the use of recombinant human granulocyte colony stimulating factor
advertisement

ISRAEL JOURNAL OF
VETERINARY MEDICINE
Vol. 56 (2) 2001
THE USE OF RECOMBINANT HUMAN
GRANULOCYTE COLONY STIMULATING FACTOR
AND RECOMBINANT HUMAN ERYTHROPOIETIN IN
THE TREATMENT OF SEVERE PANCYTOPENIA DUE
TO CANINE MONOCYTIC EHRLICHIOSIS
I. Aroch and S. Harrus
Koret School of Veterinary Medicine, The Hebrew University of Jerusalem, P.O.
Box 12, 76100 Rehovot, Israel
Abstract
The chronic severe form of canine monocytic ehrlichiosis (CME) is characterized by severe
pancytopenia, and carries a grave prognosis despite treatment. Treatment options are usually limited to
supportive care, anti-ehrlichial drugs and blood component therapy. This case report describes for the
first time successful treatment of a dog with severe chronic pancytopenia caused by CME. The
treatment included a combination of haematopoietic growth factors (recombinant human granulocyte
colony stimulating factor and recombinant human erythropoietin) and a long course of glucocorticoid
therapy.
Canine monocytic ehrlichiosis (CME) is a tick-borne (Rhipicephalus sanguineus) disease of
canids, caused by the rickettsia Ehrlichia canis, and is now recognized worldwide (1). CME consists of
acute, subclinical and chronic phases. Dogs may recover from the acute phase of the disease without
treatment, however some remain subclinically infected, and several months to years later may develop
the severe pancytopaenic chronic stage. This pancytopaenic chronic phase of CME has a grave
prognosis despite therapy (1,2,3,4,5). Hematopoietic growth factors have been proposed as a rational
treatment for the chronic pancytopaenic phase (5). However, no clinical trials using this mode of
therapy have been published. This report describes the successful treatment of a severely
pancytopaenic dog in the chronic stage of CME, with long-term corticosteroid therapy in combination
with two synthetic recombinant haematopoietic factors: human granulocyte colony stimulating factor
(rhG-CSF) and human erythropoietin (rh-EPO).
A three-year old male weimaraner dog was referred to the Hebrew University Veterinary
Teaching Hospital with chief complaints of exercise intolerance for the last 3 months, fever, and a
history of tick infestation. Two weeks prior to presentation, the referring veterinarian performed a
complete blood count (CBC) which revealed a severe pancytopenia {white blood cells (WBC) 0.29x103/mm3, platelets (Plt) - 2x103/mm3, red blood cells (RBC) - 3.94x106/mm3}. Serologic testing for
E. canis with a commercial dot-blot enzyme-linked immunosorbent assay kit (Biogal Laboratories,
Galed, Israel) was strongly positive. A presumptive diagnosis of CME was made, and the dog was
treated with doxycycline (5mg/kg q12h PO for 14 days) and imidocarb-dipropionate (5mg/kg IM,
single injection).
On the day of presentation (day 1) the dog’s general condition had deteriorated, it was lethargic,
anorexic, emaciated and had a fever (40.60C), tachycardia (160/min), tachypnea (60/min), severe
dyspnea, increased respiratory sounds and pale mucous membranes. CBC revealed severe pancytopenia
(Table 1), severe anemia (RBC - 2.48x106/mm3), and no evidence of RBC regeneration in peripheral
blood smears (reticulocyte count was 0%). The dog had hyperglobulinemia (globulin - 6.2g/dl), mild
hypoalbuminemia (albumin — 2.4 g/dl), with an A/G ratio of 0.39. Thoracic radiographs showed signs
consistent with severe bronchopneumonia. The E. canis IgG indirect immunofluorescence antibody test
(IFA) titer was 1:5120. Severe chronic CME, with secondary bronchopneumonia, were diagnosed.
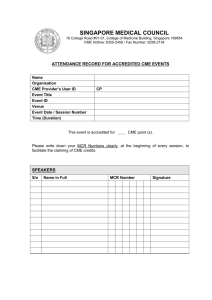
Table 1: Hematological values of a dog with severe chronic pancytopenia due to CME,
successfully treated with hematopoietic growth factors and prednisone, during a 476 day period
Day
WBC
(103/mm3)
RBC
(106/mm3)
HB (g/dl)
Ht
(%)
MCV
(fl)
MCH
(pg)
MCHC
(g/dl)
Plt
(
103/mm3)
TS (g/dl)
1
0.2
2.84
6.4
19.5
69
22.5
32.8
6
86
4
1.0
3.24
7.4
21.4
66
22.8
34.5
30
82
10
2.1
2.66
6.1
18.0
68
22.9
33.8
12
92
11
2.7
2.97
7
20.5
69
23.5
34.1
5
80
16
2.0
2.63
6.4
18.7
71
24.3
34.2
21
80
26
1.3
2.41
5.9
17.7
73
24.4
33.3
22
72
41
1.8
2.00
5.3
16.4
82
26.5
32.3
13
74_
64
2.2
2.21
6.3
19.7
89
28.5
31.9
40
72
95
1.8
4.19
10.7
32.2
77
25.5
33.2
33
80
113
3.67
4.39
10.8
34.6
79
24.6
31.2
13
Nd
142
4.5
4.92
10.8
33.1
67
21.9
32.6
64
78
191
11.8
5.14
11.5
33.7
66
22.4
34.1
3
Nd
196
11.4
5.91
12.6
38.0
64
21.3
33.1
21
88
212
19.3
5.13
12.8
32.4
63
24.9
39.5
92
90
356
9.2
5.98
12.6
35.8
60
21.0
35.1
251
90
476
15.4
6.66
14.9
0.426
64
22.3
34.9
378
74
Reference 5.5-17
5.5-8.5
12-18
37.0- 55-77 19.5- 32-36
200-700
58-78
intervals
55.0
24.5
Nd - not determined, WBC - White blood cells, RBC - Red blood cells, HB - Haemoglobin, Ht Haematocrit, MCV - mean corpuscular volume, MCH - mean corpuscular haemoglobin, MCHC - mean
corpuscular haemoglobin concentration, Plt - Platelets, TS - total solids.
The hematological results over a 476 days period are summarized in table 1. The main
treatments administered, comments of diagnoses, major clinical signs and additional data are
summarized in Table 2. Initial treatment included supportive care, cefazolin (20mg/kg IV q8h for 10
days; Cefamezin, Teva , Israel), sulfadoxin/trimethoprim (15mg/kg IV q12h for 10 days; Trimoxin,
Teva, Israel), gentamicin (2.2mg/kg IV q8h for 10 days; generic, Abic, Israel), aminophylline
(10mg/kg IV q8h for 10 days; generic, Teva, Israel), and a single injection of imidocarb-dipropionate
(5mg/kg IM; Imizol, Pitman-Moore, England).
As the dog was stabilized it was discharged on day 10 with oral cephalexine (20mg/kg q8h;
Ceforal, Teva, Israel), sulfamethoxazole/trimethoprim (20mg/kg q12h; Resprim, Teva, Israel) and
theophylline (10mg/kg q8h; Theo-Dur, Key Pharmaceuticals). On this day, recombinant-human
granulocyte colony stimulating factor (rhG-CSF) (Neupogen, Roche) therapy was initiated (Table 2)
for an overall period of 31 days (Tables 1 & 2). Resolution of bronchopneumonia was noticed
clinically, and confirmed by thoracic radiography on day 26 (table 2). Four days later, the antibiotic
treatment was changed to doxycycline (5mg/kg q12h; Doxylin, Dexxon, Israel), and prednisone (40mg
q24h; generic, Rekah, Israel), and recombinant-human erythropoietin (rhEPO; Eprex, Cilag-AG,
Germany) therapy was initiated. Erythropoietin was injected SQ q3d for a period of 36 days, followed
by 5 consecutive treatments q14d (table 2). During EPO treatment, iron (20 mg/kg IM q7d), Abidex,
Abic, Israel) and vitamins (3ml SQ q7d, Shefa-vit, Abic, Israel) were supplied continuously. The E.
canis IFA titer was 1:1280 on day 95.
Vincristine-sulfate (Vincristine, Abic, Israel) was given at 0.5mg/m2 IV on day 191, when the
dog showed severe thrombocytopaenia and petechiae, and repeated 5 days later. The platelet numbers
(Plt) increased to 3.6x103/mm3, 6 days later.
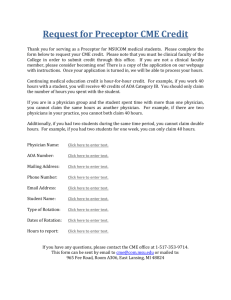
Table 2: Hematological findings, related clinical signs, and treatments during a 476-day
follow-up period of a dog with severe chronic CME and successfully treated with haematopoietic
growth factors and prednisone.
Day
1
Clinical and hematological signs
Pancytopenia, brochopneumonia, fever
3
10
Epistaxis, pancytopenia
22
Pancytopenia, petechiae
26
Pancytopenia, petechiae, resolution of bronchopneumonia
41
51
Pancytopenia, mild polychromasia
Pancytopenia, moderate polychromasia, platelet count
within reference interval
Pancytopenia, moderate polychromasia
64
142
191
Pancytopenia, neutrophil count within reference interval
196
RBC and WBC within reference interval, severe
thrombocytopenia
Mild normocytic normochromic anaemia, severe
thrombocytopaenia, WBC within reference interval
Leucocytosis,
mild
anaemia,
moderate
thrombocytopaenia, hepatozoon parasitemia, WBC within
reference interval
Mild normocytic normochromic anaemia, moderate
thrombocytopaenia, WBC within reference interval
202
212
309
Moderate anaemia, severe thrombocytopaenia, petechiae,
WBC within reference interval
356
Mild normocytic normochromic anaemia, WBC and Plt
within reference interval
427
All haematological values further improved and were
within reference intervals
476
All haematological values further improved
Treatment*
Imidocarb-dipropionate ,
Whole
blood
transfusion
(450ml)
rhG-CSF (50?g/kg q12h SQ),
imidocarb-dipropionate (5mg/kg
IM once), platelet rich
plasma transfusion (250ml)
Same as day 10
Oral doxycycline, prednisone,
rhG-CSF (50?g/kg q24h SQ),
rhG-CSF discontinued
Same as day 26
Same as day 26, rhEPO
(100U/kg once every 14 days
SQ)
rhEPO discontinued
Same as day 64, vincristine
(0.5mg/m2
once
IV),
Prednisone reduced (20mg
q24h)
Same as day 191
Vincristine stopped
Same as day 202
Prednisone dose reduced (20mg
EOD), doxycycline discontinued
Prednisone (20mg EOD)
Prednisone
(20mg
q48h
X21days, tapered to 20mg q72h
X21 days, tapered to 20mg q96h
X30 days)
All medications
and were
discontinued
within reference intervals
Treatment with immunosuppressive doses of prednisone (2mg/kg q24h PO) was initiated on day
26, when the bronchopneumonia was resolved, and was continued at that dose for 165 days, then
reduced to 0.5mg/kg q24h PO. The dose was reduced further (to 0.5mg/kg EOD) on day 309. At that
time the dog was still mildly anemic (Ht - 31.7%) and moderately thrombocytopenic (Plt 9.8x103/mm3). On day 427, when all haematological values were within reference intervals, the dose
was reduced further. On day 476, the dog was normal, the E. canis IFA titer was 1:20, and medication
was discontinued.
The diagnosis of chronic CME in the present case was based on typical clinical, haematological
and biochemical findings, a very high ehrlichial IgG IFA titer and clinical deterioration with no
response to anti-rickettsial therapy. Marked pancytopenia has been reported as the hallmark of the
severe chronic phase of CME (5), and occurs as the result of a hypocellular bone marrow (1,3,5,6).
Although bone marrow analysis was not performed in the present case due to the owner’s objection,
hypocellularity was presumed as the severe anaemia was non-regenerative and peripheral cytopaenia
was evident in all three myeloid cell lines. In our experience, severe pancytopenia due to chronic E.
canis infection with the Israeli strain carries a grave prognosis and to date conventional therapy has not
been successful (3).
The main objective of the treatment in the first period of therapy was to resolve the
bronchopneumonia by providing a broad-spectrum bacteriocidal antibiotic. However, the very low
numbers of circulating neutrophilic granulocytes might have led to failure. Human and canine
recombinant granulocyte colony stimulating factors were reported previously to increase in a dosedependent manner, the number and function of neutrophils (7). Phagocytosis, superoxide production
and antibody-dependent cytotoxicity are increased by G-CSF. In a study performed on normal healthy
dogs with recombinant canine G-CSF (rcG-CSF), the elevation in neutrophil counts in response to
treatment occurred within 24 hours, with a peak on the 19th day of treatment (7). It is unknown if the
response of a hypocellular bone marrow due to severe chronic CME, as in the present case, should be
compared with normal healthy marrow. However the mega-dose pharmacological effect could preserve
the low numbers of myeloid stem cells in the bone marrow and promote their proliferation. It has been
shown that the long-term use of rhG-CSF in dogs led to a subsequent decrease in neutrophil numbers,
presumably as a result of antibody formation to this drug (7). Thus, it was recommended that its use in
dogs should be limited to short-term therapy (7). As rcG-CSF was unavailable commercially, we
decided to use rhG-CSF. The treatment with rhG-CSF did not lead to an elevation in neutrophil
numbers throughout the treatment period (Table 1), although it might have aided in the resolution of
bronchopneumonia by increasing neutrophil function. It was decided to continue rhG-CSF treatment, at
a lower dose, with concurrent prednisone therapy given in immunosuppressive doses. The high
glucocorticoid levels may have partially prevented the destruction of rhG-CSF by antibodies.
Immunosuppression induced by high prednisone doses may also have been partially prevented by
concurrent use of rhG-CSF, by improving neutrophil function.
The use of rhEPO in veterinary medicine is increasing, mainly in erythropoietin deficiency
conditions (such as end stage renal disease) (8), but has not been reported in severe chronic CME. In
the present case, the total rhEPO treatment period was 116 days. The first response was observed 3
days after initiation of treatment, evidenced by mild polychromasia in the peripheral blood smear and
macrocytosis. This reflects a prompt bone marrow response to EPO. The mean corpuscular volume
(MCV) reached a peak of 89fl on day 64 (Table 1). During the first phase of treatment severe
hypochromia developed {mean corpuscular hemoglobin concentration (MCHC) - 24.1 g/dl}, despite a
high dose oral iron therapy. This complication of EPO treatment is well-documented (8). At this point
the platelet count increased markedly from 13x10 3/mm3 to 241x103/mm3. This could have been due to
severe depletion of body iron stores, as the number of circulating platelets was shown to be inversely
related to iron stores (9). As the MCHC improved, platelet numbers decreased markedly to
thrombocytopaenic levels. On day 95 despite a rather long (14 days) rhEPO treatment interval, the
haematocrit had improved markedly to 32.2%, the MCV was still high (77fl) and peripheral blood
smears revealed evidence of regeneration (table 1 & 2). We can assume that even with this relatively
long dosing interval rhEPO still had a beneficial effect on erythropoiesis. When the MCV returned to
normal, despite rhEPO therapy, the treatment was no longer considered effective, and was
discontinued. It is possible that immunosuppressive doses of glucocorticoids may have delayed the
production of anti-rhEPO antibodies and its destruction, and thus allowed a long beneficial effect of
EPO.
Thrombocytopaenia was the last haematological abnormality to resolve in this case. It is
possible that correction of the anemia and a gradual decrease in circulating anti-platelet antibodies and
complement concentrations, as a result of the long high-dose prednisone treatment, allowed increased
platelet production with a decline in consumption. Thrombopoietic growth factors are commercially
unavailable at present, and may prove to be important in the treatment of thrombocytopaenia secondary
to bone marrow hypocelullarity. Induction of platelet release with vincristine-sulphate treatment has
been documented previously (10). Its effect depends on the presence of satisfactory numbers of
megakariocytes in the bone marrow (11). In the present case, this mode of treatment probably had a
mild effect on platelet numbers. The platelet numbers increased from 3x10 3/mm3 to 21x103/mm3 after
one treatment, and to 36x103/mm3 following the second treatment. Thereafter the platelet numbers
continued to increase gradually with no additional vincristine therapy over a long period.
The pathogenesis of CME has been proposed to involve immunologic mechanisms, mediated
mainly by the monocyte-macrophage system and the production of excess antibodies by plasma cells
(1,3,5,6). The use of glucocorticoids in immunosuppressive doses seems rational to overcome the
excessive aberrant immune response, and has been suggested previously in severely sick animals in the
acute phase of CME (3,5,12). By the same rationale, this treatment would appear to be appropriate in
the chronic phase of CME, providing that bacterial infections are eliminated, a broad- spectrum
antibiotic treatment is administered, and neutrophil function is maintained. The beneficial effects of
glucocorticoids in CME may include the decrease in splenic destruction of blood cells and also a
decrease in immunoglobulin, complement and cytokine production, thus allowing survival and
proliferation of bone marrow stem cells and an increased life span of mature blood cells. A decrease in
immunoglobulin production was probably the main mechanism responsible for the decrease in globulin
concentrations and the improvement of the A/G ratio during treatment.
The initial E. canis antibody IFA titer was very high (1:5120, Table 2), however on day 476,
when all treatments were discontinued, the E. canis IFA antibody titer was found to be negative (less
then 1:20). Judging from the complete disappearance of E. canis antibodies and the resolution of all
clinical and hematological abnormalities, we assumed that the typical prolonged humoral reaction has
ceased, and that the parasite has been eliminated. It has been previously suggested that negative
serological results and resolution of thrombocytopenia represent elimination of the rickettsia (13).
In conclusion, this paper describes the first successful treatment of severe pancytopenia
secondary to chronic CME, caused by the Israeli strain of E. canis. The treatment included the use of
the haematopoietic growth factors rhG-CSF and rhEPO, combined with immunosuppressive doses of
glucocorticoids. The treatment described in the present case, although prolonged and expensive, may
provide a different option for therapy of severely pancytopenic CME patients. Further investigations
are needed to assess the efficacy of such therapy in a larger number of patients.
Acknowledgement
The authors thank Dr. Trevor Waner of the Israel Institute for Biological Research, Ness-Ziona
for his professional assistance.
References
1. Ristic, M. and Holland, C. J. Canine ehrlichiosis. In: Woldehiwet, Z. and Ristic M. (Eds): Rickettsial
and chlamydial diseases of domestic animals. Pergamon Press Oxford. pp 169-186, 1993.
2. Buhles, W. C., Huxsoll, D. L., and Ristic, M.: Tropical canine pancytopenia: clinical, hematologic,
and serologic response of dogs to Ehrlichia canis infection, tetracycline therapy, and challenge
inoculation. J. Inf. Dis. 130: 357-367, 1974.
3. Harrus, S., Bark, H., and Waner, T.: Canine monocytic ehrlichiosis: an update. Comp. Contin. Edu.
Vet. Pract. 19: 431-443, 1997.
4. Harrus, S., Kass, P. H., Klement, E., and Waner, T.: Canine monocytic ehrlichiosis: a retrospective
study of 100 cases, and an epidemiological investigation of prognostic indicators for the disease. Vet.
Rec. 141: 360-363, 1997.
5. Neer, T. M.: Ehrlichiosis. In: Greene, C. (Ed): Infectious diseases of the dog and the cat, 2nd edn.
Philadelphia, WB Saunders. pp 139-154, 1998.
6. Swango, L. J., Bankemper, K. W. and Kong, L. I.: Bacterial, rickettsial, protozoal and miscellaneous
infections. In: Ettinger, S. J. (Ed): Textbook of veterinary internal medicine 3rd edn. Philadelphia, WB
Saunders. pp 277-297, 1989.
7. Ogilvie, G. K., Obradovich, J. E.: Hematopoietic growth factors: clinical use and implications. In:
Kirk, R. W. and Bonagura, J. D. (Eds): Kirk’s current veterinary therapy XI, small animals practice.
Philadelphia, WB Saunders. pp 466-470, 1992.
8. Cowgill, L. D.: Application of recombinant human erythropoietin in dogs and cats. In: Kirk, R. W.
and Bonagura, J. D. (Eds): Kirk’s current veterinary therapy XI, small animal practice. Philadelphia,
WB Saunders. pp 484-487, 1992.
9. Weiser, M. G.: Erythrocyte responses and disorders. In: Ettinger, S. J. and Feldman, E. C. (Eds):
Textbook of veterinary internal medicine 4th edn. Philadelphia, WB Saunders. pp 1876-1879, 1995.
10. Robertson, J. H., Crozier, E. H., Woodend, E. D.: The effect of vincristine on the platelet count in
rats. Br. J. Haematol. 19: 331-337, 1970.
11. Ogilvie, G. K., and Moore, A. S.: Managing the veterinary cancer patient. Trenton, Veterinary
Learning Systems. pp 78-79, 1995.
12. Bartsch, R. C., Greene, R. T.: Post-therapy antibody titers in dogs with Ehrlichiosis: follow-up
study on 68 patients treated primarily with tetracycline and/or doxycycline. J. Vet. Int. Med. 10: 271274, 1996.
13. Harrus, S., Waner, T., Aizenberg, I., and Bark, H.: 1998. Therapeutic effect of doxycycline in:
Experimental subclinical canine monocytic Ehrlichiosis: evaluation of a 6-week course. J. Clin.
Microbio. 36: 2140-2142, 1998.