Acute renal failure
advertisement
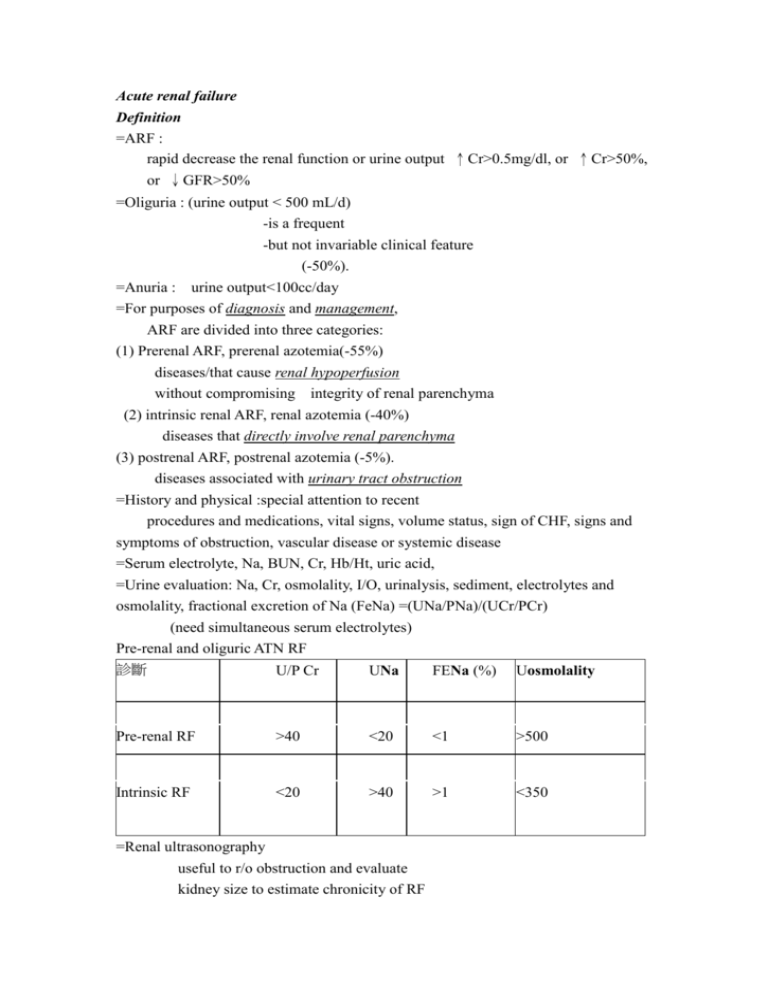
Acute renal failure Definition =ARF : rapid decrease the renal function or urine output ↑Cr>0.5mg/dl, or ↑Cr>50%, or ↓GFR>50% =Oliguria : (urine output < 500 mL/d) -is a frequent -but not invariable clinical feature (-50%). =Anuria : urine output<100cc/day =For purposes of diagnosis and management, ARF are divided into three categories: (1) Prerenal ARF, prerenal azotemia(-55%) diseases/that cause renal hypoperfusion without compromising integrity of renal parenchyma (2) intrinsic renal ARF, renal azotemia (-40%) diseases that directly involve renal parenchyma (3) postrenal ARF, postrenal azotemia (-5%). diseases associated with urinary tract obstruction =History and physical :special attention to recent procedures and medications, vital signs, volume status, sign of CHF, signs and symptoms of obstruction, vascular disease or systemic disease =Serum electrolyte, Na, BUN, Cr, Hb/Ht, uric acid, =Urine evaluation: Na, Cr, osmolality, I/O, urinalysis, sediment, electrolytes and osmolality, fractional excretion of Na (FeNa) =(UNa/PNa)/(UCr/PCr) (need simultaneous serum electrolytes) Pre-renal and oliguric ATN RF 診斷 U/P Cr UNa FENa (%) Uosmolality Pre-renal RF >40 <20 <1 >500 Intrinsic RF <20 >40 >1 <350 =Renal ultrasonography useful to r/o obstruction and evaluate kidney size to estimate chronicity of RF Category Etiology ↓cardiac output, ↓effective artery volume, sepsis, Hypovolemia, Pre-renal (↓renal blood cirrhosis (hepato-renal syndrome) flow) Drug : ACEi, NSAID, Contrast dye, cyclosporine Renal Acute tubular necrosis (ATN) (intrinsic renal -Ischemia: progression of any prerenal process toxins damage) -Drug: aminoglycocydes, amphoterecin, Cisplatin, contrast dye -Pigmets: (myoglobin, Hb), Crystal (Uric acid) or Proteins (IgG light chains) Acute interstitial nephritis (AIN) -Allergic: β-lactamantibiotics, sulfa drugs, NSAIDs, -Infection -Infiltration (sarcoid, lymphoma) -Auto immune (SLE) -Vascular : renal artery stenoses(especially bilateral +ACEi) thrombosis, hypertensive crisis, sclerderma renal crisis Cholesterol emboli, HUS/TTP Acute glomerulonephritis (AGN) Post-renal Bladder neck: BPH, prostate cancer, neuropathy, anticholindergic (Obstruction of medication urine) Ureteral : Malignancy, Lymphadenopathy, retroperitoneal fibrosis Tubular : precipitation of crystals =Renal biopsy: consider if suspect AGN [rapid ↑in Cr, proteinuria (sometimes in the nephrotic range), and an active urinary sediment with hematuria and RBC casts.] DD of Postrenal ARF - Bladder catheterization assessment of Lower tract obstruction - Ultrasonography usually identifies lower and upper tract obstruction -IVP -CT Complications - Volume overload( edema, congestive HF) - hyperkalemia, hyperphosphatemia - Uremia (encephalopathy, pericarditis, nausea, vomiting) Prevention and treatment of ARF Management of ARF Prerenal azotemia I. Hemodynamic monitoring -adequate volume expansion while avoiding overexpansion - assess and manage poor cardiac function -Invasive monitoring with a central venous pressure or pulmonary artery catheter II. Fluid Challenge -The quantity must be determined on an individual basis, but typically 500-1000 ml normal saline is infused over 30-60 minutes. -If no response is obtained, volume infusion can be followed by furosemide, 100-400 mg iv to promote urine flow. -Metolazone, 5-10 mg PO -Furosemide 10mg-40mg/H continue drip Management of Radiocontrast nephropathy: =Risk factor of Radiocontrast nephropathy (1)long term DM (2)Pre-existing renal insufficiency (Cr>1.5) (3)volume depletion (4)multiple myeloma (5)CHF (6)>65y/o =tends to be oliguric, -serum Cr peaks in the first 72 hours. -Hydration -12-24 hours before contrast and ending 12 hours after the contrast study. -Infusion rates need to be individualized -75-150 ml/hour of 0.45% saline, the -goal being a slightly volume-expanded patient with a high urine output. -Acetylcystine -1.5g/day (2pk qid/day) - starting 1 day before procedure until 12hours after procedure III. Obstructive nephropathy in the upper or lower urinary tract may incite ARF =Relief of obstruction -Foley -Surgery process - If the post-obstructive diuresis appears excessive, fluid and electrolytes should be replaced. -The appropriate initial replacement fluid in such cases is usually 0.45% saline. Prevention and treatment of complications =Intravascular volume overload -Salt (1-2 g/d) and water restriction (usually 1-1.5 L/d) -Diuretics (usually loop blockers ± thiazide) (lasix max dose=1g/day) -Ultrafiltration or dialysis Prevention and treatment of complications =Hyponatremia -Restriction of enteral free water intake (<1 L/d) -Avoid hypotonic intravenous solutions (including dextrose solutions) =Hyperkalemia -Restriction of dietary K intake (usually <40 mmol/d) -Eliminate K* supplements and K-sparing diuretic -Potassium-binding ion-exchange resins (e.g., Kyxalate) =Metabolic acidosis -Glucose (50 mL of 50 dextrose) and insulin (10 units regular) -Sodium bicarbonate (usually 50-100 mmol) -Calcium gluconate (10 mL of 10 solution over 5 min) -Dialysis (with low K* dialysate) -Restriction of dietary protein (usually 0.6 g/kg per day of high biologic value) -Sodium bicarbonate (maintain serum bicarbonate >15 mmol/L or arterial pH >7.15) -Dialysis =Nutrition -Restriction of dietary protein (0.6 g/kgper day) -Carbohydrate (100 g/d) -Enteral or parenteral nutrition (if recovery prolonged or pt very catabolic) =Indications for dialysis -Clinical evidence (symptoms or signs) of uremia -Intractable intravascular volume overload -Hyperkalemia or severe acidosis resistant to conservative measures -Prophylactic dialysis when urea >100-150 mg/dL or creatinine >8-10 mg/dL Fluid control for CRRT PAWP <6 6-8 9-11 12-14 15-17 mmHg mmHg mmHg mmHg mmHg I-O cc/H 175 cc/H 125 cc/H 18-20 21-22 >22 mmHg mmHg mmHg 75 cc/H 0 cc/H -50 cc/H -75 cc/H -100 cc/H -125 cc/H Prescribing of medications =Choice of agents Avoid -other nephrotoxins, -ACE inhibitors, -cyclooxygenase inhibitors, -radiocontrast unless absolute indication and no alternative agent =Drug dosing - Adjust doses and frequency of administration for degree of renal impairment (CCr) Management of the recovery phase of intrinsic and obstructive ARF -careful monitoring of serum electrolytes, volume status, urinary fluid and electrolyte loss -careful supplement of fluid and electrolyte when dehydration and electrolyte imbalance.