Asphyxia
advertisement

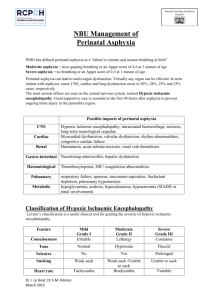
STATE ESTABLISHMENT «DNEPROPETROVSK MEDICAL ACADEMY OF MINISTRY OF HEALTH UKRAINE » “Сonfirmed;” at methodical meeting of hospital pediatrics №1 department Сhief of department professor _____________V. A. Kondratyev “______” _________________ 2013 y. METHODICAL INSTRUCTIONS FOR STUDENTS` SELF-WORK WHILE PREPARING FOR PRACTICAL LESSONS Educational discipline module № Substantial module № Theme of the lesson Course Faculty pediatrics 2 8 Asphyxia of the newborn 5 medical Dnepropetrovsk, 2013. Asphyxia of the newborn 1. Actuality of the topic: Intrahospital hypoxia – polyetiologic phenomenon which occurs quite often nowadays. It is hard to find a pregnancy which would pass without any complications (mother’s illness, toxicosis, external influence on fetus and so on). Most often chronic hypoxia is the affection factor of internal organs and systems, first of all – nervous system, therefore the knowledge of asphyxia causes, ability to render urgent medical help to a new-born baby, ability to diagnose abnormality in child’s health and carry our correcting procedures are necessary skills for each doctor. 2. Certain purposes: А. A student should know: 1. Basic causes which lead to oxygen hunger in intranatal period 2. Definition of term “asphyxia of a new-born baby” 3. Methodology of estimation of new born baby’s condition according to Apgar 4. Algorithm of rendering urgent help to a child born in asphyxia 5. Principles of intensive therapy and observation at early post-asphyxia period. 6. Consequences of new born baby’s asphyxia - in nervous system - in cardio-vascular system - in respiratory system - in kidneys - in adrenal glands - in gut - in immune system - in metabolism 7. Notion of hypoxic-ischemic encephalopathy 8. Mechanical formations of HIE 9. Clinical manifestations of HIE 10. Principles of treatment and rehabilitation of children with HIE 11. HIE outcomes B. A student should be able: 1. To determine signs of asphyxia in new-born babies 2. To estimate condition of a new-born baby according to Apgar scale 3. To determine the degree of AN 4. To draw up a plan of rendering urgent aid to a certain child 5. To draw up a plan of further child’s treatment with AN 6. To reveal signs of HIE in a new-born baby 7. To reveal signs of post-hypoxic abnormalities in other systems and organs 8. To draw up a plan of in-patient observation over children who suffered new-born asphyxia (AN) 3. Tasks for self-study work whilke preparing for the lesson 3.1. A list of basic terms, parameters, characteristics a student should master while preparing for the lesson: Term 1. Asphyxia of a new-born Definition Pathological condition caused by gas disorders in the need of 02 2 baby 2. Hipoxic-ischemic encephalopathy 3. Antenatal hypoxia 4. Intranatal hypoxia 5. Cardiac-respiratory syndrome 6. Syndrome of increased nervous anxiety 7. Syndrome of general depression 8. Hypertension syndrome 9. Hydrocephalic syndrome 10. Cramp syndrome 11. Comatose condition 12. Neurosonography necessity, superficiality of С02 which takes place along with metabolic acidosis Brain damage caused by perinatal hypoxia which is manifested by morphological-functional disorders and signs of cerebral insufficiency First revealed before birth First revealed during the delivery Mild asphyxia which develops due to depression of respiratory center which most often occurs while using sedative, pain-killers, in narcosis without acidosis development It is manifested by worry, sleep disorders, regurgitation, painful cry, increase of muscular tone, tremor of extremities and chin, hyperreflexia Most often it occurs in pre-term babies due to immaturity of CNS, which is a generalized slow-down, languor, adynamy, hyporeflexia, muscular hypotonia It is manifested by the presence of a necessary condition – head is thrown back, extremities are bent, fists are squeezed (a “boxer” pose), presence of “cerebral” cry, regurgitation and vomiting, hyper and tremor of extremities, vertical and rotator nystagmus, Grefe symptom It develops closer to the end of acute period and it is manifested by increase of head in volume, domination of cerebral cranium over facial, bridge changes with hanging of forehead part, increase of venous picture on the head, widening of liquor system and increase of ventricular index according to data of brain ultrasound It is most often manifested by generalized clonic-tonic cramps. More seldom focal and multifocal, mioclonic cramps take place. It develops in case of brain edema and it is characterized by unconsciousness, absence of motor activity, cry, emotions and reaction to pain Ultrasound of brain structures with sensor in big fontanel 3.2. Theoretical questions to the lesson: Definition of term “asphyxia of a new-born baby” Reasons of new-born asphyxia Reasons of chronic and acute intranatal fetus hypoxia Pathogenesis of changes in case of fetus hypoxia Use of contemporary diagnosing methods for fetus estimation (CT, ECG, US and so on) 6. Clinical signs of asphyxia in new-born babies 7. Methodology of estimation of new born baby’s condition according to Apgar 8. Determination of asphyxia degree 9. Urgent help to a new-born child in asphyxia 10. Contemporary equipment used for reanimation and intensive care. Methods of ALV 11. Correction of metabolism disorders 12. Complications of asphyxia in new born children - in nervous system - in cardio-vascular system - in respiratory system - in kidneys - in adrenal glands 1. 2. 3. 4. 5. 3 - in gut - in immune system - in metabolism 13. Complications of reanimation and intensive care 14. Notion of hypoxic-ischemic encephalopathy 15. Pathogenesis in development of hypoxic-ischemic encephalopathy 16. Clinical signs of hypoxic-ischemic encephalopathy. Neurological, somatic and metabolism disorders 17. Contemporary methods of diagnosing CNS disorders (neurosonography, CT, NMR, etc.) 18. Classification of hypoxic-ischemic encephalopathy 19. Treatment and rehabilitation of children with hypoxic-ischemic encephalopathy 20. Principles of treatment and control on pediatrics regions and its effectiveness 21. Outcomes of hypoxic-ischemic encephalopathy 4.3 . Practical works (tasks) which are performed on occupation: 1 To collect complaints, case history and personal (life) history 2. To inspect the child 3. To reveal early symptoms of asphyxia 4. To reveal the signs of the complications of asphyxia 5. To evaluate the condition of the child and available clinical symptoms. 6. To evaluate the results of the additional methods of investigation 7. To make the clinical diagnosis according to classification. 8. To make the plan of urgent therapeutic measures. 9. To make recommendations of dispensary supervision. . 3. Maintenance of the subject: Asphyxia of the newborn ICD-X Code: P21 Pathological life threatening condition caused by disorders of gas exchange in the form of increased requirements in 02 and excess of C02 that is accompanied by metabolic acidosis. The word "asphyxia" is translated as "without pulse", but this concept is traditionally means "dyspnea". Asphyxia in 80% of cases is the lasting fetal hypoxia, therefore it’s characterized by common etiologic and pathogenetic factors. 1. The causes which lead to acute asphyxia of the newborns: — blood supply interruption through an umbilical cord (the real knots of an umbilical cord, its compression, tense cord encirclement round a neck or other parts of the infant); - disorders of gas exchange through the placenta (premature complete or incomplete placental separation, presentation, etc.); - inadequate haemoperfusion of the maternal part of the placenta (excessively active labour, hypotension or hypertension at mother of any etiology); - deterioration of mother’s blood oxygenation (anemia, cardiovascular diseases, respiratory failure); - insufficiency of respiratory efforts of the newborn (iatrogenic - influence of drugs administered to mother, antenatal brain disorder of the fetus, congenital defects of the development of fetal lungs, etc.). 4 Intranatal hypoxia. ICD-X code: P20 Causes of antenatal fetal hypoxia: - overterm pregnancy; - long-standing (more than 4 weeks) gestoses; - multiple pregnancy; - threat of interruption of pregnancy; - diabetes in the pregnant women; - bleedings and infectious diseases in the II—III trimesters of pregnancy; - serious somatic disorders of the pregnant woman; - smoking or other types of drug addiction of the pregnant woman; - delay of intrauterine fetal development or other diseases revealed by ultrasonic or other fetal investigations. Causes of intranatal fetal hypoxia: - Cesarean section (planned or urgent); - pelvic, gluteal or others abnormal fetal position; - premature or late birth; - waterless interval more than 24 or less than 6 hours; - first labor – if it is less than 4 hours at the woman who delivers for the first time and 2 hours at repeated childbirth; - presentation or premature detachment of the placenta, rupture of the uterus; - usage of obstetric forceps, vacuum extractor and other obstetric interventions in labor; - discrepancy of the sizes of the fetal head and sizes of pelvis of mother; - acute hypoxia in childbirth at mother (shock, decompensation of somatic diseases, poisoning, etc.) - disorders of placental fetal (umbilical) blood circulation at tense cord encirclement, real knots, a tension of a small umbilical cord on length, loss of its loops, pressing loops of umbilical cord by fetal head to the walls of the birth canal - fetal cardiovascular, respiratory diseases, diagnosed by ultrasonic investigation - abnormal fetal heart rate; - mekonium in waters, increased or decreased amount of waters; - the narcotic and other analgetics, administered to the mother in 4 hours and less prior to the delivery, the general anesthesia at mother. 2. Pathogenesis of fetal disorders at hypoxia: At exposures of the specified mechanisms gas exchange is disordered and oxygen starvation of tissues develops. At the hypoxia more differentiated and young tissues, namely a brain, most often suffer. At the short-term hypoxia disorders of nervous system are reversible and are manifested by disorders of blood circulation and liquor circulation (expansion and overflow of vessels by blood, increase of permeability of the vascular wall, etc.). At longstanding oxygen deficiency there are irreversible changes of the brain and other fetal organs (lungs, heart, kidneys, adrenal glands, liver) owing to hemorrhages, ischemia, edema, dystrophy, necroses. In the pathogenesis of hypoxia there is a short circuit of many "vicious circles" - disorders of oxygenation leads to haemodynamical changes which, in turn, strengthen tissue acidosis. Severe asphyxia breaks compensatory mechanisms, pathological acidosis, arterial hypotension, disorders of permeability of cellular membranes, a hypovolemia, electrolytic disorders occur. The most threatening complication is the brain ischemia resulting in degenerative changes. 3. Main clinical manifestations of the fetal hypoxia: Heart rate disturbances (at first tachycardia, then bradycardia), deterioration of sonority of heart tones (at the beginning small strengthening, then - dullness of tones); occurance of arrhythmia, mekonium in waters, change of parameters of acid-base balance of waters and fetal blood. 5 Aschyxia of the newborn is clinically manifested by the presence of signs of disorders of vital systems: respiratory, cardiovascular, urinary, digestive, etc. for the first 3 days of life; existence of clinical signs CNS disorders, and also presence of metabolic acidosis. 4 . Technique of an assessment of the newborn by Apgar scale. Definition of the degree of asphyxia. For the assessment of severity of asphyxia the Apgar scale is used which includes main indicators of activity of the newborn: heart rate, breathing, muscular tone, reflexes, skin color. Each of the above listed criteria is estimated by two-point system (0, 1, 2). Final conclusion about the condition of the child is done on the basis of the score behind all 5 counted criteria. Assessment of the condition of the child should be carried out on the 1st minute and in 5 minutes after the birth. Light asphyxia corresponds to the 6-7 points, moderate - 4-5 points and severe - 1-3 points. Light asphyxia is regarded as the cardiorespiratory syndrome owing to thedepression of the respiratory center which is mostly seen at administration of sedative, anesthetizing preparations, an anesthesia. Unlike asphyxia, acidosis isn't characteristic for this syndrome. Clinical sign Heart rate Breathing Muscular tone The reflex excitability (reaction to the catheter) Skin color Table 1. V. Apgar scale (1953) Assessment in points 0 1 2 Absent Less than 100 in 1 More than 100 in 1 min min Absent Bradipnoe, Normal, loud cry irregular Absent Easy flexing of Active movements extremities Absent Grimace Sneezing, cough Skin color of Pink Generalised pallor or color of the body, Pink cyanosis cyanosis of color of the body extremities.. 5. The urgent help at asphyxia of the newborn The protocol of resuscitation actions at asphyxia of the newborn At pure waters At intensive meconial contamination of waters 1. To put the newborn under a source of radial 1. To suck contents of an oral cavity, a throat and a heat on the horizontal dense surface. nose cavity by the catheter after the birth of the head 2. To dry skin quickly by the warm diaper. 2. As soon as newborn it is located under the radial 3. To take away a wet diaper. heater, immediately to provide its correct situation. 4. To provide the correct provision of the head 3. Under control of the direct laringoscopia (as a rule, under shoulders enclose the roller). to suck residual meconium from the throat, then to 5. To suck at first oral cavity contents, and then intubate trachea and respiratory airways directly — nasal part of the throat (it isn't recommended through an endotracheal tube, then by special deep and intensive suctions by a probe; negative aspirator to suck away residual meconium pressure: at suction shouldn't exceed 100 mm 4. Quickly to dry up skin of the newborn by the hg). warm diaper. 5. To take away a wet diaper. 6 6. To carry out short (no more than 2 times) tactile stimulation of the newborn (a percussion on a sole). 7. To estimate existence and character of independent breathing. In the absence of independent breath or gasping breathing: immediately to begin mechanical ventilation by the bag and the mask with the use of 90 — 100% of oxygen (frequency 40-60 in 1 min.); initial pressure of ventilation usually is 30-40 cm of water column, at children with the immature and affected lungs and after the several first breaths inspiratory pressure has to be 20-40 cm of water column. If after mask putting on a child's face and carrying out several ventilations by the bag the thorax doesn't move, such actions are recommended: a) again to put a mask, providing its tight fitting to the person, and again to carry out ventilation; in the absence of effect consistently to perform the actions provided below, each time checking efficiency of ventilation; b) to check the position of the head; c) to check the presence of the secret in the oral cavity and if indicated to suck it; d) to try to carry out ventilation with a half-open mouth with air duct use; e) to increase inspiratory pressure. In the absence of effect it is necessary to carry out an intubation of the trachea and to exclude existence at the child of congenital anomalies. In 2 min. after initiating of mechanical ventilation by the bag and the mask it is necessary to enter a probe into the stomach to prevent aspiration and stomach dilatation. In the presence of adequate independent breath it is necessary to pass to item 9 at once. 8. To ventilate 15-30 times with 100% oxygen with the frequency of 40-60 in 1 min. 9 . To determine heart rate. If heart rate is more than 100 in 1 min. To evaluate skin color Pink or local cyanosis Central cyanosis To observe for the presence of independent breath, repeatedly to define heart rate, skin color. To stop mechanical ventilation in the presence of independent breath, to carry out short tactile stimulation and to appoint a free stream of oxygen To appoint a free stream of oxygen (at least 80 %) with a speed of 5 l/min and to evaluate the color of skin and mucous membranes. At cyanosis reduction gradually to reduce the concentration of oxygen, distancing an oxygen tube from the face of the infant. If heart rate is less than 100 in 1 min Less than 60 in 1 min. To begin (if independent breath is adequate and mechanical ventilation has not been carried out) or to continue mechanical ventilation of 100% From 60 to 100 in 1 min Doesn't increase Increa ses 7 oxygen To begin indirect heart massage of with a frequency of 90 in 1 min if mechanical ventilation has been already carried out by 100% oxygen within 15-30 s. To continue mechanical ventilation by100% oxygen with a frequency 30 per 1 min. To continue mechanical ventilation by 100% oxygen with a frequency of 40-60 per 1 min. To begin indirect massage of the heart with a frequency of 90 in 1 min, if mechanical ventilation has been already carried out, and heart rate is less than 80 in 1 min. To begin administration of drugs if the heart rate is less than 80 per minute 30 seconds after the initiating of mechanical ventilation by 100% oxygen and indirect massage of the heart Equipment which is used for the resuscitation and intensive care Resuscitation bags - standard and recommended equipment for mechanical ventilation of the newborn (MV) during reanimation: • can be filled with a stream or independenlyt; • volume shouldn't exceed 750 ml; • speed of the stream of oxygen in a bag has to be not less, than 5 l/minute; • to provide lung ventilation by 90-100% oxygen, to athe bag which is filled independently, attach the oxygen reservoir; • resuscitation bags have to be equipped with at least one of the following mechanisms of safety of lung ventilation of the newborn: - the valve of restriction of pressure (in resuscitation bags of both types); - the manometer (in resuscitation bags of both types); - the control valve over the stream (in a resuscitation bag which is filled with a stream); For carrying out MV of extremely preterms it is desirable to use the equipment with the valve which creates positive pressure at the end of an exhalation. MV of the newborns through the T-shaped adapter and the resuscitation mask, can regulate a stream of gas and limit ventilation pressure. • Use of devices of this kind provides effective and safe lung ventilation of the newborns, especially, preterms (better controls parameters of ventilation and gives opportunity to use positive pressure at the end of an exhalation). • It is possible to use NEOPUFF devices or the similar standard equipment. • The usage of such systems during resuscitation of the newborns should be preformed by the trained personnel. Resuscitation masks: • sizes of masks: "1" - for the child with the weight >2500,0 g, "0" - for the child with the weight <2500,0 g; • preferable to use masks with soft edges; • the round mask adjoins to the face of extremely preterms more hermetically, and for the larger newborns the mask of the anatomic form should be used. Equipment for the trachea intubation: • for the tracheal intubation of the newborns direct blades of the laryngoscope are used: size №0 for prematurely born and №1 for full-term newborns; 8 • it is necessary to install the laryngoscope and to check lighting system; • endotraсheal tubes without narrowing of four sizes • in case of introduction in the conductor tube, it should be fixed reliably that the end didn't get to the trachea during an intubation. Correction of metabolic disorders. 1. Measures which normalize the vascular volume of blood 1.1. The indication to the usage. • Hypovolemia: - possibility of the development of this condition should be provided for all children, a condition which doesn't improve after carried-out MV and indirect heart massage, especially, if blood loss is possible; - other symptoms of a hypovolemia - pallor, weak pulse filling and lack of signs of improvement of peripheral blood circulation, despite all resuscitation measures 1.2 Drug therapy: • 0,9% solution of sodium chloride (physiological solution); • for the correction of considerable blood loss (available clinical signs of hemorrhagic shock) there can be necessary an urgent transfusion 0 (І) II (-) erythrocytes; • solutions which contain albumin, shouldn't be used during primary resuscitation as its application is connected with the high risk of infectious neonatal mortality and morbidity. 1.3. Dosing and administration • To prepare 40 ml of 0,9% of solution of sodium chloride in syringes or the system. • Dose - 10 ml/kg. • Introduction way - intravenous slowly, for 5-10 minutes. 2. Sodium hydrocarbonate There are no sufficient scientific bases to recommend routine application of solution of sodium hydrocarbonatis for primary resuscitation of the newborns. 2.1 The indications to the administration. The probable or proved severe metabolic acidosis, during long-standing inefficient resuscitation against adequate MV. 2.2 Dosing and administration. Concentration of solution - 4,2% or 0,5 ml. To prepare 20 ml in a syringe. Dose - 4 ml/kg or 2 ml/kg. Way of introduction - in the umbilical cord vein in the presence of the return blood flow. Introduction rate slow, not quicker, than 2 ml/kg/minute. 3. Naloxone hydrochloride 3.1. The indications to the administration. • Considerable depression of breathing at the newborn after restoration of normal heart rate and skin color during MV if narcotic analgetics (opioids) were administered to the mother for the purpose of labor pain relief for the last 4 hours prior to the birth of the child. 3.2. Dosing and administration. • The recommended concentration of solution - 1,0 mg/ml. • Dose - 0,1 mg/kg. • Ways of administration: - preferably intravenous; - intramuscular - possible, but effect of the drug action will be slow; - endotracheal adminstration of naloxon is inefficient. 3.3. It is impossible to appoint naloxon to the child from mother with suspicion to drug addiction or from mother who gets long-standing supporting therapy by narcotic preparations. It can cause seizures in the newborn. 6. Clinical consequences of perinatal asphyxia: 9 - CNS: hypoxic-ischemic encephalopathy, brain edema, seizures, a syndrome of inappropriate secretion of antidiuretic hormone, cerebral spastic infantile paralysis. - Respiratory system: pulmonary hypertension, surfactant system disturbances, mekonium aspiration, pulmonary hemorrhage. - Urinary system: proteinuria, gematuria, oliguria, acute renal failure. - Cardiovascular system: insufficiency of the tricuspid valve, myocardium necrosis, arterial hypotension, left ventricular dysfunction, sinuse bradycardia, rigid heart rhythm, shock. - Digestive system: necrotic enterocolitis, hepatic dysfunction, gastric or intestinal bleeding, reduced tolerance to an enteral nutrition. - Blood system: thrombocytopenia, DIC-syndrome, polycytemia. - Metabolic disorders: Metabolic acidosis, hypoglycemia, hypocacemia, hyponatremia; increased potassium. 7. Concept about a hypoxic-ischemic encephalopathy Hypoxic-ischemic encephalopathy (GIE) - the brain disorder caused by perinatal hypoxia which is manifested by morphological functional disorders and signs of cerebral failure. Pathogenesis of HIE: - to decrease in the cerebral brain flow caused by the loss of ability to its autoregulation, arterial systemic hypotonia, reduced ejection fraction through owing to the hypoxemic injury of the myocardium, disorders of the venous outflow from the brain and increase of cerebral vascular resistance; - influence of prostaglandins, excessive synthesis of leucotriens by vessels, and also the role of the antidiuretic hormone (ADG) - localization of the affection at the brain – frontal and parietal regions the brain are mainly damaged as the result of the the thinnest arterioles less developed net of capillaries. At the chronic intranatal hypoxia typical changes in basal ganglia, thalamus occur which causes increase of adaptational possibilities of haemodynamics. Ischemia occurs as the result of the thromboses, hemorrhagic disorders, hematoencephalic barrier is damaged. These disorders lead to edema, dystrophy and focal necroses of neurons of cerebral cortex, hypocampus, and at preterms - periventricul regions; - cytotoxic edema of the brain which can be caused by the cascade emission of aminoacids first of all, a glutamate combined with metabolic acidosis (PH less than 7,0); - hemostatic disorders - low level of vitamins of K-dependent clotting factors and trombocytic dysfunction, development of the DIC-syndrome can predispose to intracranial hemorrhages. Clinical signs of HIE. Neurologic, somatic and exchange disorders: Clinical syndromes of the acute period of HIE: 1. Syndrome of increased neuroreflectory excitability is manifested by concern, disordered sleep, eruction, constant cry, increase of the muscular tone, tremor of the extremities and the chin, increased reflexes. These symptoms resolves within 5 days and corresponds to the light form of HIE. 2. Syndrome of the general depression is observed at prematurely born children owing to immaturity of CNS that is manifested by generalized depression. Characteristic signs are weakness , adinamia, decreases reflexes, muscular hypotonia. 3. Hypertension syndrome. It is observed at almost 100% cases of HIE It is manifested by the specific position of the child - the head is thrown back, extremities are flexed, the squeezed 10 cams, "brain" cry, eruction and vomiting, increased tone and a tremor of extremities, vertical and rotator nistagmus, Grefe symptom – the lag of an upper eyelid at eyeball movements with the emergence of the scleral strip which is defined in rest, a symptom of "the sun which sets" - the same, but at changed position of the body. At extreme degree of hypertension generalized clonic seizures occur. 4. The hydrocephalic syndrome occurs at the end of the acute period and is manifested by the increase in the size of the head, prevalence of the brain skull over facial part, sunken nasal bridge with an overhang of the frontal site, dilatation of subcutaneous veins over the head, and also dilatation ventricles index according to ultrasonic investigation of the brain. 5. The seizure syndrome at HIE is the most often manifested by generalized clonical-tonic seizures. Focal, multifocal and myoclonic seizures occur less frequently. 6. The comatous condition develops at brain edema and is characterized by unconsciousness, absence of physical activity, cry, emotions and reaction to the pain. Degree of severity of the coma is defined by the level of the brain affection. HIE classification: There are three GIE clinical forms of HIE: At light HIE signs of HIE are observed no more than 2-5 days. Hyperexcitability symptoms prevail. At moderate HIE disorders of the breathing rhythm, attacks of bradipnoe or bradycardia, decreased physical activity can be observed during the first hours of life. Seizures, high-pitch cry, eruction, tremor, chaotic movements appear later. Apnea attacks, symptoms of intracranial hypertension or brain edema can occur until the end of the second - the beginning of the third week of life. Severe HIE is characterized by the absence of consciousness during the first 12 hours of life, further some improvement of the condition of the child can be noted, but then, on 2 - the 3rd week, the coma and seizures occur again. Especially unfavorable sign is the development of generalized tonic seizures which are accompanied by the attacks of the secondary asphyxia (breathing and heart arrest) - these symptoms testify to the presence of intracellular brain edema with the involvement of brain stem structures. Symptoms of "weakness of shoulders", "a short neck", "a hanging-down hand", "a sharp-clawed paw", hypotonia, paralysis of the upper extremities can be evident at accompanying hypoxic-ischemic disorder of the cervical part of the spinal cord. Course of the disease and prognosis The most unfavorable symptoms are the preservation of the 3 points or lower by Apgar scale at 5 minute for the first 8 hours of the life, persistent muscular hypotonia. Later the child can suffer from cerebral paralysis, a delay of psychomotor and intellectual development, epilepsy HIE diagnostics. The diagnosis can be established by the complex of anamnestic data (the course of pregnancy and delivery, interventions in labor, drug therapy of mother during pregnancy and in labor, etc.), the analysis of dynamics of the clinical picture at the child and the assessment of results of such methods of diagnostics: - cranial ultrasonography - ultrasonic scanning of the brain through the big fontanel. This method is highly informative, noninvasive; without radial damage and gives the image of various structures of the brain in sagital and in frontal position; - computer tomography of the brain which allows to analyze a condition of the cranial bones, and brain parenchyma; - nuclear magnetic resonance and emission tomography - very exact research method, allowing to reveal pathological changes in the brain, to define differences between white and gray substance of the brain and to specify degree of a miyelinization (maturity) of various sites of the brain; - Electroencefalograpy (EEG). 8. HIE treatment 11 1. Organization of the regimen: decrease in intensity of sound and light irritants; careful inspection, swaddling and performance of procedures; minimizing of painful manipulations; "temperature protection" that prevents cooling and overheating, participation of mother in care of the child. 2. Nutrition depending upon the condition: parenteral; through the constant or disposable probe; from the small bottle. The child shouldn't starve. At parenteral administration of nutrition it is important to adhere to the regimen, not to overload with volume, to prevent hypovolemia, hypotension, dehydration, hyperviscosity; not to administer heparin as even its small doses (1-2 U/kg) increase risk of intracranial hemorrhages. 3. Monitoring supervision over the main physiological parameters: heart rate, blood pressure, rate of breathing, temperature, etc. 4. Restoration of potency of respiratory airways and adequate ventilation of lungs. 5. At HE - support of adequate cerebral perfusion, correction of pathological acidosis and other biochemical parameters (hypoglycemia, hypocalcemia, etc.); intravenous administration of 10% glucose solution (for the first days of life up to 50 ml/kg) 6. In case of comatous condition and at brain edema mechanical ventilation is indicated in the regimen of hyperventilation; barbiturates (phenobarbital 3-5 mg/kg each 6-8 hours) or sibazone 0,5 mg/kg each 8-12 hours are also administered. Barbiturates reduce increased intracranial pressure at brain edema. Intravenous dehydration with plasma, 10% albumin solution, mannitol or furosemid (at normal peripheral blood pressure) is carry out. These should not be administered if the cranial hemorrhage is present. When the symptoms of brain edema are progressing osmotic diuretics in connection with corticosteroids (dexamethasone in an initial dose of 0,2 mg/kg, then - 0,1 mg/kg with an interval of 6 hours) should be used. 8. Preparations which improve microcirculation: curantil (dipiridamol), trental, cavinton, xantinoli nicotinatis, instenon. 9. Antihypoxants: sodium oxybutiratis, piracetam, cocarboxylase, ascorbic acid, actovegin. 10. Antioxidants, stabilizers of cellular membranes: tocopherol, tocopherol acetate, selenium, unithiol. 11. Nootropic preparations (pantogam, piracetam) for the purpose of improvement of trophic processes in the brain. Drugs which improve trophic processes and miyelinization of nervous cells (cerebrolisin, encephabol, solcoseril) are administered after stabilization of the condition of the child, not earlier than after the 14th- the 20th day of life. Treatment of seizures: 1. Standard therapy for urgent stopping the esizures: 100-150 mg/kg of 20% of solution of sodium oxibutiratis intravenously slowly with 5% glucose solution, in the absence of the effect - 0,5 mg/kg of 0,5% of sibasone solution intravenously; then 15-20 mg/kg of oral phenobarbital; if the standard therapy isinefficient - barbiturates (thiopental sodium - 15 mg/kg/day intravenously slowly) under control of blood pressure and heart rate. 2. At hypoglycemic seizures - 10-20 ml/kg of 10-20% glucose solution intravenously, maintenance dose - 3-5 ml of 10% solution/kg/1 hour intravenously before level of glycemia normalizes. 3. At hypocalcemic seizures - 1 ml/kg of 10% of solution of calcium gluconate intravenously slowly. 4. At hypomagnemic seizures - 0,2 ml/kg of 25% of solution of magnesium sulfate intramuscular or intravenous administration simultaneously. 5. At the pyridoxine dependent seizures - 2 ml of 5% of piridoxin solution intravenously or intramuscularly; maintenance dose of the pyridoxine - 25 mg/kg. Haemostatic therapy: 1. Fresh frozen plasma 10-15 ml/kg intravenously 1 time per day. 2. Vikasolum 0,2-0,5 ml (2-5 mg) of 1% solution intravenously or intramuscularly. 3. Etamsylate-sodium (dicinon) - 1 ml of 12,5% solution intravenously for receiving fast effect. To enter 0,3-0,5 ml for the 3-5 days further. 12 At intracranial hemorrhage, additional measures: - subdural puncture; - neurosurgical intervention for the purpose of blood evacuation; - lumbar puncture for blood drainage from subarachnoid space for the purpose of the prevention of adhesion and secondary hydrocephaly. Complications of rescucitation Long-standing mechanical ventilation in the rigid mode causes the development of bronchopulmonary dysplasia. The most common distant consequence of MV is the retinopathy. When carrying out resuscitation actions different variants of traumatic complications are possible. Additional materials for the self-control А. Clinical cases Case 1 Infant I. was admitted in the department of pathology of newborns. From the anamnesis it is known that the child was born from the 25 year old woman, from the first pregnancy with toxicosis in 1st trimester, anemia (Hb - 98 g/l) in the second trimester, iron preparations were administered during pregnancy. In 28 weeks there was an interruption threat, was treated in the hospital. Timely delivery. Weakness of the birth activity. The fetal hypoxia occurred, stimulation by oxytocin. The first period of labor - 8 hours, the second - 25 minutes, a waterless period - 10 h. 20 min., mekonium in waters. Birth weight – 3300 g, length - 51 cm. Assessment by the Apgar scale - 6-8 points. The infant cried after suction of mucus. After the birth the condition of the infant is moderate caused by neurologic symptoms: tremor of hands, chin. Other physical investigation is unremarkable. At the 4-th day the condition of the child deteriorated by the neurologic symptoms, and the child was transferred to the hospital. At admitting to the hospital the condition of the child is severe. Skin is with a grayish colour, acrocyanosis, marble shade. Umbilical wound is dry. Hyperestezia. Pharynx is pale. Breathing is puerile. Tones of heart are rhythmical, heart rate 152/min. The abdomen is soft, the liver is 3 cm below the right costal arch, and the spleen isn't palpated. Stool is yellowish with undigested lumps of food. In the neurologic status - crying monotonous, big fontanel is 2,0*2,0 cm, pulse, sagital fissure is opened. Grefe symptom is positive, transient strabismus. Reflexes of the newborn are decreased, a muscular tone with a tendency to hypotonia, tendon reflexes are S=D, moderate activity. Tremor of hands is noted at the tension. Seizures weren't evident at inspection. Complete blood count: Hb – 192 g/l, erythrocytes – 5,8*1012/l, colour index – 0,98, leukocytes – 12,5*109/l, bands – 10%, segments – 56%, еosinophils – 1%, basophils – 1%, lymphocytes– 29%, ESR – 6 mm/h. Biochemical analysis of blood: the general protein – 62 g/l, bilirubin: the indirect – 51 mcmol/l, direst – absent, urea - 3,3 mmol/l, potassium - 6 mmol/l, sodium 136 mmol/l, calcium - 1,1 mmol/l, phosphorus - 2,32 mmol/l. Ultrasonic investigation of the brain at the age of 8 days: smoothed drawing of sulci and gyri. Frontal horns are expanded to 6 mm. Depth of lateral ventricles at the level of bodies (S=D) is 7 mm (normal - up to 5 mm). Local echogenous inclusions in the subcortical ganglia. Cyst of the vascular plexus about 3 mm is noted. The echogenity of the periventricular sites is moderately encreased. 13 Questions: 1. What is your preliminary diagnosis? 2. What additional investigations need to be carried out for the confirmation of the diagnosis? What are the possible results? 3. What factors indicated the development of this pathology in the newborn? 4. What features of the hematoencephalic barrier at the newborns? 5. What compensatory mechanisms are developing at acute hypoxia of the newborn? 6. Name the cellular composition of the spinal liquid of the newborn. 7. Should this patient have consultation of the ophthalmologist? If so, what changes are possible? 8. Administer treatment. 9. What drugs are used for the dehydration at treatment of brain edema? 10. What is prognosis for this child? B. Tests Question 1. In the child who has suffered a severe hypoxic ischemic injury, which of the following is true? A. Liver and kidney damage are irreversible B. Isolated brainstem function might be preserved C. CT scans do not reveal abnormalities until after 1 mo following Injury D Intracranial pressure monitoring improves outcome Answer B. Explanation: The brainstem may be preserved in the presence of cortical cell death. This is a controversial point in the discussion of brain death. Today we agree on the legal definition of whole brain death, which includes the brainstem and obviously precludes effective spontaneous ventilation. Cortical brain death proponents want to recognize cortical death alone as the criterion for legal death. The controversy has not been resolved. Question 2. The best description of the Apgar score is that it: A. Accurately predicts who will develop cerebral palsy B. Assesses neonates in need of resuscitation C. Accurately predicts a low umbilical cord pH D. Is unaffected by maternal opiate pain relief E. Accurately predicts neonates who will die in the neonatal period Answer B. Explanation: The Apgar score helps to rapidly assess the need to resuscitate neonates after birth. Although it has some value in predicting neonatal mortality and cerebral palsy, it has a poor positive predictive value. Most children with cerebral palsy have had normal Apgar scores, while neonates with low Apgar scores do not universally get cerebral palsy. Question 3. A term female is born by spontaneous vaginal delivery to a primiparous woman who received two doses of meperidine 30 min and 2 hr prior to an abrupt delivery. The baby is apneic and limp. The most important, immediate management is to: A. Administer naloxone in the umbilical vein B. Perform bag-mask ventilation C. Administer naloxone in the endotracheal tube D. Begin chest compressions E. Obtain a cord pH 14 Answer B. Explanation: Apnea from any cause is treated with securing apatent airway and instituting ventilation. If bag mask ventilation is ineffective, endotracheal intubation should be performed. Naloxone (Narcan) can be given only after the baby is ventilated. Question 4. Successful ventilation is determined by all of the following except: A. Zero reading of end-tidal CO2 measurement B. Pink color C. Rising heart rate D. Symmetric breath sounds E. Good chest rise Explanation: Indeed, one expects that with a successful intubation and ventilation, the endtidal (exhaled) CO2 will rise dramatically. This is now used in many neonatal resuscitations. Complete cardiac onset with poor perfusion may also cause a low end-tidal CO2. Question 5. An infant has the following findings at 5 min of life: pulse, 130/min; cyanotic hands and feet; good muscle tone; and a strong cry and grimace. This infant's Apgar score is: A. 7 B. 8 C. 9 D. 10 Answer C. Explanation: One point in the Apgar score is taken off for color. Question 6. A girl is born via stat cesarean section to a 34-year-old mother whose pregnancy was complicated by hypertension and abnormal fetal heart monitoring. At delivery she is covered in thick, green meconium and is limp, apneic, and bradycardic. Which of the following is the best first step in her resuscitation? A. Administer IV bicarbonate. B. Administer IV naloxone. C. Initiate bag-and-mask ventilation. D. Initiate chest compressions immediately. E. Intubate with an endotracheal tube and suction meconium from the trachea. Answer E. An attempt is made to remove the meconium from the oropharynx and the airway prior to initiation of respirations. Ideally, the obstetrician will begin suctioning the meconium upon delivery of the head, and the pediatrician will further remove meconium with an aspirator or through endotracheal intubation with suction. Ventilation is initiated after meconium is removed. The goal is to remove airway meconium and to prevent its aspiration into the small airways where ventilation-perfusion mismatch may occur with deleterious effects. Question 7. A term male is delivered vaginally to a 22-year-old mother. Immediately after birth he is noted to have a scaphoid abdomen, cyanosis, and respiratory distress. Heart sounds are heard on the right side of the chest, and the breath sounds seem to be diminished on the left side. Which of the following is the most appropriate next step in his resuscitation? A. Administer IV bicarbonate. B. Administer IV naloxone. C. Initiate bag-and-mask intubation. 15 D. Initiate chest compressions immediately. E. Intubate with an endotracheal tube. Answer E. The case describes diaphragmatic hernia. As a result of herniated bowel contents into the chest, these children often have pulmonary hypoplasia. Bag-and-mask ventilation will cause accumulation of bowel gas (which is located in the chest) and further respiratory compromise. Therefore, endotracheal intubation is the best course of action. Question 8. A 37-week-gestation boy is born after an uncomplicated pregnancy to a 33-yearold mother. At birth he was lethargic and had a slow HR. Oxygen was administered via bag and mask, and he was intubated; his HR remained at 40 bpm. Which of the following is the most appropriate next step? A. Administer IV bicarbonate. B. Administer IV atropine. C. Administer IV epinephrine. D. Administer IV calcium chloride. E. Begin chest compressions. Answer E. If the HR is still less than 60 bpm despite PPV with 100% oxygen, then chest compressions are given for 30 seconds. If the HR is still less than 60 bpm, then drug therapy (usually epinephrine) is indicated. Question 9. At 43 weeks’ gestation, a long, thin infant is delivered. The infant is apneic, limp, pale, and covered with “pea soup” amniotic fluid. The first step in the resuscitation of this infant at delivery should be A. Suction of the trachea under direct vision B. Artificial ventilation with bag and mask C. Artificial ventilation with endotracheal tube D. Administration of 100% oxygen by mask E. Catheterization of the umbilical vein The answer is A. Infants who are postmature (more than 42 weeks’ gestation) and show evidence of chronic placental insufficiency (low birth weight for gestational age and wasted appearance) have a higher-than-average chance of being asphyxiated, and passage of meconium into the amniotic fluid thus places these infants at risk for meconium aspiration. To prevent or minimize this risk, these infants should have immediate nasopharyngeal suction as their heads are delivered. Immediately after delivery and before initiation of respiration, their tracheas should be carefully and thoroughly suctioned through an endotracheal tube under direct vision with a laryngoscope. Afterward, appropriate resuscitative measures should be undertaken to establish adequate ventilation and circulation. Artificial ventilation performed before tracheal suction could force meconium into smaller airways. Question 10. A 42-week gestation neonate is born by cesarean delivery following repeated fetal heart rate decelerations. At rupture of membranes, thick meconium was noted. The infant has no respiratory effort but slight movement and a heart rate of 90 beats per minute. Of the following,which is the first intervention? A pass an umbilical artery catheter to measure pH and Po2 B start bag-and-mask ventilation with 100% oxygen C suction the mouth and trachea to remove the meconium D intubate the trachea and begin ventilation with 100% oxygen 16 E establish monitoring with ECG and pulse oximeter Answer C. After birth, intubation and tracheal suction decrease the risk of developing meconium aspiration syndrome in infants who are not vigorous at birth. The infant described in this case is not vigorous (depressed respirations, depressed muscle tone, and/or a heart rate < 100 beats per minute), thus endotracheal intubation with suctioning to remove the meconium is indicated after the infant is delivered. Question 11. A 2,9-kg term male infant is born to a mother who developed polyhydramnios at 34 weeks' gestation. At birth, the Apgar scores were 9 and 9. The infant develops choking and cyanosis with the first feed. In addition, is unable to place a nasogastric tube. What is the most likely diagnosis? A.Choanal atresia B.Laryngomalacia C.Esophageal atresia D. Tracheal atresia E. Respiratory distress syndrome Question 12. In the 43rd week of gestation a long, thin infant was delivered. He is apneic, limp, pale, and covered with "pea soup" amniotic fluid. The first step in the resuscitation of this infant at delivery should be: A.Suction of the trachea under direct vision B.Artificial ventilation with bag and mask C.Artificial ventilation with endotracheal tube D.Administration of 100\% oxygen by mask E.Catheterization of the umbilical vein Question 13. A full-term baby was born with body weight of 3200 g, body length of 50 cm, Apgar score - 8-10 points. What is the optimum time for the first breast-feeding? A.First 6 hours B.First 24 hours C.First 30 minutes D.First 48 hours E.After 48 hours Question 14. The child had Apgar scale of 8-9 points at time of birth. When should he be breastfed? A. Right after birth B.After processing of the umbilical cord and performing profilaxis of gonoblennorea C.After umbilical cord processing D.30 minutes after birth E. 2 hours after birth Question 15. What medication should be administered to the baby, born by Caesarean section, if he is at asphyxia and independent breathing is absent on the first minute of life? A.Etimizole B.Caffeine sodium benzoate C.Cordiamin D.Sodium bicarbonate E.Naloxone a hydrochloride Question 16. Newborn child experienced intranatal asphyxia. While suctioning the mucus from the upper respiratory tract miconium is reveaked. Independent breath is absent. The further actions of 17 neonatologist provide: A.External heart massage B.Tracheal intubation, sanation of respiratory tract C.Application of 100 %oxygen. D.Adrenaline introduction. E.Tactile stimulation of breathing. Question 17. After birth the child is pale, has arrhythmic breathing which doesn't improve against oxygenotherapy. Pulse is weak, tachycardia is observed, arterial pressure it barely measured. Edema is absent. What is the most likely cause of these symptoms? A.Congestive heart failure B.Intracranial hemorrhage C.Intrauterine sepsis D.Asphyxia E.Intrauterine pneumonia Question 18 . Overterm infant, which was born at 43 weeks` gestation, has apnoe, pallor, the child is covered by greenish amniotic fluid. The first steps in the newborn resuscitations include: A.Mechanical ventilation using the mask and a bag B.Mechanical ventilation using the endotracheal tube C.Application of 100 % of oxygen D.Umbilical vein cateterisation E.Aspiration of tracheal contents Question 19. The newborn which had asphyxia at the birth had apnea and the bradycardia (heart rate 70 per minute). Mechanical ventilation using 100 % oxygen with application of a mask and a bag of Ambu was applied urgently. In 30 seconds the heart rate without improvement. What should be the next step of resuscitatory measures? A.Undirect heart massage B.Tactile stimulation C.Continue ventilation D.Sodium hydrocarbonate intravenously E.Epinefrin intravenously Question 20. The term infant with cord encirclement round the neck since 1 minute of life has total cyanosis, apnea, heart rate - 80 in minute, muscular hypotonia and absent reflexes. Signs of meconium aspiration are absent. After sanation of respiratory tract breathing hasn’t restored. Your following action? A.Adrenaline introduction B.Etamzilat introduction C.Mechanical ventilation using the mask of 100 % О2 D. Intubation of trachea and mechanical ventilation E.Irritation of the skin along the spinal cord 4. LITERATURE FOR STUDENTS 1. Nelson Textbook of Pediatrics. - 18th ed. / Ed. by R. Kliegman et al.-Philadelphia: Saunders Co, 2007.- 3146 p. 2. Pediatry. Guidance Aid / За ред. О.В. Тяжка; О.П. Вінницька, Т.І. Лутай – К. : Медицина, 2007 . – 158 с. 3. Current Pediatric Diagnosis & Treatment (CPDT). - 18th ed./ Ed. By W.W.Hay et al. - The McGraw-Hill Companies. – 2006. 4. Current pediatric therapy -18th ed. / Ed. by F.D.Burg et al. - Elsevier Inc. – 2007. 18 5. Nelson Essentials of Pediatrics -5th ed. / Ed. by B.S.Siegel, J.J.Siegel. - Elsevier Inc. – 2007. 6. Examination of the Newborn. A Practical Guide / Ed. by Helen Baston and Heather Durward. - the Taylor & Francis e-Library. - 2005. 7. Fetal and neonatal secrets. - second edition . / Ed. by R.A.Polin, A.R.Spitzer. - Elsevier.2006. 8. Key Topics in Neonatology / Ed. by R.H. Mupanemunda, M. Watkinson. - Oxford Washington DC. -1999. Performed by ass. Vaculenko L.I., ass. Tkachenko N.P. Approved “_____”____________20____y. Сhief of the department, professor Protocol №_____ V. A. Kondratyev Reconsidered Approved “_____”____________20____р. Сhief of the department, professor Protocol №_____ V. A. Kondratyev Reconsidered Approved ““_____”____________20____р. Сhief of the department, professor Protocol №_____ V. A. Kondratyev Reconsidered Approved “_____”____________20____р. Сhief of the department, professor Protocol №_____ V. A. Kondratyev Reconsidered Approved ““_____”____________20____р. Сhief of the department, professor Protocol №_____ V. A. Kondratyev Reconsidered Approved “_____”____________20____р. Сhief of the department, professor Protocol №_____ V. A. Kondratyev 19