Hospice of North Iowa - Northeast Iowa Family Practice
advertisement
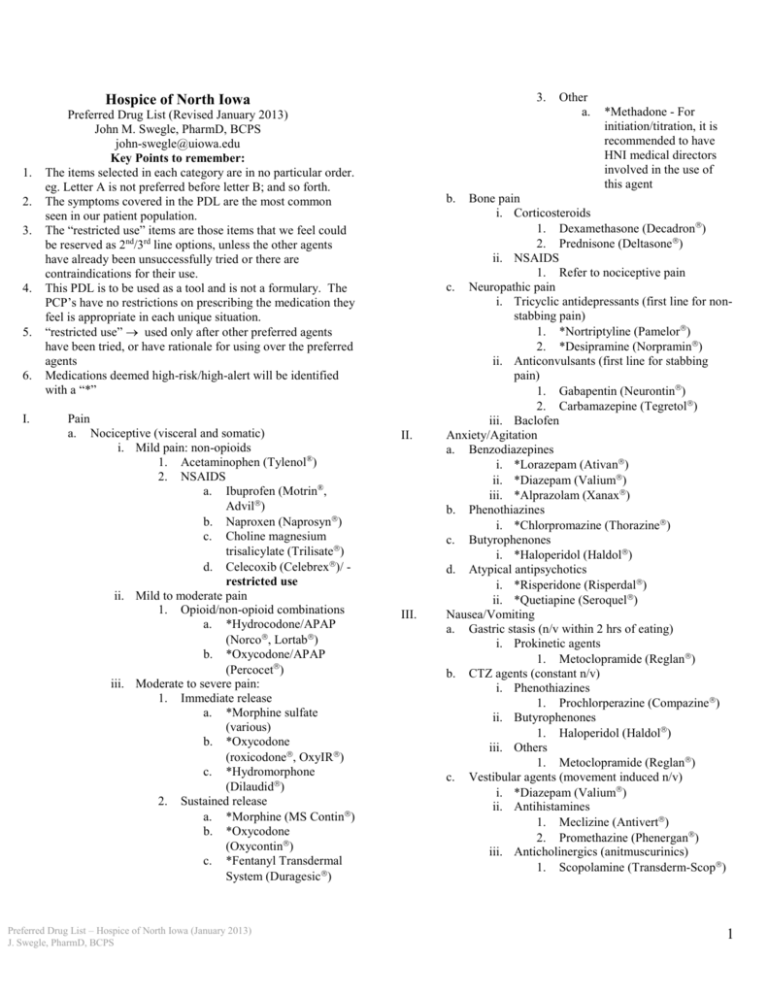
3. Hospice of North Iowa 1. 2. 3. 4. 5. 6. I. Preferred Drug List (Revised January 2013) John M. Swegle, PharmD, BCPS john-swegle@uiowa.edu Key Points to remember: The items selected in each category are in no particular order. eg. Letter A is not preferred before letter B; and so forth. The symptoms covered in the PDL are the most common seen in our patient population. The “restricted use” items are those items that we feel could be reserved as 2nd/3rd line options, unless the other agents have already been unsuccessfully tried or there are contraindications for their use. This PDL is to be used as a tool and is not a formulary. The PCP’s have no restrictions on prescribing the medication they feel is appropriate in each unique situation. “restricted use” used only after other preferred agents have been tried, or have rationale for using over the preferred agents Medications deemed high-risk/high-alert will be identified with a “*” Pain a. Nociceptive (visceral and somatic) i. Mild pain: non-opioids 1. Acetaminophen (Tylenol®) 2. NSAIDS a. Ibuprofen (Motrin®, Advil) b. Naproxen (Naprosyn) c. Choline magnesium trisalicylate (Trilisate) d. Celecoxib (Celebrex)/ restricted use ii. Mild to moderate pain 1. Opioid/non-opioid combinations a. *Hydrocodone/APAP (Norco, Lortab) b. *Oxycodone/APAP (Percocet) iii. Moderate to severe pain: 1. Immediate release a. *Morphine sulfate (various) b. *Oxycodone (roxicodone, OxyIR) c. *Hydromorphone (Dilaudid) 2. Sustained release a. *Morphine (MS Contin) b. *Oxycodone (Oxycontin) c. *Fentanyl Transdermal System (Duragesic) Preferred Drug List – Hospice of North Iowa (January 2013) J. Swegle, PharmD, BCPS Other a. *Methadone - For initiation/titration, it is recommended to have HNI medical directors involved in the use of this agent b. II. III. Bone pain i. Corticosteroids 1. Dexamethasone (Decadron) 2. Prednisone (Deltasone) ii. NSAIDS 1. Refer to nociceptive pain c. Neuropathic pain i. Tricyclic antidepressants (first line for nonstabbing pain) 1. *Nortriptyline (Pamelor) 2. *Desipramine (Norpramin) ii. Anticonvulsants (first line for stabbing pain) 1. Gabapentin (Neurontin) 2. Carbamazepine (Tegretol) iii. Baclofen Anxiety/Agitation a. Benzodiazepines i. *Lorazepam (Ativan) ii. *Diazepam (Valium) iii. *Alprazolam (Xanax) b. Phenothiazines i. *Chlorpromazine (Thorazine) c. Butyrophenones i. *Haloperidol (Haldol) d. Atypical antipsychotics i. *Risperidone (Risperdal) ii. *Quetiapine (Seroquel) Nausea/Vomiting a. Gastric stasis (n/v within 2 hrs of eating) i. Prokinetic agents 1. Metoclopramide (Reglan) b. CTZ agents (constant n/v) i. Phenothiazines 1. Prochlorperazine (Compazine ) ii. Butyrophenones 1. Haloperidol (Haldol) iii. Others 1. Metoclopramide (Reglan) c. Vestibular agents (movement induced n/v) i. *Diazepam (Valium) ii. Antihistamines 1. Meclizine (Antivert) 2. Promethazine (Phenergan) iii. Anticholinergics (anitmuscurinics) 1. Scopolamine (Transderm-Scop) 1 d. e. f. IV. V. VI. VII. Cerebral cortex agents (anxiety induced n/v) i. Benzodiazepines § 1. *Lorazepam (Ativan) 2. *Alprazolam (Xanax) 3. *Diazepam (Valium) § available in topical gel Combinations* (severe n/v) i. *ABH supp (ativan 2mg, benadryl 12.5mg, haldol 2mg)§ ii. *RBD supp (reglan 10mg, benadryl 25mg, dexamethasone 4mg) § available in topical PLO gel Other i. Ondansetron (Zofran) 1. Limit use to those with serotonininduced nausea (radiation, highly emetogenic chemotherapy) GI Irritation a. Antacids i. Maalox ii. Mylanta iii. Calcium carbonate (Tums) b. H2 Antagonists i. Famotidine (Pepcid) c. Proton Pump Inhibitors i. Omeprazole (Prilosec OTC) ii. Lansoprazole (Prevacid) iii. Esomeprazole (Nexium) – restricted use Depression a. SSRI’s i. Sertraline (Zoloft) ii. Citalopram (Celexa) iii. Paroxetine b. Tricyclic antidepressants i. Nortriptyline c. Miscellaneous i. Mirtazapine (Remeron) ii. Bupropion (Wellbutrin) iii. Venlafaxine (Effexor) d. Psychostimulants* i. Methylphenidate (Ritalin) - limit use and duration Insomnia a. Sedative/hypnotics* i. Lorazepam (Ativan) ii. Temazepam (Restoril) iii. Zolpidem (Ambien) b. Antidepressants i. Trazodone (Desyrel) Constipation Preferred Drug List – Hospice of North Iowa (January 2013) J. Swegle, PharmD, BCPS a. b. c. d. Stimulant laxatives i. Sennosides (Senokot-S) ii. Bisacodyl (Dulcolax) iii. Enema (Fleets®) Stool softeners i. Docusate (Colace) Saline laxatives i. MOM ii. Magnesium citrate Osmotic laxatives i. PEG (Miralax) ii. Sorbitol 70% VIII. Diarrhea/Gas a. Antidiarrheal agents i. Loperamide (Immodium) ii. Diphenoxylate/atropine (Lomotil)* iii. APAP w/codeine* b. Antiflatulants i. Simethicone (Mylicon) IX. Seizures a. Antiepileptic agents* i. Phenytoin (Dilantin) ii. Valproic acid derivatives (Depakote) iii. Levetiracetam (Keppra) b. Benzodiazepines* i. Lorazepam (Ativan) ii. Diazepam (Valium) X. Fluid overload (edema, heart failure) a. Thiazide/thiazide-like diuretics i. §Metolazone (Zaroxolyn) § may use in combination with loop b. Loop diuretics i. Furosemide (Lasix) ii. Torsemide (Demadex) - use as alternative for oral furosemide failure c. Potassium sparing diuretics i. Spironolactone (Aldactone) XI. Blood coagulation a. Anticoagulants* i. Warfarin sodium (Coumadin) ii. Enoxaparin (Lovenox) iii. Heparin b. Anti-platelet i. Aspirin ii. Clopidogrel (Plavix) XII. Infection a. Antibiotics i. -lactam antibiotics 1. Amoxicillin 2 b. c. 2. Cephalexin (Keflex) ii. Macrolides 1. Azithromycin (Zithromax) iii. Fluoroquinolones – restricted use 1. Levofloxacin (Levaquin) 2. Ciprofloxacin (Cipro) iv. Miscellaneous 1. Metronidazole (Flagyl) 2. Sulfamethoxazole/trimethoprim (Bactrim) 3. Doxycycline Antivirals i. Acyclovir (Zovirax) Anitfungals i. Nystatin (Mycostatin) ii. Clotrimazole (Mycelex troches) iii. Fluconazole (Diflucan) XIII. Skeletal muscle spasms a. Benzodiazepines* i. Diazepam (Valium) b. “Skeletal muscle relaxants” i. Cyclobenzaprine (Flexeril) ii. Metaxalone (Skelaxin) c. Miscellaneous i. Nortriptyline (Pamelor) ii. Amitriptyline (Elavil) XIV. Hiccups a. Chlorpromazine (Thorazine) b. Baclofen (Lioresal) XV. Pruritis a. Antihistamine i. Diphenhydramine (Benadryl) ii. Hydroxyzine (Atarax, Vistaril) iii. Cetirizine (Zyrtec) b. H2 antagonists i. Famotidine (Pepcid) c. Antidepressant i. Doxepin (Sinequan, Zonalon) d. Corticosteroids i. Prednisone XVI. XVII. Mucositis/Stomatitis a. Cryotherapy (ice chips, popsicles, cold liquids) b. Viscous lidocaine c. “Stomatitis cocktail”: Benadryl elixir 30 ml + Maalox suspension 30 ml + Viscous Lidocaine 2% 30 ml b. i. Oxybutynin (Ditropan immediate-release) ii. Tolterodine (Detrol LA) Urinary burning sensation i. Phenazopyridine (Pyridium) XVIII. Anorexia a. Prednisone (Deltasone) b. Dexamethasone (Decadron) c. Amitriptyline (Elavil) d. Mirtazapine (Remeron) e. Megestrol acetate (Megace®) – Restricted use; liquid preferred XIX. Upper respiratory symptoms a. (cough, congestion) i. Antitussives* 1. Dextromethorphan/guaifenesin (Robitussin DM) 2. Hydrocodone/guaifenesin (Codiclear) 3. Morphine (Roxanol) ii. Expectorants 1. Guaifenesin (Humibid LA, Mucinex) 2. Fluids b. Bronchospasms i. -agonists 1. Albuterol (Ventolin) ii. Anticholinergics 1. Ipratropium bromide (Atrovent) use Combivent if on both iii. Corticosteroids – oral therapy more effective in terminal care 1. Prednisone (Deltasone) 2. Dexamethasone (Decadron) XX. Copious secretions a. Anticholinergics i. Atropine 1. Eye drops given orally 2. Injection for acute control ii. Scopolamine (Transderm Scop) – best to limit use due to delayed onset of effect iii. Glycopyrrolate (Robinul) XXI. Dyspnea a. Identify and treat the cause (if possible) b. Morphine (Roxanol)* c. Lorazepam (Ativan)* d. Non-pharmacologic Bladder issues a. Bladder spasms Preferred Drug List – Hospice of North Iowa (January 2013) J. Swegle, PharmD, BCPS 3