtain a direct reading in the Datex O-NIBP were higher in the dexmedetomidine protocols. Bias itself did not differ between the protocols. Conclusion 1 & 2 The most accurate data produced by the Datex O-NIBP was the MAP. The optimal site for cuff placement was the tail base. However, due to the high variability of all values it is difficult to determine whether the machine is producing accurate (e.g. unbiased) results. It should be noted that trend information (multiple consecutive measurements) gathered with the Datex O-NIBP can be useful. However sudden drops or increases of O-NIBP do not necessarily indicate that the anesthesia is insufficient, as it could also be accounted for by the variability of the O-NIBP. Conclusions 3 Anesthetic protocols do influences the number of failures to provide direct measurement. This is most likely related to the use of dexmedetomidine (a2-agonist) which causes vasoconstriction. This vasoconstriction is the likely culprit for the increased failure to provide direct measurements with the Datex O-NIBP. Clinical relevance The Datex Ohmeda GE S/5 can not be used on patients that need accurate blood pressure monitoring because of high anesthetic risks (ASA-III or up). In cases where placement of the arterial catheter-system for the IABP fails and patients in ASA-I and ASA-II (where protocols usually don’t include measurement of the arterial blood pressure (ABP)) it can be used to get information on the arterial blood pressure trend. In these before mentioned situations, the MAP is shown to be the most reliable. Keywords anesthesia, arterial blood pressure, dog, non invasive blood pressure, oscillometric, measurement site. 3 Introduction The Arterial Blood Pressure (ABP) is the most direct measurable cardiovascular parameter to provide insight in the tissue perfusion. Directly dependant on the afterload of the heart, it is commonly used as an indicator for the workload of the heart, and as such the cardiac performance. At tissue level the ABP, the oscillations between systolic blood blood pressure (SAP) and diastolic blood pressure (DAP) are dampened [Sharnvet, 2008][Deflandre, C.J.A., 2008][Wagner, A.E., 1997]. This dampening means that tissue perfusion is largely dependant upon the average pressure in the cardiovascular system. The determining factor is called the Mean Arterial Blood Pressure or MAP and is relevant for virtually every tissue in the body. One exception to the MAP being important in tissue perfusion is the heart itself. During the systolic phase of the heart action the blood flow is limited because the small vessels are compressed. As such the tissues get their share of oxygen and nutrients during the diastolic phase. Because of this fluctuating availability of oxygen in the cardiac muscle, the DAP needs monitoring as well [Sharnvet, 2008]. Blood pressure measurement (arterial and venous) is rarely preformed in the veterinary practice. Equipment is expensive and measurement methods are usually time consuming. However one of the common complications of anesthesia is hypotension (MAP < 70 mmHg), in both human and veterinary patients [Wagner, A.E., 1997]. As early as in 1897, when Hill and Barnard experimented with chloroform anesthesia, it was well known chloroform caused a significant drop in ABP. In human medicine/anesthesia the ABP monitoring is part of basic monitoring and the American College of Veterinary Anesthesiology published a similar set of guidelines in 1995 [Anonymous., (2005)][Birks S.H., (2007)]. These included the monitoring of the ABP for both canine and feline patients with an ASA status (table 1) of III or higher and for equine patients undergoing general anesthesia. Table 1: ASA-classification system modified for veterinary use Classification Implication for the patient’s status ASA I A normal healthy patient ASA II A patient with mild systemic disease but no expected functional consequences ASA III A patient with severe systemic disease with clear functional consequence ASA IV A patient with severe systemic disease that is a constant threat to it’s life ASA V A moribund patient who is not expected to survive without the operation Invasive Arterial Blood Pressure measurement The golden standard for blood pressure measurement at the moment is the direct (or invasive) arterial blood pressure measurement (IABP) and is accurate even in hypo- or hypertensive patients [Billiet, E., 1998]. It is based upon a fluid filled catheter system which is connected to a pressure transducer [Deflandre, C.J.A., 2008]. The catheter system is filled with a NaClLow dose Heparin Solution (2500 IE of Heparin in 500 mL NaCl 0.9%). The catheter is placed on the femoral artery (central), or the dorsal metatarsal artery (peripheral) depending on the patient’s size and hemorrhage risk. Currently this is the only method capable of providing a continuous measurement of the arterial blood pressure. The invasive method has, however, several disadvantages. For example, the placement of arterial catheters is challenging in small dogs and in feline patients. There is a slight risk for complications such as arterial hemorrhage, infection, septicaemia and partial or complete occlusion of the artery. Occlusion (e.g. arterial embolisation) is potentially followed by ischemia of the tissue distal of the catheter it theoretically could result in loss of a toe or other extremity [Deflandre, C.J.A., 2008] [Gains, M.J., 1995]. Besides the risks to the patient’s health, the system is susceptible to outside influences. The catheter is difficult to fixate to the patient, leading to dislocation especially when patients are moved around. The IABP-system is also sensitive to gravity. If the transducer is not placed at the correct height (equal to the height of the right atrium in any position) this can lead to under- or 4 overestimation of the ABP. Another factor resulting in over- or underestimation are air bubbles in the fluid column. These air bubbles create a dampening effect because they are compressed with the fluctuations in the blood pressure [Deflandre, C.J.A., 2008]. Non Invasive methods Over the years several methods have been developed to assess the cardiovascular system functioning and some are very useful in determining the MAP. Palpation of the peripheral pulse for example does not yield any additional information on the arterial blood pressure other than that there is a pressure wave traveling through the vascular bed. Similarly, determination of the heart rate gives no information about the current arterial blood pressure [Chalifoux A., 1985][Wagner, A.E., 1997]. In human medicine the use of a stethoscope and sphygmomanometer with attached cuff for determining the ABP, was common practice up until the introduction of digital equipment. The latter method, which is the basis for many of the Non Invasive Blood Pressure (NIBP) measurement methods nowadays, is largely dependant on the quality of hearing of the (general) practitioner (G.P.) [Chalifoux A., 1985][Wagner, A.E., 1997]. First the cuff is placed and inflated far above the SAP for any patient. While the G.P. listens with his stethoscope on the brachial artery, the cuff is slowly deflated. Eventually the pressure drops below the SAP. When this happens a turbulent blood flow occurs. This turbulent blood flow produces a distinctive sound know as Korotkoff-sounds, named after the person who discovered it. As soon as the cuff pressure falls below the DAP the blood flow becomes unimpeded and the Korotkoff-sounds disappear [Chalifoux A., 1985]. The Korotkoff -sounds are however virtually impossible to hear, even for the best trained cardiologist, in canine and feline patients and as such the method is completely useless in small animal medicine [Chalifoux A., 1985][Mandigers P., 2005][Wagner, A.E., 1997]. Figure 1 The principle behind the non invasive blood pressure measurement. Cuff is inflated above the 120 mmHg (B) and than lowered (line between B and C) as pressure decreases the pressure waves pass underneath the cuff resulting in either Korotkoff sounds, Doppler-Audio output or pressure oscillations. These disappear when the line B-C falls below the 80 mmHg. (humane) [Berne, R.M., 2004]. In veterinary medicine there are currently two non-invasive techniques in use. The Non Invasive Doppler flow-ultrasonography (NDFU-NIBP) and the Non Invasive Oscillometric Spygmomamometry (O-NIBP). Figure 1 shows the basic principle of all non invasive methods [Deflandre, C.J.A., 2008][Mandigers, P., 2005][Nelson, R.W., 2003] . The NDFU-NIBP system is based on a comparable principle as the sphyngomanometric method but instead of a stethoscope, an ultrasound transducer is used to determine when the blood starts to flow again. It will create an audio signal as soon as the cuff pressure falls below the SAP. DAP and the related MAP can not be determined reliably with this system because it is difficult to determine when the blood flow becomes unimpeded by the cuff [Mandigers P., 2005][Nelson, R.W., 2003]. As a result the Doppler Ultrasonography is an unreliable system for determining hypotension. The ultrasound-transducer needs to be moved underneath the cloths of the sterile field, a region that is difficult to access for any anesthesiologist under normal circumstances. As such the NDFU-NIBP has no place in the operating theater. Next to this surgical problem it has also been determined that the NDFU-NIBP is more accurate at higher blood pressures The NDFU-NIBP system can however be used reliable in animals suspected of systolic hypertension. Since cats are 5 known to suffer from idiopathic high arterial blood pressure this method is especially useful in these cases [Mandigers, P., 2005]. Non Invasive Oscillometric Spygmomamometry (O-NIBP) once again uses the same principle as the before mentioned auditory and Doppler-Ultrasonographic methods. It uses a cuff that is inflated and deflated in cycles. The machine however detects small oscillations in the pressure of the cuff during the phase that the cuff is below SAP and above DAP [Nelson, R.W., 2003]. The maximum reading is equal to the MAP and from that point an algorithm calculates the SAP and DAP [Valerio, F., 2006]. Several O-NIBP devices have been tested over the years with variable results. Some were capable of delivering accurate readings while others underestimated pressures [Deflandre, C.J.A., 2008][Sawyer, D.C., 1994][Meurs K.M., 1996]. The cuff can be placed on three sites on the patient, the tail base (medial sacral artery – medial caudal artery), the hind limb (dorsal pedal artery) or the front limb (palmar arches of the median artery). Several authors point out that the most reliable place for O-NIBP measuring in dogs is the tail base followed by the hind limb’s metatarsal region [Mandigers, P., 2005][Habermann, C.E., 2006][Sawyer, D.C., 2004]. It needs to be noted that, although anesthesia should prevent any active movement, the site should always be selected on basis of movement. It has been demonstrated (in conscious dogs) that the cuff can best be placed on the tail base when the patient is awake, primarily because cuff placement on the other measurement sites (metacarpal and/or hock) can lead a preoccupation with removing the cuff from its extremity. This results in more movement and as such less reliable data collection. Shivering should be avoided for the same reason [Grosenbaugh, D.A., 1998]. For the O-NIBP, clipping the area of cuff-placement is unnecessary, although longhaired breeds can prove to be a challenge. The long fur can obstruct the use of the Velcro used on most cuffs [Mandigers, P., 2005][Bodey, A.R.,1994]. Another factor in reliability is the size of the cuff. In 1980 Geddes et al. demonstrated that a cuff: circumference ratio of about 0,40 (or 40%) in dogs front limb produced the best results. Selection of the wrong cuff can lead to under- or overestimation. The research of Geddes et al. registered the MAP via an IABP system and the pressure in the balloon inside the cuffs. This in conjunction with a registration of the oscillations in the balloon resulted in the advise to use a cuff: circumference ratio of 0,40 or 40% [Geddes, L.A., 1980]. The manufacturer of the cuffs used in this experiment also recommends such a ratio. A major concern is the algorithm used by the machine especially when the O-NIBP is determined via a machine originally designed for human medicine. The algorithm itself could be unsuitable for veterinary use however this has yet to be determined [Valerio F., 2006]. 6 Goals of this study The objectives of this study are based upon the current use of the Datex Ohmeda GE S/5 O-NIBP module in the surgical facilities of the department of Clinical Sciences of Companion Animals at the faculty of Veterinary Medicine, University of Utrecht, Utrecht, the Netherlands. Since it is currently used without any form of verification as to the reliability of the device, it remains difficult to determine whether or not critical decisions in patient care can be made on basis of data generated by this system. Hence the first objective of this study is to compare the Datex Ohmeda GE S/5 ONIBP and the golden standard (IABP) to determine its reliable and to determine whether it provides comparable and accurate data in patients during general anesthesia, before and during surgery. The corresponding hypotheses is “The oscillometric Arterial blood Pressure device is only reliable at values equal or lower then normotension in comparison to the IABP”. The second objective is to determine the optimal site for cuff placement for the Datex Ohmeda GE S/5 on the patient. Corresponding hypothesis “The optimal site for cuff placement is the tail base”. After writing the research proposal it became clear that this study would be carried out in conjunction with a study in to the anesthetic effect of dexmedetomidine and alfaxalone. As such it became possible to look at the differences in the performance of the Datex Ohmeda GE S/5 in the different anesthetic protocols (methadone-isoflurane, dexmedetomidine-propofol and dexmedetomidine-alfaxalone). This became the third objective of the study. 7 Materials and methods Thirty-one canine patients of various breeds, weighing 32.0 +/- 14.8 kg (mean, SD) were used for this study. All the dogs were scheduled for general anaesthesia and would either need an arterial catheter for monitoring there blood pressure or they took part in another study protocol (in this case the recently registered anaesthetic agent alfaxalone (alfaxalone 10 mg/mL solution, Alfaxan®, Vétoquinol Buckingham England) for which an arterial catheter was also required to collect arterial blood pressure data. The average age of the dogs was 4,5 years, with a variation of 1,5 months to over ten years of age. The ASA classifications ranged from I to IV. Sixteen dogs were classified as ASA-I, six in ASAII, six in ASA-III and three in the ASA-IV. There were no exclusion criteria based upon gender or breed. Size was limiting factor since the smallest cuff could fit an extremity of 3 centimetres circumference or up and the largest cuff could only fit an extremity of up to fifteen centimetres circumference. No exclusion is made based up on the premedication and anaesthetic protocols used on the patients. Commonly used protocols included dexmedetomide-alfaxalone (9), dexmedetomidinepropofol (9), methadone-midazolam-isoflurane (12). In one case sevoflurane was used in stead of isoflurane in the methadone protocol. All of the dexmedetomidine patients were classified as ASA-I and ASA-II. All patients were intubated and the arterial catheter (Abbocath-T, 22 SWG, 32 mm, Abbot, Sligo, Republic of Ireland), arterial cannula with flow switch, (20 SWG, 45 mm, Braun Dickinson, Swindon, UK or Secalon T over the needle central venous catheter with flow switch, 18 SWG, 90 mm, Braun Dickinson Critical Care Systems Pte Ltd, Singapore) was placed either at the hock (dorsal pedal artery, peripherally) or in the thigh (femoral artery, centrally) depending on the preferences of the staff and on whether the animal participated in the alfaxalone-study (dorsal pedal artery only). The catheter is placed by an anesthesiologist or nurse anesthetist to ensure proper and rapid placement. After placing the catheter is flushed using a 2500 IE heparin/0.9% and then fixed to the patient. In the operating room (OR) the arterial catheter is connected to a disposable transducer (Gabarith TM single transducer set, Braun Dickinson Infusion Therapy Systems Inc, Sandy, UT, USA) which is positioned at the height of the right atrium. The transducer is connected to the Datex Ohmeda GE S/5 monitor and micro flushed continuously using a prepared 2500 IE heparin/0.9% saline. To ensure proper micro flush function this solution is pressurized to approximately 300 mmHg to prevent backflow of blood into the catheter-transducer system. The IABP- system is then is zeroed to the ambient air pressure in the OR. To determine the correct cuff-size for measuring the NIBP the circumference (in centimeters) of the extremity is determined. Based on this measurement the appropriate cuff (Critikon Neonatal soft cuffs, sizes 1 to 5 for DINAMAP available) size is chosen. Manufacturer’s recommendations for human use were taken into account in selecting the appropriate cuff size (e.g. the circumference of the measurement-site had to correspond with the manufacturer’s circumference recommendations on the cuffs). Cuffs are placed on three different places. Before and during the surgery the preferred location is the contra lateral hind limb just below the hock (metatarsal region, 22 patients). If placement is impossible because due to the surgical procedure undertaken in that region, the cuff is placed at the tail base (9 patients). When the cuffs were placed they were connected to the Datex Ohmeda GE S/5 using the infant cuff connector system. After placement, the O-NIBP system was tested to see if the selected location delivered viable data, if not the cuff was repositioned on the same site (two times maximum) and tested again. When it was possible to reach the tail base, the cuff was then moved to this position and the procedure of placement and testing was repeated. If positioning of the cuff was no longer possible due to lack of time (start of the surgery was imminent) the patient was considered lost to this study. A total of 5 consecutive measurements are recorded before the start of the surgical procedure. This is repeated during surgery at intervals of 2,5 minutes minimum and a maximum of 10 minutes. After surgery the cuff is moved to the two other measuring locations to make three consecutive measurements at each site. 8 Data is recorded by hand on a hard copy excel data-sheet and the IBP (continuous measurement) in the following sequence: heart rate, invasive blood pressures (SAP, DAP, MAP) and last O-NIBP pressures. This was done to get the best accuracy since the heart rate and invasive pressures were continuous readings. After completion of the measurements a printer was connected to the Datex monitor to print out the numerical trend sheet (displaying IBP, NIBP and HR at any time, per minute, during surgery). The hand written data then function as a back-up. Statistical analysis was performed using the Bland Altman method to compare two machines for a parameter [Bland, J.M., 1986]. It is slightly modified to a percentual bias of the O-NIBP measurement compared to the IBP. Also the different protocols will be compared and the different measurement sites using an ANOVA and scatter plots respectively [Petrie, A., 1999]. 9 Results Table 2 shows the different arterial blood pressures found in the two premedication-groups measured during the pre-operative phase. The mean SAP, DAP and MAP in the dexmedetomidine groups was significantly higher than in the methadone group. Table 2: Average SAP, DAP and MAP, based upon data from the IABP (for all groups 0.02 < P < 0.05). Premedication In the protocol Patients (N) SAP (mmHg) (mean +/- Sd) DAP (mmHg) (mean +/- Sd) MAP (mmHg) (mean +/- Sd) Methadone 13 97 +/- 18 52 +/- 13 66+/- 14 Dexmedetomidine 18 149 +/- 19 88 +/- 11 104 +/- 18 The first time failure rate (FFR) (total and divided on basis of the anesthetic protocol) I presented in Table 3. The first time failure rate is the calculated using the formula rate (%) = (x/n)*100%. The FFR is technically the number of measurements in which the O-NIBP device failed to provide an instant measurement. In the protocols were dexmedetomidine was used as premedicant, the failure rates were higher compared to methadone (dexmedetomidine, average FFR of 31,8% versus 8,5% in the methadone groups). Table 3: First time failure rate divided on basis of the protocol and overall Protocol Patients (N) Total number of measurements (n) Number of failures (x) FFR (%) MethadoneIsoflurane 12 183 14 7 MethadoneSevoflurane 1 16 3 19 DexmedetomidinePropofol 9 132 49 37 DexmedetomidineAlfaxalone 9 132 35 26 Overall 31 463 103 22 In table 4 the standard deviations (Sd) and corresponding P-values are given for each measuresite and bloodpressure parameter. The standard deviations of the NIBP values are all higher, although the difference is only significant if the value of P is below 0.05. In other words there is more variation. The tail base gives the least variable results (Sd NIBP is the lowest) in this case and the variation (Sd) is higher during surgical stimulation. The MAP appears to be the best (accurate) of the blood pressure determinants (P≤0,02). Displayed in figure 2 a-c are the Bland-Altman, or difference plots for SAP, DAP and MAP from the hind limb, taken pre surgically. These graphically display what can be found with the Bland-Altmann method for comparing two different measurement-methods. The identity (thin, grey line) is equal to zero bias (e.g. methods do not differ). The bias is the average difference (thick, blue line) and the 95% limits of agreement are the limits in which 95% of the bias-point can be found (thick, interrupted, light blue line). The 95% CI lines are the 95% confidence intervals (thin, dotted, light blue lines). If a line would be drawn through the dot-clouds it would give a >-shaped line with the point of the > in the direction of the higher blood pressures. This >- shape is visible in the SAP and MAP scatter plots and means that the higher the ABP the smaller the Bias gets. 10 Difference Plot Difference (gemSAP-NIBPpreAP - gemSAP-IBPpre AP) / Mean of All 50% Identity 40% Bias (-2.5%) 30% 95% CI 20% 95% Limits of agreement (-35.6% to 30.6%) 10% 95% CI 0% -10% -20% -30% -40% -50% 40 60 80 100 120 140 160 180 200 Mean of All Figure 2a: SAP difference plot for the O-NIBP (pre-surgical stimulation) at the hind limb. Difference Plot Difference (gemDAP-NIBPpreAP - gemDAP-IBPpreAP) / Mean of All 60% Identity 40% Bias (-26.7%) 20% 95% CI 0% 95% Limits of agreement (-78.6% to 25.2%) 95% CI -20% -40% -60% -80% -100% 20 40 60 80 100 Mean of All Figure 2b: DAP difference plot for the O-NIBP (pre-surgical stimulation) at the hind limb. 11 Difference Plot Difference (gemMAP-NIBPpreAP - gemMAP-IBPpreAP) / Mean of All 50% Identity 40% Bias (0.5%) 30% 95% CI 20% 95% Limits of agreement (-35.4% to 36.3%) 10% 95% CI 0% -10% -20% -30% -40% -50% 40 60 80 100 120 140 Mean of All Figure 2c: MAP difference plot for the O-NIBP (pre-surgical stimulation) at the hind limb. Scatter Plot with Fit 220 Linear fit (15.88 +0.8513x) 200 95% CI 180 95% Prediction interval gemSAP-NIBPpreAP 160 140 120 100 80 60 40 20 60 80 100 120 140 160 180 200 gemSAP-IBPpre AP Figure 3: SAP scatter plot of the IBP (x-axis) versus the NIBP (y-axis). Further data is presented in table 5. 12 As mentioned before, figures 2a-c only display the data for the hind limb under pre-surgical conditions. In the appendix (Figures 1a-c to 3a-c) the other measurement sites can be found. These figures are virtually the same as the figures displayed in the text (with the exception of the front limb, which appears to be equally biased at any arterial blood pressure). Table 4: Standard deviations for each measurement location Location sd SAP sd SAP PIBP NIBP value sd DAP sd DAP PIBP NIBP value sd MAP sd MAP PIBP NIBP value Hind limb Pre-anaest 2.35 1.55 0.044 2.11 2.89 0.717 1.24 1.94 0.001 Hind limb during Sur. 3.94 9.80 0.071 2.89 19.99 0.118 3.13 3.86 0.010 Front Limb Pre-anaest 2.19 5.73 0.032 1.59 3.15 <0.001 1.54 5.62 0.020 Tail base Pre-anaest 1.22 5.73 <0.001 1.12 2.85 0.001 1.02 1.78 0.008 In Figure 3 the scatter plot displays the NIBP compared to the IBP for the Systolic Arterial blood pressure. As can be seen in this figure the difference between the NIBP and the IBP decreases as the pressure becomes higher. However it should also be noted that it is not an exact fit. This is expressed by the fact that the identity of the line is not Y=X. In other words when the IBP is 60 mmHg the NIBP gives a value of approximately 67 mmHg. In conjunction with data presented in Appendix table 1, which containes the corresponding regression lines for all the different measurement sites (hind limb, front limb and tail base) it is possible to determine that the best correlation is found in the tail base measurements (R is high). MAP once again gives the best correlations and the front limb is less accurate (based upon the identity of the lines/equation). Figure 4 a-c show information about the MAP trend over time for 6 randomly selected patients without regard for the protocol or measurement site. Although some of the peaks and dips that appear in the IABP/IBP are not found in the NIBP and the other way around the lines are quite similar. SAP and DAP plots (not included) show a similar pattern however the variability is higher in SAP and DAP so the NIBP doesn’t always follow the IABP so closely. Summarizing all of the results above, the tail base O-NIBP provides the least biased results compared to the IABP. The front limb appears to be the least reliable of the three measurementsites. Furthermore the MAP is the most accurate of the three measurement parameters for the arterial blood pressure. The cuff size itself does not seem to influence the accuracy if the manufacturer’s recommendations are taken in to account. The anesthetic protocols influence the O-NIBP to some extent. The dexmedetomidine protocols tend to make the Datex Ohmeda GE S/5 less capable to produce instant results, which means that it will take more time to get a single measurement since the inflation-deflation sequence of the cuff has to be done over again. The anesthetic protocols do not appear to differ in the amount of bias found (ANOVA yields no significant differences). Analysis of the trend-lines of all patients suggests, that the Datex Ohmeda can provide information about the SAP, DAP and MAP over time. 13 MAP Trend (patient 1) MAP Trend (patient 2) 200 mmHg mmHg 150 NIBP MAP 100 IBP MAP 50 0 160 140 120 100 80 60 40 20 0 1 4 7 10 13 16 19 22 25 28 31 34 37 40 43 NIBP MAP IBP MAP 1 measurement NIBP MAP IBP MAP 5 7 9 11 13 15 17 19 21 23 NIBP MAP IBP MAP 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 measurement MAP Trend (patient 6) 80 70 60 50 40 30 20 10 0 mmHg mmHg MAP Trend (patient 5) NIBP MAP IBP MAP 3 5 7 9 11 13 15 9 11 13 15 17 19 21 23 160 140 120 100 80 60 40 20 0 measurement 1 7 MAP Trend (patient 4) mmHg mmHg 160 140 120 100 80 60 40 20 0 3 5 Measurement MAP Trend (patient 3) 1 3 160 140 120 100 80 60 40 20 0 NIBP MAP IBP MAP 1 3 5 7 9 11 13 15 17 19 21 23 25 17 19 measurement measurement Figure 4 a-c: Randomly selected MAP trends for multiple patients. 14 Discussion When the O-NIBP device is used in a clinical setting it will surely provide the basis for decisions about fluid therapy and/or vasopressive therapy and inotropic drug use. Hence it is important that the O-NIBP (in this case the Datex Ohmeda GE S/5 O-NIBP module) provide consistent and reliable results. The American Association of Medical Instrumentation (AAMI) and the British Hypertension Society have determined standards for diverse medical equipment including NIBP-measuring devices. According to these standards any NIBP device should predict the values within a range of 5+/- 8 mmHg of error compared to the golden standard (IBP). Only a few veterinary NIBP monitors have been able to comply to these standards [Deflandre, C.J.A., 2008]. It should be noted that (in contrast to other authors, like Deflandre et al.) we looked at the percentage of bias and 95%-limits of agreements and not the absolute numbers. To put it simply, a bias of 5 mmHg is relatively limited on a blood pressure of 200 (2,5%). However it is quite large on 50 mmHg (10%). As such we prevent the misinterpretation on the extent of the bias especially in the lower blood pressures. The variability for SAP, DAP and MAP differs substantially. MAP is relatively unbiased especially on the tail base, while SAP and DAP are more variable. This can be attributed to the fact that when the MAP and cuff-pressure are (nearly) equal, the oscillations in the cuff are maximized and thus the signal is most distinct. Furthermore, the MAP is least distorted in the IABP because the dynamic response characteristics and distortions in the recording system are of little importance [Gardner, R.M., 1981]. The problems with the accuracy of the O-NIBP in light of the SAP can in part be attributed to the pulse wave. The peak pressure is relatively short lived and can easily be missed in an inflation-deflation cycle of the O-NIBP [Mandigers, P., 2005] [Binns S.H., 1995][Grosenbaugh D.A., 1998] [Stephien, R.L.,1999]. Furthermore the formation of oscillations takes more energy than pressure waves in the IABP doing there work on the transducer, as such explaining further signal loss in the O-NIBP [Binns S.H., 1995]. Lastly, there is still the aspect of vasoconstriction, which is clearly demonstrated by the results from the different anaesthetic protocols. It should be noted that the measurements on the hind limb are based upon five consecutive measurements and the tail base and front limb measurements on three. This difference means that the amount tail base and front limb data is considerably less then hind limb data. In this study several types of anesthetic protocols where used, one was a protocol of methadone and isoflurane (twelve patients). The others were dexmedetomidine in conjunction with propofol (nine patients) or alfaxalone (nine patients), respectively. It was found that in the dexmedetomidine groups the blood pressure levels where higher then in the methadone-isoflurane group (Table 2). Since dexmedetomidine is a potent vasoconstrictive agent, like all other α2-agonists, it could inevitably influence the results due to vasoconstriction in the periphery where the O-NIBP is to get a signal [Uilenreef, J.J., 2008][Lin, G.Y., 2008]. As mentioned in the results, the first time failure rate in the protocols in which dexmedetomidine was used is higher than in the methadone-isoflurane protocol (Table 3), which could mostly likely be attributed to the vasoconstriction caused by dexmedetomidine. Alfaxalone, which was used for induction and maintenance of anaesthesia, has cardiovascular effects as well. Alfaxalone produces a significant drop in blood pressure, especially in higher dosages (e.g 20 mg kg-1) [Muir, W., 2008]. In the dosages of alfaxalone used in this study (0.9 – 2.0 mg kg-1 and 2.6 – 7.6 mg kg-1 hour-1 for induction and maintenance, respectively) the effects are minimal and α2-agonistic effects (the standard premedication dexmedetomidine dose was 5 μg kg-1 in the alfaxalone study, followed by a continuous rate infusion (CRI) of 1 μg kg -1 hour-1) on the cardiovascular system are dominant. Methadone has minimal effects on the cardiovascular system when given slowly (intravenous route) over the course of a minute [Hall, L.W., 2001]. Propofol, isoflurane and sevoflurane all give a decrease in blood pressure due to actions on the heart itself and vasodilatation which can is not be prevented by premedication compensated when these are combined with methadone. However, the combination of propofol and dexmedetomidine shows higher blood pressures, which can be attributed to the α2-agonistic effects on the vascular system (peripheral vasoconstriction) [Hall, L.W., 2001]. A strange phenomenon remains being that the data collected during surgery are more variable then the data collected with out surgical stimulation. Theoretically the patient should remain as cardiovascular stable during surgery as before surgery. The exact reason is obscured since the exact amount and timing of surgical stimulation was not scored and recorded as goes for the amount and type of fluids administered to the patient. 15 Location of the cuff has effects on the accuracy of the O-NIBP. The use of the tail base produced the best results followed by the hind limb and then the front limb. The accuracy of the tail base has been demonstrated by other authors in anesthetized [Bodey,A.R., 1994][Haberman, C.E., 2006] and conscious dogs [Bodey,A.R., 1996]. It has been demonstrated that (at least in conscious dogs) that cuff placement on front- or hind limbs leads to a preoccupation with removal of the cuff in dogs. Since the dogs where anesthetized the only relevant movement would be shivering. Shivering was never seen however during measurements, as such one would expect similar results on hind limb and tail base. Perhaps the pressure-waves in the medial caudal artery are relatively strong when compared to the dorsal pedal artery. Thus creating a better signal and more reliable results at the tail base cuff site. 16 Conclusions Concluding from all above, the Datex Ohemda Ge S/5 O-NIBP blood pressure measurement device tends to under- or overestimate the IABP given the data in table 4. There is also a tendency to be less accurate during times of surgical stimulation. Accuracy, in contrast to the Goal one hypothesis (“The oscillometric Arterial blood Pressure device is only reliable at values equal or lower then normotension in comparison to the IABP”), tends to be lower in the low-normotensive and hypotensive range and the accuracy increases with increasing arterial blood pressure. It has also been determined that the tail base is the most accurate position to place the cuff and that it is wise to take the recommended cuff size for a given circumference into account. The anesthetic protocol used also influences the O-NIBP’s ability to get first time readings (not the accuracy of the readings), which can be attributed to the vasoconstrictive action of α2agonists on the vascular system. First time failure rate in the dexmedetomidine group (32%) is more then three times higher then in the methadone groups (9,5%). 17 Clinical relevance The use of the Datex Ohmeda Ge S/5 O-NIBP is only advisable under certain circumstances. The IBP remains to be the standard blood pressure measuring method for patients with ASA-III or higher. The Datex O-NIBP can provide trend information about the patient’s blood pressure (with some considerations to its accuracy) and can be used for patients that are undergoing anesthesia for minor surgery or non surgical procedures for example MRI, ultrasonography or X-ray’s. If placement of the arterial catheter fails, the Datex O-NIBP can be used as an alternative device to the IABP if properly used (e.g. cuff placed on the tail base and the correct cuff size is used). Single measurements yield no reliable data, it is best to consider trends for decision making. Sudden peaks or dips don’t always indicate that a patient is in trouble. When dips or peaks are maintained over longer periods or when other vital signs are changing in conjunction to a single measurement it could spell trouble and action can be taken. The MAP needs to be the main focus when monitoring the blood pressure with the Datex since this parameter is the least biased and least variable of the three arterial blood pressure parameters. Anesthetic protocols have some influence on the system’s functioning, and although they do not change the amount of variation, they can change the Datex ability to quickly provide results. Especially protocols with dexmedetomidine influence the O-NIBP system so this should be considered when selecting a time interval for measurements. The best interval time for the Datex is 2,5 to 5 minute at maximum otherwise the intervals become to great to provide up-to-date information. Since the average time for an inflation-deflation cycle is approximately one minute shorter than 2,5 minute intervals are not advisable. 18 Acknowledgements I would like to thank the following persons for supporting me during my research. Rob Sap for supporting me on a day to day basis with my problems and questions as well for is support during the writing of research-proposal, this research paper and the article that (hopefully) is going to follow from it. Furthermore, my thanks for the placement of many arterial catheters on the patients, otherwise measuring would not have been possible. On that same matter (placement of arterial catheters) I would also like to thank Ies Akkerdaas and Joost Uilenreef. And of course Ies also for suggesting the NIBP-subject in the first place. And the both of them for suggestions and tips given during my time on the OR. Of course the rest of the staff working on the OR during my “onderzoeksstage” should be mentioned as well for making it so enjoyable. Noting better than having a good time when you are doing your work. And last but not least I would like to thank Erik Teske for his help and support with the statistical analysis of the collected data. He helped me a great deal with his insights and his time input for analysing the data. Knowing myself it would have turned out a complete disaster when I was left by my self to do the statistics on my own. Thanks again. 19 Appendix Difference (gemSAP-NIBP AP - gemSAP-IBP AP) / Mean of All Difference Plot 50% Identity 40% Bias (-1.0%) 30% 95% CI 20% 95% Limits of agreement (-34.7% to 32.7%) 10% 95% CI 0% -10% -20% -30% -40% -50% 60 80 100 120 140 160 180 200 220 Mean of All Appendix Figure 1a: SAP difference plot for the O-NIBP (during surgical stimulation) at the hind limb Difference (gemDAP-NIBP AP - gemDAP-IBP AP) / Mean of All Difference Plot 80% Identity 60% Bias (-15.3%) 40% 95% CI 20% 95% Limits of agreement (-71.0% to 40.5%) 0% 95% CI -20% -40% -60% -80% -100% 20 40 60 80 100 120 Mean of All Appendix figure 1b: DAP difference plot for the O-NIBP (during surgical stimulation) at the hind limb 20 Difference Plot Difference (gemMAP-NIBP AP - gemMAP-IBP AP) / Mean of All 50% Identity 40% Bias (2.9%) 30% 95% CI 20% 95% Limits of agreement (-28.1% to 34.0%) 10% 95% CI 0% -10% -20% -30% -40% -50% 50 70 90 110 130 150 Mean of All Appendix figure 1c: MAP difference plot for the O-NIBP (during surgical stimulation) at the hind limb Difference Plot Difference (gemSAP-NIBP_VP - gemSAP-IBP_VP) / Mean of All 40% Identity 30% Bias (-7.8%) 20% 95% CI 10% 95% Limits of agreement (-41.7% to 26.1%) 0% 95% CI -10% -20% -30% -40% -50% -60% 80 100 120 140 160 180 200 Mean of All Appendix figure 2a: SAP difference plot for the O-NIBP (post surgical stimulation) at the front limb 21 Difference (gemDAP-NIBP_VP - gemDAP-IBP_VP) / Mean of All Difference Plot 40% Identity 20% Bias (-27.4%) 95% CI 0% 95% Limits of agreement (-75.0% to 20.1%) -20% 95% CI -40% -60% -80% -100% 20 40 60 80 100 Mean of All Appendix figure 2b: DAP difference plot for the O-NIBP (post surgical stimulation) at the front limb Difference (gemMAP-NIBP_VP - gemMAP-IBP_VP) / Mean of All Difference Plot 40% Identity 30% Bias (-7.3%) 20% 95% CI 10% 95% Limits of agreement (-35.7% to 21.0%) 0% 95% CI -10% -20% -30% -40% -50% 60 70 80 90 100 110 120 130 Mean of All Appendix figure 2c: MAP difference plot for the O-NIBP (post surgical stimulation) at the front limb 22 Difference (gemSAP-NIBP_SB - gemSAP-IBP_SB) / Mean of All Difference Plot 30% Identity 20% Bias (-11.2%) 10% 95% CI 0% 95% Limits of agreement (-36.0% to 13.6%) 95% CI -10% -20% -30% -40% -50% 60 80 100 120 140 160 180 200 Mean of All Appendix figure 3a: SAP difference plot for the O-NIBP (post surgical stimulation) at the tail base Difference (gemDAP-NIBP_SB - gemDAP-IBP_SB) / Mean of All Difference Plot 30% Identity 20% Bias (-22.2%) 10% 95% CI 0% -10% 95% Limits of agreement (-56.3% to 12.0%) -20% 95% CI -30% -40% -50% -60% -70% 20 40 60 80 100 Mean of All Appendix figure 3b: DAP difference plot for the O-NIBP (post surgical stimulation) at the tail base 23 Difference (gemMAP-NIBP_SB - gemMAP-IBP_SB) / Mean of All Difference Plot 30% Identity 20% Bias (-4.6%) 95% CI 10% 95% Limits of agreement (-23.6% to 14.3%) 0% 95% CI -10% -20% -30% -40% 40 60 80 100 120 140 Mean of All Appendix figure 3c: MAP difference plot for the O-NIBP (post surgical stimulation) at the tail base Appendix table 1: Values for scatter plots for each location. Values from tail base (xxx-xxxx-TB) based upon three measurements instead of five for the hind limb (xxx-xxxx-HL), hind limb presurgical (xxx-xxxx-preHL) and front limb (xxx-xxxx-FL). Parameter Combination R Adjusted-R2 Significance Equation SAP-IABP-preHL SAP-NIBP-preHL 0,841 0,697 <0,001 Y=15.884 + 0.851X DAP-IABP-preHL DAP-NIBP-preHL 0,801 0,628 <0,001 Y=-8.118 + 0.904X MAP-IABP-preHL MAP-NIBP-preHL 0,852 0,715 <0,001 Y=2.875 + 0,981X SAP-IABP-HL SAP-NIBP-HL 0,747 0,536 <0,001 Y=36.262 +0.707X DAP-IABP-HL DAP-NIBP-HL 0,730 0,510 <0,001 Y=2,394 +0.853X MAP-IABP-HL MAP-NIBP-HL 0,850 0,709 <0,001 Y=12.751 + 0.888X SAP-IABP-FL SAP-NIBP-FL 0,654 0,289 0,003 Y=55.04 + 0.949X DAP-IABP-FL DAP-NIBP-FL 0,596 0,327 0,002 Y=16.206 + 0.533X MAP-IABP-FL MAP-NIBP-FL 0,659 0,409 <0,001 Y=37.551 + 0.490X SAP-IABP-TB SAP-NIBP- TB 0,873 0,752 <0,001 Y=-19.895 + 1.06X DAP-IABP-TB DAP-NIBP- TB 0,919 0,839 <0,001 Y=-12.488 + X MAP-IBP-TB MAP-NIBP- TB 0,933 0,870 <0,001 Y=-7.899 + 1.056X 24 References [Anonymous]. (2005) Standards for basic anesthetic monitoring. http://www.asahq.org/publicationsAndServices/standards/02.pdf. Accessed 12/8, 2008 BERNE R. M., LEVY M. N., KOEPPEN B. M. & STANTON B. A. (2004) Physiology. In Arterial System. 5th edn. Anonymous St. Louis, Mosby-Elsevier. pp 355-367 BILLIET E. & COLARDYN F. (1998) Pressure measurement evaluation and accuracy validation: The gabarith test. Intensive Care Medicine 24, 1323-1326 BINNS S. H., SISSON D. D., BUOSCIO D. A. & SCHAEFFER D. J. (1995) Doppler ultrasonographic, oscillometric sphygmomanometric, and photoplethysmographic techniques for noninvasive blood pressure measurement in anesthetized cats. Journal of Veterinary Internal Medicine / American College of Veterinary Internal Medicine 9, 405-414 BIRKS R. J. S., GEMMELL L. W., O’SULLIVAN E. P., ROWBOTHAM D. J. & SNEYD J. R. (2007) http://www.aagbi.org/publications/guidelines/docs/standardsofmonitoring07.pdf. Accessed 12/8, 2008 BLAND J. M. & ALTMAN D. G. (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1, 307-310 BODEY A. R., YOUNG L. E., BARTRAM D. H., DIAMOND M. J. & MICHELL A. R. (1994) A comparison of direct and indirect (oscillometric) measurements of arterial blood pressure in anaesthetised dogs, using tail and limb cuffs. Research in Veterinary Science 57, 265-269 CHALIFOUX A., DALLAIRE A., BLAIS D., LARIVIERE N. & PELLETIER N. (1985) Evaluation of the arterial blood pressure of dogs by two noninvasive methods. Canadian Journal of Comparative Medicine.Revue Canadienne De Medecine Comparee 49, 419-423 DEFLANDRE C. J. & HELLEBREKERS L. J. (2008) Clinical evaluation of the surgivet V60046, a non invasive blood pressure monitor in anaesthetized dogs. Veterinary Anaesthesia and Analgesia 35, 13-21 GAINS M. J., GRODECKI K. M., JACOBS R. M., DYSON D. & FOSTER R. A. (1995) Comparison of direct and indirect blood pressure measurements in anesthetized dogs. Canadian Journal of Veterinary Research = Revue Canadienne De Recherche Veterinaire 59, 238-240 GARDNER R. M. (1981) Direct blood pressure measurement--dynamic response requirements. Anesthesiology 54, 227-236 GEDDES L. A., COMBS W., DENTON W., WHISTLER S. J. & BOURLAND J. D. (1980) Indirect mean arterial pressure in the anesthetized dog. The American Journal of Physiology 238, H664-6 GROSENBAUGH D. A. & MUIR W. W.,3RD. (1998) Accuracy of noninvasive oxyhemoglobin saturation, end-tidal carbon dioxide concentration, and blood pressure monitoring during experimentally induced hypoxemia, hypotension, or hypertension in anesthetized dogs. American Journal of Veterinary Research 59, 205-212 HABERMAN C. E., KANG C. W., MORGAN J. D. & BROWN S. A. (2006) Evaluation of oscillometric and doppler ultrasonic methods of indirect blood pressure estimation in conscious dogs. Canadian Journal of Veterinary Research = Revue Canadienne De Recherche Veterinaire 70, 211-217 HALL L. W., CLARKE K. W. & TRIM C. M. (2001) Veterinary anaesthesia. 10th edn. London, Saunders 25 KUUSELA E., VAINIO O., SHORT C. E., LEPPALUOTO J., HUTTUNEN P., STROM S., HUJU V., VALTONEN A. & RAEKALLIO M. (2003) A comparison of propofol infusion and propofol/isoflurane anaesthesia in dexmedetomidine premedicated dogs. Journal of Veterinary Pharmacology and Therapeutics 26, 199-204 LIN G. Y., ROBBEN J. H., MURRELL J. C., ASPEGREN J., MCKUSICK B. C. & HELLEBREKERS L. J. (2008) Dexmedetomidine constant rate infusion for 24 hours during and after propofol or isoflurane anaesthesia in dogs. Veterinary Anaesthesia and Analgesia 35, 141-153 MANDIGERS P. (2005) Methoden van niet-invasieve bloeddrukmeting bij de hond en kat. 130, 198203 MEURS K. M., MILLER M. W. & SLATER M. R. (1996) Comparison of the indirect oscillometric and direct arterial methods for blood pressure measurements in anesthetized dogs. Journal of the American Animal Hospital Association 32, 471-475 MUIR W., LERCHE P., WIESE A., NELSON L., PASLOSKE K. & WHITTEM T. (2008) Cardiorespiratory and anesthetic effects of clinical and supraclinical doses of alfaxalone in dogs. Veterinary Anaesthesia and Analgesia NELSON R. W. & COUTO C. G. (2003) Small animal internal medicine. In Systemic Arterial Hypertension. 3rd edn. Anonymous St. Louis, Mosby. pp 199-205 PETRIE A. & WATSON P. (1999) Statistics for veterinary and animal science. In Additional Topics. 1st edn. Anonymous Malden (USA), Blackwell Science Ltd. pp 168-181 SAWYER D. C., GUIKEMA A. H. & SIEGEL E. M. (2004) Evaluation of a new oscillometric blood pressure monitor in isoflurane-anesthetized dogs. Veterinary Anaesthesia and Analgesia 31, 27-39 SHARN VETERINARY INC. (2008) http://www.sharnvet.com/CustomerService/faqs.aspx. Accessed 11/24, 2008 STEPIEN R. L. & RAPOPORT G. S. (1999) Clinical comparison of three methods to measure blood pressure in nonsedated dogs. Journal of the American Veterinary Medical Association 215, 16231628 UILENREEF J. J., MURRELL J. C., MCKUSICK B. C. & HELLEBREKERS L. J. (2008) Dexmedetomidine continuous rate infusion during isoflurane anaesthesia in canine surgical patients. Veterinary Anaesthesia and Analgesia 35, 1-12 VALERIO F., MARISCOLI M. & PETRIZZI L. (2006) Comparative evaluation of the accuracy of oscillometric and direct methods for arterial blood pressure monitoring during anaesthesia in dogs. 30, 321-323 WAGNER A. E. & BRODBELT D. C. (1997) Arterial blood pressure monitoring in anesthetized animals. Journal of the American Veterinary Medical Association 210, 1279-1285 26