Can the response to mood stabilizers be predicted in - HAL
advertisement

Can the response to mood stabilizers be predicted in bipolar disorder?
Pierre Alexis GEOFFROY1,2,3,4, Frank BELLIVIER4,6,7, Marion LEBOYER1,3,4,5, Bruno ETAIN1,3,4
1INSERM,
U955, Creteil, 94000, France, 2Psychiatry department, Lille Nord de France University, CHRU Lille, F-59000 Lille,
France, 3AP-HP, H. Mondor - A. Chenevier, Psychiatry department, Creteil, 94000, France, 4FondaMental Foundation, Creteil,
94000, France, 5Paris Est University, Creteil, 94000, France, 6AP-HP, GH Saint-Louis - Lariboisiere - Fernand Widal,
Neurosciences department, Paris, France, 7Paris-7 Paris-Diderot University, UFR Medecine, Paris, France
TABLE OF CONTENTS
1. Abstract
2. Introduction
3. Methods
4. Phenotypic features and definitions
4.1. Which phenotype should be assessed for subjects with BD?
4.2. How should treatment response phenotypes be assessed?
5. Pharmacogenomics of mood stabilizers
5.1. Lithium
5.1.1. Linkage studies on the response to lithium
5.1.2. The candidate gene approach
5.1.2.1. The inositol pathway
5.1.2.2. The circadian signaling system
5.1.2.3. The neurotransmitter system: serotonin, dopamine and GABA pathways
5.1.2.4. The BDNF/TrkB signaling pathway
5.1.2.5. Other signaling pathways
5.1.3. Genome Wide Association Studies (GWAS) on the response to lithium
5.2. Pharmacogenomics of other mood stabilizers
5.2.1. Valproate (VPA)
5.2.2. Lamotrigine (LTG)
5.2.3. Atypical antipsychotics (AAP)
6. Summary and perspectives
7. Conclusion
8. References
1. ABSTRACT
Bipolar disorder (BD) is a severe chronic multifactorial disease that requires maintenance therapy with mood
stabilizers (MS). Even with medications, the rate of response among patients with BD is low and the risk of relapse is high.
Therefore, in this context of the urgent need for reliable and reproducible predictors of individual responses to MS,
pharmacogenetics research is expected to provide helpful progress. Most pharmacogenetic studies of MS have focused on the
response to lithium with several good putative candidate genes but informative results are sparse. There have been few studies on
valproate, lamotrigine or atypical antipsychotics. Overall, the results of pharmacogenomics studies have not provided sufficient
data to change daily practices in BD significantly and further investigation is warranted to identify highly relevant genetic
predictors of response their roles. Although progress still remains to be made, the clinical assessment of a subject including the
identification of specific individual phenotypic and pharmacogenetic characteristics is likely to become a powerful instrument for
the development of personalized therapies.
2. INTRODUCTION
Bipolar disorder (BD) is a chronic multifactorial psychiatric disorder that is characterized by recurrent alternating
episodes of mania/hypomania and depression interspaced with euthymic periods variably affected by residual symptoms and
dysfunction (1). BD causes impairment in functioning and health-related quality of life, and BD patients require maintenance
therapy (2). The lifetime prevalence of BD is about 1% for the traditional BD I subtype and up to 6.5% if all BD spectrum
subtypes are included; thus, it is evidence that BD is a major public health problem (3,4). Indeed, BD is seventh most major cause
of disability-adjusted life-years according to the World Health Organization (WHO) (5).
The etiological determinants of BD remain poorly understood; similarly, the mechanisms of action of psychotropic
drugs have not been described in detail, and indeed the exact targets are still to be definitively identified. Current guidelines
1
advocate the use one of a group of variably similar treatment algorithms for all patients, such that the clinical, pathophysiological,
and lifetime heterogeneity of BD is not taken into accounts, because of the lack of evidence (2). Thus, personalized therapeutic
strategies with targeted interventions —taking into account both individual characteristics and the characteristics of the clinical
expression of the disorder in a given individual— are clearly required to improve prognosis. Pharmacogenomics can be exploited
to identify key biomarkers and therefore drive innovation in this field of personalized medicine.
Numerous studies have attempted to identify genetic markers that could be used to predict drug efficacy and safety in
several fields of medicine. Pharmacogenetics is “the study of variability in drug response due to heredity”, and may thus be
contribute to the development of ‘personalized’ treatment strategies in medicine, and including BD. However to date, there is
only one US FDA-approved commercial pharmacogenetic test available (Roche Diagnostic, AmpliChip CYP450) which allows
genotyping for the two cytochrome P450 genes (CYP2D6 and CYP2C19). Using this chip, patients can be genotyped to help
predict the metabolizer status of patients, which may influence choice and dose of antipsychotic or antidepressant medication (6).
No clear genetic biomarker for use in routine clinical care in BD has been described.
This is particularly unfortunate because BD patients show a low rate of response, a high risk of relapse and several side
effects to MS that are unfortunately not predictable. Indeed, survival analysis of BD patients indicates a 5-year risk of relapse into
mania or depression of 73% despite continual and adequate MS medication (7). Even for those who do not relapse, considerable
affective morbidity is observed (7). The large EMBLEM prospective study with BD I patients shows that 64% achieved
remission and 34% achieved functional recovery at 2 years (8). A naturalistic observation study of the response to MS described
very low rates of full response to individual MS: lithium 30%, carbamazepine 0%, valproate 13%, lamotrigine 11%, and
olanzapine 25% (9). The predictors were few and uncertain: lithium responders were more likely to be bipolar II with earlier
onset of illness, and responders to valproate presented higher rates of psychosis (9). Various evidence indicates that the response
to long-term lithium treatment is a familial trait and clusters in families (10). Also, the mode of inheritance of BD responsive to
lithium appears to conform to a recessive model with sex-specific penetrance of transmission (11). Evidence for such heritability
is consistent with the relevant genes exerting a high-magnitude effect on the response to long-term lithium treatment. Thus, the
response to long-term prophylactic treatment with mood stabilizers (MS) has been suggested to be a clinical trait that could be
exploited to identify homogeneous subgroups of BD and to map genes relevant to both treatment response and BD itself (12–15).
Therefore, informative and helpful results are expected from pharmacogenomics research in this context of the urgent need to
find reliable and reproducible predictors of individual responses to MS and MS safety (14,16–18).
We review the current state of, and perspectives for, pharmacogenetic research on MS treatments in BD. First, we
consider issues pertaining to the diagnosis of BD patients, sample selection and definitions of treatment response phenotypes
used in various pharmacogenetic studies. Then, we review existing evidence for genetic predictors of the response of BD patients
to MS treatment. Finally, we discuss the possible challenges and future directions for pharmacogenetics in BD.
3. METHODS
We conducted in March 2013 an extensive review on the pharmacogenomics studies exploring MS treatment in BD.
The publications were obtained from the PubMed electronic database. The literature search was performed using the Mesh
heading: “Bipolar Disorder” AND ("genetics" OR "gene" OR “pharmacogenomics” OR “pharmacogenetics”) AND ("mood
stabilizer" OR "lithium" OR "valproate" OR "valproic acid" OR "lamotrigine” OR "carbamazepine” OR "oxcarbazepine” OR
"topiramate” OR "gabapentin” OR "antipsychotic”). We also used the related articles function of the PubMed database, the
reference list of retained studies and searched Google Scholar to identify additional articles. We included only published data
written in English.
4. PHENOTYPIC FEATURES AND DEFINITIONS
A research in pharmacogenetics is confronted by a methodological question: should the response to MS treatment in all
BD subjects be studied, or should phenotypically defined subgroups of subjects with BD be studied?
The genetic and phenotypic heterogeneity of BD clearly cloud the identification of its biological determinants (19).
The use of valid and consensual definitions for all steps of studies is essential for reliable and comparable results to be obtained.
Rigorous definitions of the probands and clear criteria for the definition of treatment are needed to detect causative determinants
of differences in response to medication.
4.1. Which phenotype should be assessed for subjects with BD?
Investigations of drug responders (20) and the comparison of patients responsive to different drugs (21) have led to
promising results. Responsive patients that differ with respect to course of the disease, comorbidity and family history, may
represent distinct subtypes of BD. There is now evidence to suggest that lithium-responsive BD is a core bipolar phenotype (20):
responders to lithium show a family history of BD and a familial response to lithium consistent with genetic factors having a
prominent role (20). Also, family histories and some clinical characteristics differ between responders to lithium and responders
to other MS (20).
2
BD is a broad-large spectrum with wide range of symptoms. Defining intermediate phenotypes, or homogeneous
subgroups within the BD population may be useful. Indeed, the early genetic research with the whole BD spectrum, or even with
the traditional BD I subgroup, failed to obtain significant and relevant results (19). Consequently, recent studies focus on more
homogeneous subgroups, and there has been substantial effort directed towards phenotypic refinement. The purpose of
phenotypic refinement is to select subgroups that differ from the whole BD population as concerns clinical presentation, course
of the disease, family history, comorbidities and/or possibly long-term response to treatment (22). Alda proposed a classification
based on three main subtypes of BD: (1) classical, (2) psychosis spectrum and (3) 'characterological' which includes cases with
distinct clinical characteristics and specific patterns of drug treatment response that might lead to more targeted treatment (23).
Such phenotype selection of BD populations aims to increase the probability of identifying genes of interest. They
highlight the importance of careful diagnostic assessment of BD cases, with attention to specific clinical features, family history,
comorbidities and clinical course as these factors may be closely linked to the treatment response phenotype.
4.2. How should treatment response phenotypes be assessed?
Assessment of treatment response phenotypes is central to identifying the role of genetic factors in determining a
subject’s response to a drug or the onset of adverse drug reactions (ADR). The definitions of treatment response used in the
literature are often not clear and divergent between pharmacogenetic studies. Defining treatment response phenotypes is expected
to be highly complex, largely because the clinical quantification of the response to treatment is complex.
The simplest phenotype is dichotomous (responders/non-responders) and has been used in most pharmacogenetic
studies of MS (14). Nevertheless, a binary trait of this type does not allow correct measurement of the response to a drug, which
is, constitutively, a quantitative trait. Indeed, such binary measurement does not reflect the clinical reality because most patients
show partial responses and very few of presented a full response to MS (9). If a categorical approach is used, partial responses to
a drug can be usefully assessed in addition to the classical traits of responders/non-responders. Applying a dimensional approach,
the response to MS is studied as a quantitative trait, and this may facilitate the identification of genetic variants and their
expression associated with a wide range of intermediate phenotypes. The dimensional approach allows the degree of variation in
the treatment response phenotype to be studied, and this contrasts with the dichotomous approach that only the two extreme
points of the dimensional gradient into account. Moreover, combining assessment of the response to treatment as measured from
the improvement of BD symptoms, with assessment of treatment side effects, as with the Clinical Global Impressions Scale
(CGI), might be useful to separate out the two effects (24). The method of “extreme discordant phenotype” (EDP) may increase
the statistical power and consequently the probability of detecting gene variants associated with drug efficacy or toxicity (25).
Alternatively, individual trait values, for example treatment response, can be used as indices for phenotype selection, and
selective genotyping has been proven to be effective for mapping quantitative trait loci (QTL) (26).
The definition of treatment response is complex, especially in BD: several factors have to be considered, including the
long-term response to MS, the severity and the duration of episodes before and after the introduction of the MS, the presence of
possible confounders, for example multiple pharmacotherapy, and the degree of compliance. Thus, stringent definitions are tricky
to establish, and several tools have been proposed. The average Affective Morbidity Index and the Illness Severity Index are both
analytical tools (27) (28). They each provide a quantitative evaluation of the improvement under MS and take into account both
severity and duration of episodes before and after the introduction of MS treatment. However, they suffer limitations because
they do not take the presence of confounders into account, such as compliance or poly-pharmacotherapy. Grof et al. recently
compared response to long-term lithium treatment in bipolar relatives of BD lithium responders and BD controls, and proposed a
more complete rating scale referred to as the “Alda scale” (10). It is a quantitative scale for measuring the degree of improvement
under MS taking the presence of confounders into account. As well as allowing improvement due to MS only to be observed, it
also permits both an intermediate phenotype approach (partial response to MS) and an EDP approach (10). This approach
involves rating the degree of response on a 10-point scale (“A” criteria) and the number of episodes off the treatment, the
frequency of episodes off the treatment, the duration of treatment, the compliance during period (s) of stability, and the use of
additional medications during the periods of stability (“B” criteria); a total score from 0 to 10 is then obtained by subtracting B
from A criteria (10).
However, irrespective of the definition used, we observed that the rate of response to various MS treatments in
monotherapy is always close to 50% (and about 30% for placebo), with an incremental benefit of about 20% when adding a
second MS agent (29). Thus, treatment refractoriness in BD remains a substantial medical challenge. We believe therefore that it
is very important to identify markers that are predictive of the response to MS treatments; this may involve the identification of
genetic variant patterns that can be used to help choose between different molecules available as treatment in routine practice.
5. PHARMACOGENOMICS OF MOOD STABILIZERS
5.1. Lithium
3
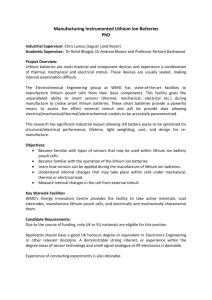
Lithium salts are the best studied MS and remain a cornerstone of treatment in BD. Pharmacogenetic studies have for
the most part focused on the response to lithium prophylaxis as a way to define a more homogeneous population (Table 1).
5.1.1. Linkage studies on the response to lithium
Linkage studies on the response to lithium were the first to generate relevant and informative results. Analysis of the
Faroese population with eight lithium-responsive BD probands provided evidence of increased haplotype sharing on the distal
part of chromosome 18q23, confirming the preliminary findings for this region by Freimer et al. (30). A linkage study focused on
this region of chromosome 18: in the sample of lithium-responsive BD probands including only unilineal families, two
chromosomal regions with modestly positive LOD scores were found at D18S53 and at D18S61 for maternal and paternal
pedigrees, respectively (31). Further linkage studies using a temperament-based measure (cyclothymic temperament) as a
quantitative intermediate phenotype found the highest linkage on chromosome 18p11 and weaker linkage for chromosomes 3 and
7 (32). Consequently, chromosome 18 is a potential region of interest and quantitative measures may lead to the detection of loci
for BD and maybe for the response to lithium. Work with a very large pedigree derived from a homogeneous population in
Quebec from Saguenay-Lac-St-Jean area found the chromosome 12q23-q24 region to be linked with the response to lithium in a
BD population (33). Linkage to chromosome 12q24 was confirmed later in a larger study in the same population, and other
regions of lower interest were found on chromosomes 2, 5, 7, 9, 10, 17 and 20 (34). Evidence for linkage was found in 31 BD
families identified as excellent lithium responders with loci on chromosomes 15q14 and 7q11.2 (35); considering response
phenotype, this study also suggests that chromosome 7q11.2 may be more involved in the response to lithium than chromosome
15q14, which was implicated in the etiology of BD (35). These observations highlight how it is important to pay attention to the
interpretation of studies of this type. Indeed, comparing responders to non-responders allows treatment response genes to be
identified, whereas studying BD responders alone only allows conclusions about genes associated with the disease. A very
relevant recent linkage study considered 36 families recruited through responsive probands to long-term lithium treatment; it
involved an initial linkage study followed by fine mapping and gene expression analysis. Exploiting these two complementary
strategies, the authors found evidence of linkage to lithium-responsive BD in 3p25, 3p14 and 14q11 regions; they also found
significantly deregulated synaptic and mitochondrial genes in these regions (36).
These linkage studies on the response to lithium generated enthusiastic results and should also be performed in the
future on the “non-response” phenotype. Moreover, some methodological issues, such as spontaneous remission of the illness,
will have to be addressed.
5.1.2. The candidate gene approach
5.1.2.1. The inositol pathway
Selecting candidate genes for pharmacogenetic investigation is difficult because the exact mechanism of action of
lithium remains unclear (37). Lithium inhibits the activity of several enzymes including those involved in the
phosphatidylinositol cycle and in phospholipase C signal transduction that may be responsible for mood stabilization. Williams
RS et al. reported that the effects of MS (including valproate and carbamazepine as well as lithium) are mediated through action
on inositol depletion (38). They demonstrate that all three drugs inhibit the collapse of sensory neuron growth cones and increase
growth cone area, and that this action is reversed by inositol (38). Consequently, numerous candidate gene studies on the
response to lithium prophylaxis have addressed inositol-related genes.
The hypothesis that inositol polyphosphate 1-phosphatase (INPP1) in the phospholipase C signaling pathway is a
putative target of lithium has been investigated: several pharmacogenetic studies have tested for associations between
polymorphisms in the INPP1 gene and the response to lithium of BD patients. An association between the C973A variant of the
INPP1 gene and good efficacy of lithium in BD has been reported (39), but not subsequently confirmed by Michelon et al. (40).
Candidate genes studies have drawn attention to the myo-inositol monophosphatase 2 (IMPA2) that encodes an
enzyme of the phosphatidylinositol signaling system and is inhibited by lithium (41). One study compared good responders to
lithium treatment with the poor responders among 237 parent-offspring trios, 174 cases and 170 controls: this study reported a
trend for significant associations in predicting the response to lithium treatment for two polymorphisms (41). The two
polymorphisms of IMPA2 on chromosome 18p11.2 were confirmed in a supplementary study (42). Two studies found no
association between the polymorphisms of myo-inositol monophosphatase 1 (IMPA1) on chromosome 8q21.13-21.3 with
variation in the response to lithium treatment in cases of BD (42,43). Generally, preliminary studies implicate several enzymes
related to inositol phosphate metabolism and therefore the genes of this pathway may be suitable targets for studies of the action
of lithium.
Diacylglycerol kinase eta (DGKH) is a key protein in the lithium-sensitive phosphatidyl inositol pathway responsible
for the recycling and degradation of diacylglycerol (DAG). A recent genome-wide association study implicates the diacylglycerol
kinase eta gene (DGKH), and found the strongest association signal at a marker within the first intron of DGKH (44). However,
study of a sample of 199 Sardinian BD patients characterized for the response to lithium therapy did not replicate the association
with DGKH polymorphisms (45), and an additional study in 91 subjects characterized for lithium response did not find an
association but the sample was too small to detect anything other than large, strong effects (46).
4
Several studies have tested the phospholipase C-gamma 1 (PLCG1) gene that codes for a gamma-1 isozyme of
phospholipase (PLC), an enzyme of the inositol pathway second messenger system. One study reported a positive association for
one PLCG1 polymorphism in 136 excellent lithium responders compared to 163 controls (47). The same authors screened the
PLCG1 gene for functional polymorphisms and identified three polymorphic sites in three different exons (exons 9, 26, 31);
however, none of the markers was found to be associated with BD in a sample of 133 excellent responders to lithium and 99
healthy controls (48). Because of the absence of a comparison non-responder group, these two studies only show that the PLCG1
gene is associated with BD. A recent study tried to confirm the findings that bipolar patients with an excellent response to lithium
treatment have a higher frequency of a specific dinucleotide repeat allele in the PLCG1 genomic region; however, this was not
replicated in a sample of Norwegian lithium-treated bipolar patients sub-classified as lithium responders, non-responders, or
partial-responders/unclassified (49). Only a PLCG1-8 repeat was more frequent among lithium responders than controls when
analysing according to presence or absence of different dinucleotide alleles (49). Although further studies are needed to explain
these contradictory results, work in the inositol pathway shows promise and generates helpful findings.
5.1.2.2. The circadian signaling system
There is interest in variants of genes associated with the molecular clock, as some of these genes encode enzymes that
are inhibited by lithium, for example glycogen synthase kinase 3 alpha and beta (GSK3α and GSK3β). Lithium acts on these
enzymes either by direct inhibition or indirectly by regulating other mechanisms like the formation of a signaling complex
comprised of beta-arrestin 2 (βArr2) and Akt. (50). Benedetti et al. studied the association of GSK3β (-50 T/C) polymorphism
with the therapeutic response to lithium among 88 bipolar type I patients: the recurrence index for homozygotes for the wild
variant (C/C) did not change under treatment, whereas carriers of the mutant allele showed improvement. This thus suggests that
the long-term response to lithium in bipolar illness is influenced by the GSK3β -50 T/C polymorphism (51). However,
contradictory results have been reported: one study concluded that this polymorphism is not related to the response to
prophylactic lithium (52) and another found no association (40). GSK3β also phosphorylates and stabilizes the orphan nuclear
receptor REV-ERBα, one of the principal components of the circadian rhythm system that is involved in the cyclic regulation of
Brain and Muscle Arnt-like protein-1 (BMAL1). Lithium induces degradation of REV-ERBα and BMAL1 gene expression,
implicating REV-ERBα as a target of lithium in its mechanism of action (53). The association of the gene encoding for REVERBα (NR1D1) and the response to lithium prophylaxis in BD patients has been investigated in a sample of 199 Sardinian BD
patients characterized for the response to lithium therapy; the interaction analysis did not show any significant effect of any
NR1D1 polymorphisms (45). However, more recently, Campos-de-Sousa et al. observed a significant association between the
variant rs2314339 in NR1D1 and the response to lithium (54). Further evidence of a role for REV-ERBα in the therapeutic
mechanism of lithium has recently been described. McCarthy et al. conducted a candidate gene association study for 16 variants
in seven circadian clock genes and the response to lithium of 282 Caucasian patients with BD (55). They found that a variant in
the promoter of NR1D1 (rs2071427) and a variant in cryptochrome-1 (CRY1; rs8192440) were nominally associated with the
response to lithium (55). Also, GSK3β and NR1D1 genotypes considered together predicted the response to lithium robustly and
additively; the response was proportional to the number of response-associated alleles (55).
Glucocorticoid receptors are regulators of the circadian rhythm. A polymorphism of the glucocorticoid receptor gene
(NR3C1) on chromosome 5q31-32 is associated with lithium responder status (56). Although the mechanism of action of lithium
is not understood, it clearly interferes with the expression of circadian genes and this is involved in its mood stabilizing effect
(53). These first results from pharmacogenetic studies with the circadian system are promising but still preliminary and further
replications are required.
5.1.2.3. The neurotransmitter system: serotonin, dopamine and GABA pathways
Serretti et al. explored the dopamine, GABA and serotonin pathways and did not find any association between the
efficacy of lithium and polymorphisms at the genes of any of the following: the D2 receptor (57), the D3 receptor (58), the D4
receptor (57), the γ-aminobutyric acid (GABA) type A receptor α-1 subunit (57), and the 5-HT2A, 2C and 1A receptors (59). The
same authors found an association between a functional polymorphism in the upstream regulatory region of the serotonin
transporter gene (5-HTTLPR) and the prophylactic efficacy of lithium: 5-HTTLPR s/s variants were associated with a worse
response to lithium than either l/s and l/l variants (60). These 5-HTTLPR s/s and l/s variants showed a significant epistatic
interaction with the Val/Val genotype of brain-derived neurotrophic factor (BDNF) and response to lithium prophylaxis in a
sample of 107 BD patients (61). In the study by Michelon et al., the 5-HTTLPR gene and BDNF gene variants were not
predictive factors for the response to lithium prophylaxis (40). Manchia et al. investigated several polymorphisms of genes of the
neurotransmitter system, including the DRD1, DRD2, DRD3, DAT1, 5-HTTLPR and HTR2A genes, for association with response
to lithium prophylaxis in a sample of 155 Sardinian BD probands (62). No association was found between the polymorphisms of
these genes and the response to lithium treatment (62). A recent association study involving DRD1 showed an association
between allele G at −48 A/G and a worse response to lithium (63). An additive association analysis of 5-HT2A and 5-HT2C
serotonin receptor gene polymorphisms and the response of BD patients to lithium prophylaxis found no association (64). To
summarize, four studies have reported associations between genotypes carrying the 5-HTTLPR s allele and a worse response to
lithium (60,61,65,66). An association and linkage study confirmed the absence of association between the response to lithium and
GABRA3, GABRA5 and GABRB3 subunits of the GABAA receptor (67).
5
Enzymes involved in the synthesis/catabolism of amines, including neurotransmitters, may be of relevance. Serretti et
al. did not find any association between the prophylactic efficacy of lithium in mood disorders and the following variants of
enzymes in the corresponding pathways: catechol-O-methyltransferase (COMT) G158A, monoamine oxidase A (MAO-A) 30-bp
repeat, and G-protein beta 3-subunit (Gβ3) C825T (68). A further association and linkage study found no association between
MAO-A and the response to lithium (69). The prophylactic efficacy of lithium may depend in part on variants of the tryptophan
hydroxylase (TPH) gene, which is a serotonin-related gene. Subjects with the TPH A/A variant showed a trend toward a worse
response to lithium than subjects with either TPH A/C or TPH C/C variants (70). An association study focused on the gene
encoding tyrosine hydroxylase (TH), the rate-limiting enzyme in catecholamine synthesis: it revealed no association in 54
patients with the long-term response to lithium monotherapy (71).
To conclude, the serotonin-related genes of the neurotransmitter system, and in particular the serotonin transporter
gene, show the strongest evidence of interactions with the response to lithium prophylaxis.
5.1.2.4. The BDNF/TrkB signaling pathway
BDNF-related genes have been implicated in the pathogenesis of BD and in the mechanism of action of lithium.
Rybakowski et al. showed extreme differences in response to lithium prophylaxis between subjects according to their BDNF
polymorphisms (61). Subsequent studies tended to validate this result and the Val/Met BDNF genotype at the Val66Met
functional polymorphism showed a positive association with better response to lithium in a sample of 88 BD patients (72). The
same authors provided a supplementary study investigating the association in the BDNF gene and polymorphisms in the gene
encoding the neurotrophic tyrosine kinase receptor type 2 (NTRK2) (73). Among the four BDNF polymorphisms tested, two
(C/G (rs988748) and G/A (rs6265)) showed an association with the response to lithium prophylaxis (73). No association was
found between the response to lithium and either the interaction of BDNF and NTRK2 genes or polymorphism of the NTRK2
gene alone (73). The Michelon et al and Masui et al studies did not find such results for BNDF (40,74).
Lithium inhibits glutamatergic transmission via NMDA receptors, and the src-family tyrosine kinases (FYN) belong to
the protein kinase family that phosphorylates NMDA receptor subunits, participating in the BDNF/TrkB signal transduction
pathway. A marginal association between FYN polymorphisms and a worse response to lithium in 101 BD patients has been
reported (75). The same authors investigated the association between three polymorphisms in the NMDA receptor 2B subunit
(GRIN2B) gene and the response to lithium but did not find a significant association (76).
These various findings suggest that the BDNF/TrkB signal transduction pathway may play a key role in the response to
lithium prophylaxis.
5.1.2.5. Other signaling pathways
Lithium may affect the cyclic adenosine monophosphate (cAMP) pathway of signal transduction. The first relevant
genetic study of BD found significant associations with the CREB1, CREB2 and CREB3 genes of this pathway (77). In a BD
sample of 180 lithium responders and 69 non-responders, and 127 controls, the same authors found that two CREB1
polymorphisms may be associated with BD and/or the response to lithium (77). In the same sample, there was no association
between the propyl endopeptidase (PREP) gene l and the response to lithium (78).
The endoplasmic reticulum (ER)-stress response, a potential pathophysiological mechanism of BD, involves various
molecules including the X-box-binding protein 1 (XBP1). An association between the response to lithium and -116C/G
polymorphism of XBP1 has been reported in Japanese BD patients (79). In the same BD Japanese population, this association
was further confirmed, with -116C allele carriers showing a better response than -116G homozygotes to lithium (80). The same
authors found a significant association between the breakpoint cluster region (BCR) gene and the response to lithium, observing
that the allele frequency of the Asn796Ser single-nucleotide polymorphism was significantly higher in non-responders than in
responders (81).
The protein kinase C (PKC) pathway is an important mediator of several intracellular responses to neurotransmitter
signaling. It has therefore been the subject of investigation, but a recent study failed to show any positive association between the
response to lithium and PDLIM5 (PDZ and LIM domain 5), an adaptor protein that selectively binds the isozyme PKC (epsilon)
to N-type Ca (2+) channels in neurons (82). Silberberg et al. investigated the calcium channel gamma-2 subunit (CACNG2,
Stargazin) gene on 22q13.1 and found that three single nucleotide polymorphisms (rs2284017, rs2284018, rs5750285) were
significantly associated with the response to lithium (83).
These preliminary results need to be replicated before any conclusions can be drawn. Polymorphisms of the genes for
activating enhancer-binding protein 2 beta 3 (AP2-B), the myristoylated alanine-rich C-kinase substrate (MARKS) and the betaadrenergic receptor kinase 2 (GRK3, BARK2) have been found not be to associated with the response to lithium (40,84).
Rybakowski et al., who had previously reported an association between BD and a functional polymorphism of matrix
metalloproteinase-9 (MMP-9) gene, tested for its involvement in the response to lithium and were unable to find any such
association (85).
6
Recently, Rybakowski et al. aimed to replicate some of these earlier findings and tested the association of 14 gene
polymorphisms with the quality of the response to lithium prophylaxis (86). The authors confirmed an association between the
response to lithium and the polymorphisms of 5HTTLPR, DRD1, COMT, BDNF and FYN genes, but not those of 5HT2A,
5HT2C, DRD2, DRD3, DRD4, GSK-3, NTRK2, GRIN2B and MMP-9. A list of these pharmacogenetic studies is provided in
Table 1.
5.1.3. Genome Wide Association Studies (GWAS) on the response to lithium
An international consortium on lithium genetics (ConLiGen, www.conligen.org) is currently driving an international
effort to elucidate the genetic underpinnings of the response of BD patient to lithium. The consortium aims to establish the largest
ever sample of cases of BD characterized for their response to lithium treatment suitable for genome-wide studies (87). In
particular, there is a particular effort to develop stringent definitions for the response phenotypes. This consortium has not yet
published or made available any results, but the scientific community is awaiting the findings with high hopes.
An early report described a sample of 359 BD patients characterized for the response to lithium and who were
participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) cohort (88). The associations
identified did not reach genome-wide significance, but the findings for two regions, on chromosome 10p15 (rs10795189) and
chromosome 4q32 including a gene coding for the glutamate/alpha-amino-3-hydroxy-5-methyl-4-isoxazolpropionate (AMPA)
receptor GRIA2, indicate that they deserve further examination (88). Squassina et al. performed a GWAS in a sample of 204
Sardinian patients with BD characterized for response to lithium and found an association, supported by quantitative trait
analysis, for a single nucleotide polymorphism (SNP) in intron 1 of the amiloride-sensitive cation channel 1 neuronal (ACCN1)
gene (89). This cation channel has high affinity for sodium and is permeable to lithium and consequently is a putative genetic
marker of lithium efficacy for patients with BD (89). However, this possibility needs to be confirmed. McCarthy et al. used a
multi-level approach focusing on associations between circadian clock genes and BD compared to controls, and also considered
the response to lithium (90). They reconciled discordant results from earlier GWAS and candidate gene studies by identifying
recognized and previously unrecognized associations between clock genes and BD-spectrum illnesses (90).
The results of these various approaches and the findings generated argue for continued GWAS of the response to
lithium in BD patients.
5.2. Pharmacogenomics of other mood stabilizers
Almost all pharmacogenetic studies of MS have focused on the response to lithium but informative results are sparse.
The situation for other MS is similarly, in addition to fewer reported studies. Thus, there is little evidence available for valproate
and even less for lamotrigine. Lastly, we will review current evidence about atypical antipsychotics’ pharmacogenetics.
5.2.1.Valproate (VPA)
The mechanism of action of valproate (VPA) is poorly understood and several hypotheses exist. The X-box-binding
protein 1 (XBP1) is involved in the endoplasmic reticulum (ER)-stress response, and the 116C/G polymorphism in the promoter
region of the corresponding gene is known to be associated with BD. An association between this polymorphism and the
response to VPA has been reported (91): in a sample of 51 BD patients the G allele was associated with a better response to VPA
than the C allele (91). The transcription activity of XBP1 was lower for the G allele than for the C allele. Thus VPA increases the
endoplasmic reticulum (ER)-stress response, which is compromised by the G allele. Similarly, association between the -116C/G
polymorphism and the clinical efficacy of lithium has been observed consistent with the notion that the XBP1 gene product is
involved in the response to MS (91).
The Val158Met polymorphism in the COMT gene is another candidate gene in the response to VPA and to lithium; its
role was examined in a sample of 144 BDI patients and 157 controls (92). The study found that the Met/Met genotype was more
frequent in non-responders than in responders to MS (either lithium, VPA or carbamazepine), whereas no differences were
detected between BD patients and controls. Unfortunately, the sample was pooled for types of MS and therefore the study is
uninformative about the role of COMT Val66Met in the response to individual mood stabilizers (92). Further studies with a larger
numbers of subjects are required to elucidate the role of COMT gene polymorphism in the therapeutic response of BD patients to
mood stabilizer.
5.2.2. Lamotrigine (LTG)
A pharmacogenetic study based on the response to LTG has been performed in 85 LTG-treated BD I depression
patients. Polymorphisms in the dopamine D2 receptor (DRD2), dopamine β-hydroxylase (DBH), glucocorticoid receptor
(NR3C1), histamine H1 receptor (HRH1) and melanocortin 2 receptor (MCR2) genes were associated with the response to
treatment (93). As far as we are aware, this is the only pharmacogenetic study addressing LTG to be reported, no other results of
studies of this type, relevant to conventional MS, have been published. Several pathways seem to be involved in the response to
LTG, and might be, at least in part, shared by lithium and other conventional MS.
5.2.3. Atypical antipsychotics (AAP)
7
Antipsychotic medication is widely used, being prescribed to between 72% and 92% of patients with mania (94).
Despite this extensive use of AAP in the treatment of BD, pharmacogenetic studies are again lacking and very few studies have
investigated the genetic underpinnings of the therapeutic response. Furthermore, these few studies only included patients during
acute phases of BD.
Perlis et al. investigated common genetic variations for association with clinical improvement in a cohort of 88 BD I
depression patients following treatment with an olanzapine/fluoxetine combination (OFC) (93). They found significant
associations between polymorphisms in the dopamine D (3) receptor (DRD3) and HRH1 genes, and response to OFC (93).
Subsequently, in the same population, they found an association between the response to OFC and polymorphisms in the
norepinephrine transporter (SLC6A2) gene, the melanocortin 3 receptor (MC3R) gene and the tryptophan hydroxylase 2 (TPH2)
gene (95).
Furthermore, Dávila et al. investigated the role of the COMT Val158Met polymorphism in the plasma concentration
of catecholamine metabolites and clinical features in 42 BD I patients (96). Authors found no significant association with the
response to olanzapine treatment or with any of the markers tested, including the plasma concentrations of metabolites of
dopamine (homovanillic acid; HVA) and of noradrenaline (3-methoxy-4-hydroxyphenylglycol; MHPG). Nevertheless, in the
homozygous Val-Val group, a non-significant aggregation of BD patients presenting with psychosis was found; and clinical
improvement significantly correlated with the plasma concentration of MHPG prior to treatment. The preliminary findings of
these two studies are of interest and further work on these issues would be fruitful.
Table 2 presents published pharmacogenetic studies of the response to various mood-stabilizing medications. In view
of the widespread and increasing prescription of antipsychotics to patients with BD further research efforts in pharmacogenetics
to identify possible genetic predictors of response would be extremely valuable.
6. SUMMARY AND PERSPECTIVES
To prescribe MS appropriately to patients, predictors of the response are required. Various genetic markers are
considered to be promising candidates. In this review, we present diverse findings that are promising, and further investigation is
warranted for confirmation. It seems very likely that the response to MS has a complex genetic heritability. Candidate genes
associated with BD display relatively low odds ratios (OR) and minor allele frequencies (MAF), and therefore it is unlikely that
the response to MS is determined by common variants with large effect-sizes.
Furthermore, specific clinical features, family history, comorbidities and clinical course are factors that may be closely
linked to the MS response phenotype and thus may help to understand its complex genetic heritability. For example, A. Bremer
et al observed that polymorphisms in NTRK2 and INPP1 genes were associated with the response to lithium, and also with both
suicidal ideation and post-traumatic stress disorder; this indicates that the response to lithium in BD and clinical co-morbidities
share, at least partly, genetic determinants (84).
This review leads us to suggest several putative goals for pharmacogenomics research in BD: genetic research in mood
disorders can be reasonably expected to contribute in the following areas associated with treatment effects: 1) prediction of
treatment response in individual patients; 2) prediction of side effects; 3) development of personalized therapies; 4) identification
of homogeneous clinical subgroups of BD for genetic studies; 5) identification of causative determinants of BD; 6) identification
of new treatment pathways; 7) development of gene therapy for BD; and 8) findings that are relevant to other psychiatric
diseases. Some of the goals that we believe are important for pharmacogenomics research in BD are summarized in Figure 1.
These approaches are however subject to several limitations, and as a consequence of some of them, the interpretation
of pharmacogenetic results can be difficult (summarized in Table 1 as relevant to the efficacy of lithium prophylaxis). First,
diagnostic heterogeneity in patient groups prevents rigorous comparison between studies. The definitions of the response to MS
(see table 1 and 2) are not consensual and differ between studies. Clearly, valid and consensual definitions of probands and clear
criteria for the definition of the response to MS are needed for results to be reliable and comparable.
Also, most of the candidate genes studied were chosen for their possible association with mood disorders, rather than
for their putative role in the mechanism of action of lithium or other MS. Future studies on biological and genetic factors
associated with lithium response will have to consider potential confounders such as compliance and co-administration of
circadian rhythm therapy, other psychotropic drugs or psychotherapy. Finally, sample sizes in these studies are often small;
prospective studies with larger samples are required to study the response to MS.
7. CONCLUSION
To date, the results from pharmacogenomics studies are not sufficiently abundant, informative or conclusive to have
significantly changed daily practice in the management of BD. The clinical assessment of a subject with the identification of
specific individual phenotypic and pharmacogenetics data may nevertheless become a powerful approach for the development of
8
personalized therapies. Further pharmacogenomics studies are needed to validate reliable and reproducible predictors of
individual responses to MS and MS safety. Advances made in pharmacogenomics may help the clinician select appropriate
effective treatment and monitoring, leading to more personalized treatment algorithms that are currently lacking for BD.
8. ACKNOWLEDGEMENTS
P.A. Geoffroy has received a prize from Bayer for being Laureate of the medical university of Lille. F. Bellivier has
received honoraria and financial support as an independent symposium speaker from Sanofi-Aventis, Lundbeck, AstraZeneca, Eli
Lilly, Bristol-Myers Squibb and Servier. M. Leboyer has received honoraria and financial support as an independent symposium
speaker from AstraZeneca and Servier. B. Etain has received honoraria and financial support as an independent symposium
speaker from Sanofi-Aventis, Lundbeck, AstraZeneca, Eli Lilly, Bristol-Myers Squibb and Servier.
9. REFERENCES
1. M Leboyer, DJ Kupfer: Bipolar disorder: new perspectives in health care and prevention. J Clin Psychiatry. 71 (12), 1689–
1695 (2010)
2. PA Geoffroy, B Etain, C Henry, F Bellivier: Combination Therapy for Manic Phases: A Critical Review of a Common
Practice. CNS Neurosci Ther. 18 (12), 957-964 (2012)
3. J Angst: The emerging epidemiology of hypomania and bipolar II disorder. J Affect Disord. 50 (2-3), 143–151 (1998)
4. KR Merikangas, HS Akiskal, J Angst, PE Greenberg, RMA Hirschfeld, M Petukhova, RC Kessler: Lifetime and 12-month
prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch. Gen. Psychiatry. 64 (5), 543–552
(2007)
5. Murray C, Lopez A: The Global Burden of Disease. A Comprehensive Assessment of Morbidity and Disability From Diseases,
Injuries and Risk Factors in 1990 and Projected to 2020. Cambridge, Massachusetts: Harvard University Press (1996)
6. J de Leon, MT Susce, E Murray-Carmichael: The AmpliChip CYP450 genotyping test: Integrating a new clinical tool. Mol
Diagn Ther. 10 (3), 135–151 (2006)
7. MJ Gitlin, J Swendsen, TL Heller, C Hammen: Relapse and impairment in bipolar disorder. Am J Psychiatry. 152 (11), 1635–
1640 (1995)
8. JM Haro, C Reed, A Gonzalez-Pinto, D Novick, J Bertsch, E Vieta: 2-Year course of bipolar disorder type I patients in
outpatient care: factors associated with remission and functional recovery. Eur Neuropsychopharmacol. 21 (4), 287–293 (2011)
9. J Garnham, A Munro, C Slaney, M Macdougall, M Passmore, A Duffy, C O’Donovan, A Teehan, M Alda: Prophylactic
treatment response in bipolar disorder: results of a naturalistic observation study. J Affect Disord. 104 (1-3), 185–190 (2007)
10. P Grof, A Duffy, P Cavazzoni, E Grof, J Garnham, M MacDougall, C O’Donovan, M Alda: Is response to prophylactic
lithium a familial trait? J Clin Psychiatry. 63 (10), 942–947 (2002)
11. M Alda, E Grof, P Cavazzoni, A Duffy, R Martin, L Ravindran, P Grof: Autosomal recessive inheritance of affective
disorders in families of responders to lithium prophylaxis? Journal of Affective Disorders. 44 (2–3), 153–157 (1997)
12. M Alda: Genetic factors and treatment of mood disorders. Bipolar Disord. 3 (6), 318–324 (2001)
13. HA Mansour, M Alda, VL Nimgaonkar: Pharmacogenetics of bipolar disorder. Curr Psychiatry Rep. 4 (2), 117–123 (2002)
14. A Squassina, M Manchia, M Del Zompo: Pharmacogenomics of mood stabilizers in the treatment of bipolar disorder. Hum
Genomics Proteomics. 2010, 159761 (2010)
15. GM MacQueen, T Hajek, M Alda: The phenotypes of bipolar disorder: relevance for genetic investigations. Mol. Psychiatry.
10 (9), 811–826 (2005)
16. DJ Smith, R Evans, N Craddock: Predicting response to lithium in bipolar disorder: a critical review of pharmacogenetic
studies. J Ment Health. 19 (2), 142–156 (2010)
17. MJ McCarthy, SG Leckband, JR Kelsoe: Pharmacogenetics of lithium response in bipolar disorder. Pharmacogenomics. 11
(10), 1439–1465 (2010)
9
18. A Serretti, A Drago: Pharmacogenetics of lithium long-term treatment: focus on initiation and adaptation mechanisms.
Neuropsychobiology. 62 (1), 61–71 (2010)
19. M Leboyer, F Bellivier, M Nosten-Bertrand, R Jouvent, D Pauls, J Mallet: Psychiatric genetics: search for phenotypes.
Trends Neurosci. 21 (3), 102–105 (1998)
20. M Alda, P Grof, GA Rouleau, G Turecki, LT Young: Investigating responders to lithium prophylaxis as a strategy for
mapping susceptibility genes for bipolar disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry. 29 (6), 1038–1045 (2005)
21. MJ Passmore, J Garnham, A Duffy, M MacDougall, A Munro, C Slaney, A Teehan, M Alda: Phenotypic spectra of bipolar
disorder in responders to lithium versus lamotrigine. Bipolar Disord. 5 (2), 110–114 (2003)
22. PA Geoffroy, B Etain, J Scott, C Henry, S Jamain, M Leboyer, F Bellivier: Reconsideration of bipolar disorder as a
developmental disorder: Importance of the time of onset. J. Physiol. Paris. (2013)
23. M Alda: The phenotypic spectra of bipolar disorder. Eur Neuropsychopharmacol. 14 Suppl 2, S94–99 (2004)
24. MK Spearing, RM Post, GS Leverich, D Brandt, W Nolen: Modification of the Clinical Global Impressions (CGI) Scale for
use in bipolar illness (BP): the CGI-BP. Psychiatry Res. 73 (3), 159–171 (1997)
25. DW Nebert: Extreme discordant phenotype methodology: an intuitive approach to clinical pharmacogenetics. European
Journal of Pharmacology. 410 (2–3), 107–120 (2000)
26. G Zhang, DW Nebert, R Chakraborty, L Jin: Statistical power of association using the extreme discordant phenotype design.
Pharmacogenetics and Genomics. 16 (6), 401–413 (2006)
27. A Coppen, SA Montgomery, RK Gupta, JE Bailey: A double-blind comparison of lithium carbonate and maprotiline in the
prophylaxis of the affective disorders. Br J Psychiatry. 128, 479–485 (1976)
28. M Maj, M Del Vecchio, F Starace, R Pirozzi, D Kemali: Prediction of affective psychoses response to lithium prophylaxis.
The role of socio-demographic, clinical, psychological and biological variables. Acta Psychiatr Scand. 69 (1), 37–44 (1984)
29. P Gajwani: Treatment-refractory bipolar disorder: classification to aid in clinical management. Expert Opin Pharmacother.
10 (12), 1907–1915 (2009)
30. H Ewald, AG Wang, M Vang, O Mors, M Nyegaard, TA Kruse: A haplotype-based study of lithium responding patients with
bipolar affective disorder on the Faroe Islands. Psychiatr. Genet. 9 (1), 23–34 (1999)
31. G Turecki, P Grof, P Cavazzoni, A Duffy, E Grof, R Martin, R Joober, GA Rouleau, M Alda: Lithium responsive bipolar
disorder, unilineality, and chromosome 18: A linkage study. Am. J. Med. Genet. 88 (4), 411–415 (1999)
32. LM Evans, HS Akiskal, TA Greenwood, CM Nievergelt, PE Keck Jr, SL McElroy, AD Sadovnick, RA Remick, NJ Schork,
JR Kelsoe: Suggestive linkage of a chromosomal locus on 18p11 to cyclothymic temperament in bipolar disorder families. Am. J.
Med. Genet. B Neuropsychiatr. Genet. 147 (3), 326–332 (2008)
33. J Morissette, A Villeneuve, L Bordeleau, D Rochette, C Laberge, B Gagné, C Laprise, G Bouchard, M Plante, L Gobeil, E
Shink, J Weissenbach, N Barden: Genome-wide search for linkage of bipolar affective disorders in a very large pedigree derived
from a homogeneous population in quebec points to a locus of major effect on chromosome 12q23-q24. Am. J. Med. Genet. 88
(5), 567–587 (1999)
34. E Shink, J Morissette, R Sherrington, N Barden: A genome-wide scan points to a susceptibility locus for bipolar disorder on
chromosome 12. Mol. Psychiatry. 10 (6), 545–552 (2005)
35. G Turecki, P Grof, E Grof, V D’Souza, L Lebuis, C Marineau, P Cavazzoni, A Duffy, C Bétard, P Zvolský, C Robertson, C
Brewer, TJ Hudson, GA Rouleau, M Alda: Mapping susceptibility genes for bipolar disorder: a pharmacogenetic approach based
on excellent response to lithium. Mol. Psychiatry. 6 (5), 570–578 (2001)
36. C Lopez de Lara, I Jaitovich-Groisman, C Cruceanu, F Mamdani, V Lebel, V Yerko, A Beck, LT Young, G Rouleau, P Grof,
M Alda, G Turecki: Implication of synapse-related genes in bipolar disorder by linkage and gene expression analyses. Int. J.
Neuropsychopharmacol. 13 (10), 1397–1410 (2010)
10
37. L Toker, RH Belmaker, G Agam: Gene-expression studies in understanding the mechanism of action of lithium. Expert Rev
Neurother. 12 (1), 93–97 (2012)
38. RSB Williams, L Cheng, AW Mudge, AJ Harwood: A common mechanism of action for three mood-stabilizing drugs.
Nature. 417 (6886), 292–295 (2002)
39. VM Steen, R Løvlie, Y Osher, RH Belmaker, JO Berle, AK Gulbrandsen: The polymorphic inositol polyphosphate 1phosphatase gene as a candidate for pharmacogenetic prediction of lithium-responsive manic-depressive illness.
Pharmacogenetics. 8 (3), 259–268 (1998)
40. L Michelon, I Meira-Lima, Q Cordeiro, K Miguita, G Breen, D Collier, H Vallada: Association study of the INPP1, 5HTT,
BDNF, AP-2beta and GSK-3beta GENE variants and restrospectively scored response to lithium prophylaxis in bipolar disorder.
Neurosci. Lett. 403 (3), 288–293 (2006)
41. A Dimitrova, V Milanova, S Krastev, I Nikolov, D Toncheva, MJ Owen, G Kirov: Association study of myo-inositol
monophosphatase 2 (IMPA2) polymorphisms with bipolar affective disorder and response to lithium treatment.
Pharmacogenomics J. 5 (1), 35–41 (2005)
42. G Sjøholt, RP Ebstein, RT Lie, JØ Berle, J Mallet, JF Deleuze, DF Levinson, C Laurent, M Mujahed, I Bannoura, I Murad, A
Molven, VM Steen: Examination of IMPA1 and IMPA2 genes in manic-depressive patients: association between IMPA2
promoter polymorphisms and bipolar disorder. Mol. Psychiatry. 9 (6), 621–629 (2004)
43. VM Steen, AK Gulbrandsen, HG Eiken, JO Berle: Lack of genetic variation in the coding region of the myo-inositol
monophosphatase gene in lithium-treated patients with manic depressive illness. Pharmacogenetics. 6 (1), 113–116 (1996)
44. AE Baum, N Akula, M Cabanero, I Cardona, W Corona, B Klemens, TG Schulze, S Cichon, M Rietschel, MM Nöthen, A
Georgi, J Schumacher, M Schwarz, R Abou Jamra, S Höfels, P Propping, J Satagopan, SD Detera-Wadleigh, J Hardy, FJ
McMahon: A genome-wide association study implicates diacylglycerol kinase eta (DGKH) and several other genes in the
etiology of bipolar disorder. Mol. Psychiatry. 13 (2), 197–207 (2008)
45. M Manchia, A Squassina, D Congiu, C Chillotti, R Ardau, G Severino, M Del Zompo: Interacting genes in lithium
prophylaxis: preliminary results of an exploratory analysis on the role of DGKH and NR1D1 gene polymorphisms in 199
Sardinian bipolar patients. Neurosci. Lett. 467 (2), 67–71 (2009)
46. A Squassina, M Manchia, D Congiu, G Severino, C Chillotti, R Ardau, M Piccardi, MD Zompo: The diacylglycerol kinase
eta gene and bipolar disorder: a replication study in a Sardinian sample. Mol. Psychiatry. 14 (4), 350–351 (2009)
47. G Turecki, P Grof, P Cavazzoni, A Duffy, E Grof, B Ahrens, A Berghöfer, B Müller-Oerlinghausen, M Dvoráková, E
Libigerová, M Vojtechovský, P Zvolský, R Joober, A Nilsson, H Prochazka, RW Licht, NA Rasmussen, M Schou, P
Vestergaard, A Holzinger, C Schumann, K Thau, GA Rouleau, M Alda: Evidence for a role of phospholipase C-gamma1 in the
pathogenesis of bipolar disorder. Mol. Psychiatry. 3 (6), 534–538 (1998)
48. N Ftouhi-Paquin, M Alda, P Grof, N Chretien, G Rouleau, G Turecki: Identification of three polymorphisms in the translated
region of PLC-gamma1 and their investigation in lithium responsive bipolar disorder. Am. J. Med. Genet. 105 (3), 301–305
(2001)
49. R Løvlie, JO Berle, E Stordal, VM Steen: The phospholipase C-gamma1 gene (PLCG1) and lithium-responsive bipolar
disorder: re-examination of an intronic dinucleotide repeat polymorphism. Psychiatr. Genet. 11 (1), 41–43 (2001)
50. L Freland, J-M Beaulieu: Inhibition of GSK3 by lithium, from single molecules to signaling networks. Front Mol Neurosci.
5, 14 (2012)
51. F Benedetti, A Serretti, C Colombo, C Lorenzi, V Tubazio, E Smeraldi: A glycogen synthase kinase 3-beta promoter gene
single nucleotide polymorphism is associated with age at onset and response to total sleep deprivation in bipolar depression.
Neurosci. Lett. 368 (2), 123–126 (2004)
52. A Szczepankiewicz, JK Rybakowski, A Suwalska, M Skibinska, A Leszczynska-Rodziewicz, M Dmitrzak-Weglarz, PM
Czerski, J Hauser: Association study of the glycogen synthase kinase-3beta gene polymorphism with prophylactic lithium
response in bipolar patients. World J. Biol. Psychiatry. 7 (3), 158–161 (2006)
53. L Yin, J Wang, PS Klein, MA Lazar: Nuclear receptor Rev-erbalpha is a critical lithium-sensitive component of the circadian
clock. Science. 311 (5763), 1002–1005 (2006)
11
54. S Campos-de-Sousa, C Guindalini, L Tondo, J Munro, S Osborne, G Floris, M Pedrazzoli, S Tufik, G Breen, D Collier:
Nuclear receptor rev-erb-{alpha} circadian gene variants and lithium carbonate prophylaxis in bipolar affective disorder. J. Biol.
Rhythms. 25 (2), 132–137 (2010)
55. MJ McCarthy, CM Nievergelt, T Shekhtman, DF Kripke, DK Welsh, JR Kelsoe: Functional genetic variation in the RevErbα pathway and lithium response in the treatment of bipolar disorder. Genes Brain Behav. 10 (8), 852–861 (2011)
56. A Szczepankiewicz, JK Rybakowski, A Suwalska, J Hauser: Glucocorticoid receptor polymorphism is associated with
lithium response in bipolar patients. Neuro Endocrinol. Lett. 32 (4), 545–551 (2011)
57. A Serretti, R Lilli, C Lorenzi, L Franchini, D Di Bella, M Catalano, E Smeraldi: Dopamine receptor D2 and D4 genes, GABA
(A) alpha-1 subunit genes and response to lithium prophylaxis in mood disorders. Psychiatry Res. 87 (1), 7–19 (1999)
58. A Serretti, R Lilli, C Lorenzi, L Franchini, E Smeraldi: Dopamine receptor D3 gene and response to lithium prophylaxis in
mood disorders. Int. J. Neuropsychopharmacol. 1 (2), 125–129 (1998)
59. A Serretti, C Lorenzi, R Lilli, E Smeraldi: Serotonin receptor 2A, 2C, 1A genes and response to lithium prophylaxis in mood
disorders. J Psychiatr Res. 34 (2), 89–98 (2000)
60. A Serretti, R Lilli, L Mandelli, C Lorenzi, E Smeraldi: Serotonin transporter gene associated with lithium prophylaxis in
mood disorders. Pharmacogenomics J. 1 (1), 71–77 (2001)
61. JK Rybakowski, A Suwalska, M Skibinska, M Dmitrzak-Weglarz, A Leszczynska-Rodziewicz, J Hauser: Response to
lithium prophylaxis: interaction between serotonin transporter and BDNF genes. Am. J. Med. Genet. B Neuropsychiatr. Genet.
144B (6), 820–823 (2007)
62. M Manchia, D Congiu, A Squassina, S Lampus, R Ardau, C Chillotti, G Severino, M Del Zompo: No association between
lithium full responders and the DRD1, DRD2, DRD3, DAT1, 5-HTTLPR and HTR2A genes in a Sardinian sample. Psychiatry
Res. 169 (2), 164–166 (2009)
63. JK Rybakowski, M Dmitrzak-Weglarz, A Suwalska, A Leszczynska-Rodziewicz, J Hauser: Dopamine D1 receptor gene
polymorphism is associated with prophylactic lithium response in bipolar disorder. Pharmacopsychiatry. 42 (1), 20–22 (2009)
64. M Dmitrzak-Weglarz, JK Rybakowski, A Suwalska, A Słopień, PM Czerski, A Leszczyńska-Rodziewicz, J Hauser:
Association studies of 5-HT2A and 5-HT2C serotonin receptor gene polymorphisms with prophylactic lithium response in
bipolar patients. Pharmacol Rep. 57 (6), 761–765 (2005)
65. A Serretti, PN Malitas, L Mandelli, C Lorenzi, C Ploia, B Alevizos, C Nikolaou, F Boufidou, GN Christodoulou, E Smeraldi:
Further evidence for a possible association between serotonin transporter gene and lithium prophylaxis in mood disorders.
Pharmacogenomics J. 4 (4), 267–273 (2004)
66. JK Rybakowski, A Suwalska, PM Czerski, M Dmitrzak-Weglarz, A Leszczynska-Rodziewicz, J Hauser: Prophylactic effect
of lithium in bipolar affective illness may be related to serotonin transporter genotype. Pharmacol Rep. 57 (1), 124–127 (2005)
67. A Duffy, G Turecki, P Grof, P Cavazzoni, E Grof, R Joober, B Ahrens, A Berghöfer, B Müller-Oerlinghausen, M Dvoráková,
E Libigerová, M Vojtĕchovský, P Zvolský, A Nilsson, RW Licht, NA Rasmussen, M Schou, P Vestergaard, A Holzinger, C
Schumann, K Thau, C Robertson, GA Rouleau, M Alda: Association and linkage studies of candidate genes involved in
GABAergic neurotransmission in lithium-responsive bipolar disorder. J Psychiatry Neurosci. 25 (4), 353–358 (2000)
68. A Serretti, C Lorenzi, R Lilli, L Mandelli, A Pirovano, E Smeraldi: Pharmacogenetics of lithium prophylaxis in mood
disorders: analysis of COMT, MAO-A, and Gbeta3 variants. Am. J. Med. Genet. 114 (4), 370–379 (2002)
69. G Turecki, P Grof, P Cavazzoni, A Duffy, E Grof, B Ahrens, A Berghöfer, B Müller-Oerlinghausen, M Dvoráková, E
Libigerová, M Vojtechovsky, P Zvolsky, R Joober, A Nilsson, H Prochazka, RW Licht, NA Rasmussen, M Schou, P
Vestergaard, A Holzinger, C Schumann, K Thau, GA Rouleau, M Alda: MAOA: association and linkage studies with lithium
responsive bipolar disorder. Psychiatr. Genet. 9 (1), 13–16 (1999)
70. A Serretti, R Lilli, C Lorenzi, M Gasperini, E Smeraldi: Tryptophan hydroxylase gene and response to lithium prophylaxis in
mood disorders. J Psychiatr Res. 33 (5), 371–377 (1999)
12
71. P Cavazzoni, M Alda, G Turecki, G Rouleau, E Grof, R Martin, A Duffy, P Grof: Lithium-responsive affective disorders: no
association with the tyrosine hydroxylase gene. Psychiatry Res. 64 (2), 91–96 (1996)
72. JK Rybakowski, A Suwalska, M Skibinska, A Szczepankiewicz, A Leszczynska-Rodziewicz, A Permoda, PM Czerski, J
Hauser: Prophylactic lithium response and polymorphism of the brain-derived neurotrophic factor gene. Pharmacopsychiatry. 38
(4), 166–170 (2005)
73. M Dmitrzak-Weglarz, JK Rybakowski, A Suwalska, M Skibinska, A Leszczynska-Rodziewicz, A Szczepankiewicz, J
Hauser: Association studies of the BDNF and the NTRK2 gene polymorphisms with prophylactic lithium response in bipolar
patients. Pharmacogenomics. 9 (11), 1595–1603 (2008)
74. T Masui, R Hashimoto, I Kusumi, K Suzuki, T Tanaka, S Nakagawa, T Suzuki, N Iwata, N Ozaki, T Kato, H Kunugi, T
Koyama: Lithium response and Val66Met polymorphism of the brain-derived neurotrophic factor gene in Japanese patients with
bipolar disorder. Psychiatr. Genet. 16 (2), 49–50 (2006)
75. A Szczepankiewicz, M Skibinska, A Suwalska, J Hauser, JK Rybakowski: The association study of three FYN
polymorphisms with prophylactic lithium response in bipolar patients. Hum Psychopharmacol. 24 (4), 287–291 (2009)
76. A Szczepankiewicz, M Skibińska, A Suwalska, J Hauser, JK Rybakowski: No association of three GRIN2B polymorphisms
with lithium response in bipolar patients. Pharmacol Rep. 61 (3), 448–452 (2009)
77. F Mamdani, M Alda, P Grof, LT Young, G Rouleau, G Turecki: Lithium response and genetic variation in the CREB family
of genes. Am. J. Med. Genet. B Neuropsychiatr. Genet. 147B (4), 500–504 (2008)
78. F Mamdani, A Sequeira, M Alda, P Grof, G Rouleau, G Turecki: No association between the PREP gene and lithium
responsive bipolar disorder. BMC Psychiatry. 7, 9 (2007)
79. C Kakiuchi, T Kato: Lithium response and -116C/G polymorphism of XBP1 in Japanese patients with bipolar disorder. Int. J.
Neuropsychopharmacol. 8 (4), 631–632 (2005)
80. T Masui, R Hashimoto, I Kusumi, K Suzuki, T Tanaka, S Nakagawa, H Kunugi, T Koyama: A possible association between
the -116C/G single nucleotide polymorphism of the XBP1 gene and lithium prophylaxis in bipolar disorder. Int. J.
Neuropsychopharmacol. 9 (1), 83–88 (2006)
81. T Masui, R Hashimoto, I Kusumi, K Suzuki, T Tanaka, S Nakagawa, T Suzuki, N Iwata, N Ozaki, T Kato, M Takeda, H
Kunugi, T Koyama: A possible association between missense polymorphism of the breakpoint cluster region gene and lithium
prophylaxis in bipolar disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry. 32 (1), 204–208 (2008)
82. A Squassina, D Congiu, F Manconi, M Manchia, C Chillotti, S Lampus, G Severino, MD Zompo: The PDLIM5 gene and
lithium prophylaxis: an association and gene expression analysis in Sardinian patients with bipolar disorder. Pharmacol. Res. 57
(5), 369–373 (2008)
83. G Silberberg, A Levit, D Collier, D St Clair, J Munro, RW Kerwin, L Tondo, G Floris, G Breen, R Navon: Stargazin
involvement with bipolar disorder and response to lithium treatment. Pharmacogenet. Genomics. 18 (5), 403–412 (2008)
84. T Bremer, C Diamond, R McKinney, T Shehktman, TB Barrett, C Herold, JR Kelsoe: The pharmacogenetics of lithium
response depends upon clinical co-morbidity. Mol Diagn Ther. 11 (3), 161–170 (2007)
85. JK Rybakowski, M Skibinska, A Suwalska, A Leszczynska-Rodziewicz, L Kaczmarek, J Hauser: Functional polymorphism
of matrix metalloproteinase-9 (MMP-9) gene and response to lithium prophylaxis in bipolar patients. Hum Psychopharmacol. 26
(2), 168–171 (2011)
86. JK Rybakowski, P Czerski, M Dmitrzak-Weglarz, S Kliwicki, A Leszczynska-Rodziewicz, A Permoda-Osip, M Skibinska, A
Suwalska, A Szczepankiewicz, J Hauser: Clinical and pathogenic aspects of candidate genes for lithium prophylactic efficacy. J.
Psychopharmacol. (Oxford) 26 (3), 368–373 (2012)
87. TG Schulze, M Alda, M Adli, N Akula, R Ardau, ET Bui, C Chillotti, S Cichon, P Czerski, M Del Zompo, SD DeteraWadleigh, P Grof, O Gruber, R Hashimoto, J Hauser, R Hoban, N Iwata, L Kassem, T Kato, S Kittel-Schneider, S Kliwicki, JR
Kelsoe, I Kusumi, G Laje, SG Leckband, M Manchia, G Macqueen, T Masui, N Ozaki, RH Perlis, A Pfennig, P Piccardi, S
Richardson, G Rouleau, A Reif, JK Rybakowski, J Sasse, J Schumacher, G Severino, JW Smoller, A Squassina, G Turecki, LT
Young, T Yoshikawa, M Bauer, FJ McMahon: The International Consortium on Lithium Genetics (ConLiGen): an initiative by
the NIMH and IGSLI to study the genetic basis of response to lithium treatment. Neuropsychobiology. 62 (1), 72–78 (2010)
13
88. RH Perlis, JW Smoller, MAR Ferreira, A McQuillin, N Bass, J Lawrence, GS Sachs, V Nimgaonkar, EM Scolnick, H
Gurling, P Sklar, S Purcell: A genomewide association study of response to lithium for prevention of recurrence in bipolar
disorder. Am J Psychiatry. 166 (6), 718–725 (2009)
89. A Squassina, M Manchia, J Borg, D Congiu, M Costa, M Georgitsi, C Chillotti, R Ardau, K Mitropoulos, G Severino, M Del
Zompo, GP Patrinos: Evidence for association of an ACCN1 gene variant with response to lithium treatment in Sardinian patients
with bipolar disorder. Pharmacogenomics. 12 (11), 1559–1569 (2011)
90. MJ McCarthy, CM Nievergelt, JR Kelsoe, DK Welsh: A survey of genomic studies supports association of circadian clock
genes with bipolar disorder spectrum illnesses and lithium response. PLoS ONE. 7 (2), e32091 (2012)
91. B Kim, CY Kim, MJ Lee, YH Joo: Preliminary evidence on the association between XBP1-116C/G polymorphism and
response to prophylactic treatment with valproate in bipolar disorders. Psychiatry Res. 168 (3), 209–212 (2009)
92. H-Y Lee, Y-K Kim: Catechol-O-methyltransferase Val158Met polymorphism affects therapeutic response to mood stabilizer
in symptomatic manic patients. Psychiatry Res. 175 (1-2), 63–66 (2010)
93. RH Perlis, DH Adams, B Fijal, VK Sutton, M Farmen, A Breier, JP Houston: Genetic association study of treatment response
with olanzapine/fluoxetine combination or lamotrigine in bipolar I depression. J Clin Psychiatry. 71 (5), 599–605 (2010)
94. J Cookson: Use of antipsychotic drugs and lithium in mania. Br J Psychiatry. 178 (Suppl 41), S148–156 (2001)
95. JP Houston, K Lau, V Aris, W Liu, BA Fijal, AN Heinloth, RH Perlis: Association of common variations in the
norepinephrine transporter gene with response to olanzapine-fluoxetine combination versus continued-fluoxetine treatment in
patients with treatment-resistant depression: a candidate gene analysis. J Clin Psychiatry. 73 (6), 878–885 (2012)
96. R Dávila, M Zumárraga, N Basterreche, A Arrúe, MI Zamalloa, JB Anguiano: Influence of the catechol-O-methyltransferase
Val108/158Met polymorphism on the plasma concentration of catecholamine metabolites and on clinical features in type I
bipolar disorder--a preliminary report. J Affect Disord. 92 (2-3), 277–281 (2006)
Key Words: Bipolar disorder, Pharmacogenomics, Pharmacogenetics, Mood Stabilizer, Lithium, Review
Send correspondence to: Pierre Alexis Geoffroy, Pole de Psychiatrie, Centre Expert Bipolaire, Hopital Albert Chenevier,
pavillon Hartman, 40, rue de Mesly,
94000 Creteil Cedex, France, Tel:33149813290, Fax:33149813099, E-mail:
pierre.a.geoffroy@gmail.com
14
Table 1. Pharmacogenetic studies on the response to lithium in bipolar disorder
Gene
Sample
The inositol pathway
INPP1
a) 23 BD + 20
controls
b) 54 BD I + 50
controls
134 BD I
184 BD
(92R, 92NR)
IMPA2
IMPA1
DGKH
PLCG1
237 parentsoffspring trios
and 174 cases
ascertained for
their response
to lithium and
170 controls
a)44
Norwegian
lithium-treated
patients with
BD
b) 75 nuclear
families from a
Palestinian
Arab trio
sample with
BD
184 BD
(92R, 92NR)
184 BD
(92R, 92NR)
a)44
Norwegian
lithium-treated
patients with
BD
b) 75 nuclear
families from a
Palestinian
Arab trio
sample with
BD
21 BD patients
(7R, 7NR,
7UN)
91 BD lithium
responders
(24FR,
67PR+NR)
199 BD lithium
responders
(57FR,
142PR+NR)
a) 136 BD
lithium
responders
163 controls
b) 32 families
ascertained
through
lithiumresponsive BD
probands
133 BD lithium
responders
Association
(Yes/No)
Study design
Definition of response
Reference
a) Yes
b) No
Retrospective
a) R: demonstrated “complete lithium response”
b) R: demonstrated “long and complete remission” on
lithium alone
(39)
No
Retrospective
(40)
Yes
(in BD with
posttraumatic
stress
disorder)
Yes
Retrospective
R ‘‘ Good responders’’: no recurrence of impairing
symptoms, or recurrence of mild symptoms, promptly
controlled by adjusting the lithium dose or with short
courses of benzodiazepines but no other medication.
PR : lithium level ≥0.6 mEq/l with improvement of the
recurrence pattern in spite of being mildly depressed or
hypomanic while on monotherapy.
R: rated retrospectively from standardized interviews and
medical records
‘‘ Good responders’’: patients recruited for genetic
association studies had clearly shown a good response to
lithium
(41)
Retrospective
(84)
‘‘Poor responders’’: some of these patients experienced no
benefit at all
a) No
b) Yes
Retrospective
a) classified retrospectively according to the clinical
history, with comparison of the frequency, duration and
severity of episodes before and after treatment
b) demonstrated “long and complete remission” on lithium
alone
(42)
No
Retrospective
(84)
No
Retrospective
a) No
b) No
Retrospective
R: rated retrospectively from standardized interviews and
medical records
R: rated retrospectively from standardized interviews and
medical records
a) classified retrospectively according to the clinical
history, with comparison of the frequency, duration and
severity of episodes before and after treatment
b) demonstrated “long and complete remission” on lithium
alone
No
Retrospective
classified retrospectively according to the clinical history
(43)
No
Retrospective
Response to lithium: assessed using the scale of Grof et al.
(24).
(46)
No
Retrospective
Response to lithium: assessed using the scale of Grof et al.
(24).
(45)
a) Yes
b) Yes
(when
unilineal
families
were
considered)
Prospective
Response to lithium was evaluated prospectively with an
average follow-up of 14.4 ± 6.8 years.
(47)
No
Prospective
Patients were stabilized on lithium monotherapy for an
average of 14.4 ± 9 years
(48)
(84)
(42)
99 controls
61 BD
(29R, 16NR,
16PR/UN)
No
(only a
PLCG1-8
repeat was
more
frequent
among R)
Retrospective
Retrospectively subclassified as lithium R, NR, or PR/UN
according to the clinical history, with comparison of the
frequency, duration and severity of episodes before and
after lithium therapy.
(49)
No
Retrospective
Response to lithium: assessed using the scale of Grof et al.
(24).
(45)
Yes
Prospective
(54)
282 BD (148R,
134NR)
Yes
Retrospective
NR3C1
115 BD
(30ER, 58PR,
27NR)
Yes
Retrospective
GSK3β
88 BD I lithium
responders
Yes
Prospective
134 BD I
No
Retrospective
89 BD
(23 ER, 47 PR,
19 NR)
No
Retrospective
184 BD
(92R, 92NR)
282 BR (148R,
134NR)
No
Retrospective
No: alone
Yes: when
GSK3β and
NR1D1
genotypes
were
considered
together
No
Retrospective
R: minor or modest improvement in frequency of episodes
or admissions.
R: if there was a 50% reduction in the frequency and/or
severity of symptoms on Li.
NR: if less than 50% symptom reduction.
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to pre-lithium period
NR: < 50% reduction, no change or worsening in the
episode index, defined as number of episodes per year
compared to the pre-lithium period.
Efficacy of lithium was evaluated by calculating the
difference between the “pre-lithium treatment recurrence
index” and the “on-lithium treatment recurrence index”.
R ‘‘ Good responders’’: no recurrence of impairing
symptoms, or recurrence of mild symptoms, promptly
controlled by adjusting the lithium dose or with short
courses of benzodiazepines but no other medication.
PR: lithium level ≥0.6 mEq/l with improvement of the
recurrence pattern in spite of being mildly depressed or
hypomanic while on monotherapy.
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to pre-lithium period
NR: < 50% reduction, no change or worsening in the
episode index, defined as number of episodes per year
compared to the pre-lithium period.
R: rated retrospectively from standardized interviews and
medical records
R: if there was a 50% reduction in the frequency and/or
severity of symptoms on Li.
NR: if less than 50% reduction of symptoms.
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to pre-lithium period
NR: < 50% reduction, no change or worsening in the
episode index
CRY1
282 BR (148R,
Yes
Retrospective
R: if there was a 50% reduction in the frequency and/or
134NR)
severity of symptoms on Li.
NR: if less than 50% reduction of the symptoms.
The neurotransmitter system: serotonin, dopamine and GABA pathways
DRD1
155 BD
No
Retrospective
The response to lithium was assessed using the scale
(43R, 112PR +
developed by Grof et al. (24)
NR)
92 BD
Yes
Retrospective
ER: no affective episodes on lithium
(24ER, 48PR,
PR: 50% reduction in the episode index, defined as number
20NR)
of episodes per year compared to the pre-lithium period
NR: < 50% reduction, no change or worsening in the
episode index, defined as number of episodes per year
compared to the pre-lithium period.
101 BD
Yes
Retrospective
ER: no affective episodes on lithium
(24ER, 51PR,
PR: 50% reduction in the episode index, defined as number
26NR)
of episodes per year compared to pre-lithium period
NR: < 50% reduction, no change or worsening in the
episode index
DRD2
125 patients
No
Prospective
Efficacy evaluated by the difference between a pre(100BD;
treatment index and an ongoing treatment index
25MD)
155 BD
No
Retrospective
The response to lithium was assessed using the scale
(43R, 112PR +
developed by Grof et al. (24)
(86)
The circadian signaling system
NR1D1
199 BD lithium
responders
(57FR,
142PR+NR)
170 BD
101 BD
(24ER, 51PR,
26NR)
16
Retrospective
(55)
(56)
(51)
(40)
(52)
(84)
(55)
(55)
(45)
(63)
(86)
(57)
(45)
NR)
101 BD
(24ER, 51PR,
26NR)
DRD3
DRD4
DAT1
GABRA1
GABRA3
GABRA5
GABRB3
5-HT1A
5-HT2A
No
Retrospective
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to the pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index
The response to lithium was assessed using the scale
developed by Grof et al. (24)
(86)
155 BD
(43R, 112PR +
NR)
55 patients
(43BD; 12MD)
101 BD
(24ER, 51PR,
26NR)
No
Retrospective
No
Prospective
Efficacy evaluated as the difference between a pretreatment index and an ongoing treatment index
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to the pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index
Efficacy evaluated as the difference between a pretreatment index and an ongoing treatment index
(58)
No
Retrospective
125 patients
(100BD;
25MD)
101 BD
(24ER, 51PR,
26NR)
No
Prospective
No
Retrospective
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to the pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index
The response to lithium response was assessed using the
scale developed by Grof et al. (24)
(86)
155 BD
(43R, 112PR +
NR)
125 patients
(100BD;
25MD)
a) 138 BDI
lithium
responders and
108 controls
b) 24 families
ascertained
through
lithiumresponsive BD
probands
a) 138 BDI
lithium
responders and
108 controls
b) 24 families
ascertained
through
lithiumresponsive BD
probands
a) 138 BDI
lithium
responders and
108 controls
b) 24 families
ascertained
through
lithiumresponsive BD
probands
124 patients
(102BD;
22MD)
124 patients
(102BD;
22MD)
155 BD
(43R, 112PR +
NR)
92 BD
(24ER, 48PR,
20NR)
No
Retrospective
No
Prospective
Efficacy evaluated as the difference between a pretreatment index and an ongoing treatment index
(57)
a) No
b) No
Prospective
Patients were stabilized on lithium monotherapy
(67)
a) No
b) No
Prospective
Patients were stabilized on lithium monotherapy
(67)
a) No
b) No
Prospective
Patients were stabilized on lithium monotherapy
(67)
No
Prospective
(59)
No
Prospective
No
Retrospective
Efficacy evaluated as the difference between a pre-lithium
treatment recurrence index and an on-lithium treatment
recurrence index
Efficacy evaluated as the difference between a pre-lithium
treatment recurrence index and an on-lithium treatment
recurrence index
The response to lithium response was assessed using the
scale developed by Grof et al. (24)
No
Retrospective
(64)
No
Retrospective
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to the pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index, defined as number of episodes per year
compared to the pre-lithium period.
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to the pre-lithium period
NR: < 50% reduction, no change or worsening of the
101 BD
(24ER, 51PR,
26NR)
(45)
(86)
(57)
(45)
(59)
(45)
(86)
17
5-HT2C
5HTTLPR
124 patients
(102BD;
22MD)
92 BD
(24ER, 48PR,
20NR)
No
Prospective
No
Retrospective
101 BD
(24ER, 51PR,
26NR)
No
Retrospective
201 patients
(167BD,
34MD)
Yes
(s/s and
worse
response)
Yes
(l/s and
better
response)
Yes
(s/s and s
and worse
response)
Prospective
Interaction
between
BDNF and
5HTTLPR
polymorphis
m and the
response to
lithium
No
Retrospective
155 BD
(43R, 112PR +
NR)
101 BD
(24ER, 51PR,
26NR)
No
Retrospective
Yes
Retrospective
201 patients
(160 BD +
41MD
characterized
for lithium
response)
101 BD
(24ER, 51PR,
26NR)
No
Prospective
Yes
Retrospective
201 patients
(160 BD +
41MD
characterized
for lithium
response)
a) 138 BD and
108 controls
b) 25 families
ascertained
through
lithiumresponsive BD
probands
201 patients
(160 BD +
No
Prospective
a) No
b) No
No
83 BD
(36R, 47NR)
67 BD
(18ER, 35PR,
14NR)
121 BD
(31ER, 54PR,
26NR)
134 BD I
COMT
MAO-A
Gβ3
18
episode index
Efficacy evaluated as the difference between a pre-lithium
treatment recurrence index and an on-lithium treatment
recurrence index
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to the pre-lithium period
NR: < 50% reduction, no change or worsening in the
episode index, defined as number of episodes per year
compared to the pre-lithium period.
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to the pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index
Efficacy evaluated as the difference between a pre-lithium
treatment recurrence index and an on-lithium treatment
recurrence index
(59)
(64)
(86)
(60)
Prospective
Efficacy evaluated as the difference between a pre-lithium
treatment recurrence index and an on-lithium treatment
recurrence index
(65)
Retrospective
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index, defined as number of episodes per year
compared to the pre-lithium period.
ER: no affective episodes
PR: 50% reduction in the number of episodes per year
compared to the pre-lithium period
(66)
R ‘‘ Good responders’’: no recurrence of impairing
symptoms, or recurrence of mild symptoms, promptly
controlled by adjusting the lithium dose or with short
courses of benzodiazepines but no other medication.
PR: lithium level ≥0.6 mEq/l with improvement of the
recurrence pattern in spite of being mildly depressed or
hypomanic while on monotherapy.
The response to lithium was assessed using the scale
developed by Grof et al. (24)
(40)
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to the pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index
Efficacy evaluated as the difference between a pre-lithium
treatment recurrence index and an on-lithium treatment
recurrence index
(86)
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year compared to pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index
Efficacy evaluated as the difference between a pre-lithium
treatment recurrence index and an on-lithium treatment
recurrence index
(86)
Prospective
The response to lithium was evaluated prospectively with
an average follow-up of 14.4 ± 6.8 years.
(69)
Prospective
Efficacy evaluated as the difference between a pre-lithium
treatment recurrence index and an on-lithium treatment
(68)
Retrospective
(61)
(45)
(68)
(68)
TPH
TH
41MD
characterized
for lithium
response)
108 patients
(90BD + 18MD
characterized
for lithium
response)
54 BD lithium
responders (48
BD and 6 RU)
94 controls
recurrence index
Yes
Prospective
Efficacy evaluated as the difference between a pre-lithium
treatment recurrence index and an on-lithium treatment
recurrence index
(70)
No
Retrospective
ER: patients judged to have a high risk of recurrence on the
basis of the number and frequency of episodes before
lithium therapy. Maintained on lithium monotherapy for ≥3
years, at plasma levels ≥0.6 mEq/l, with no further
episodes of the illness while on adequate treatment. No
additional biological or pharmacological interventions
allowed.
(71)
Retrospective
ER: had no affective episodes on lithium;
PR: showed 50% reduction in the episode index (number
of episodes per year relative to that during the pre-lithium
period);
NR : showed <50% reduction, no change, or worsening of
the episode index.
ER: had no affective episodes on lithium;
PR: showed 50% reduction in the episode index (number
of episodes per year relative to that during the pre-lithium
period);
NR: showed <50% reduction, no change, or worsening of
the episode index.
R ‘‘ Good responders’’: no recurrence of impairing
symptoms, or recurrence of mild symptoms, promptly
controlled by adjusting the lithium dose or with short
courses of benzodiazepines but no other medication.
PR: lithium level ≥0.6 mEq/l with improvement of the
recurrence pattern in spite of being mildly depressed or
hypomanic while on monotherapy.
The response to lithium was rated retrospectively from
standardized interviews and medical records
ER: had no affective episodes on lithium;
PR: showed 50% reduction in the episode index (number
of episodes per year relative to that during the pre-lithium
period);
NR: showed <50% reduction, no change, or worsening of
the episode index.
R: Less frequent and/or severe relapses, including no
relapse, by comparison with the period before the initiation
of lithium treatment
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, defined as number
of episodes per year, since the pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index
ER: had no affective episodes on lithium;
PR: showed 50% reduction in the episode index (relative to
that during the pre-lithium period);
NR: showed <50% reduction, no change, or worsening of
the episode index.
The response to lithium was rated retrospectively from a
standardized interviews and medical records
(45)
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, from that during
the pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index
ER: had no affective episodes on lithium;
PR: showed 50% reduction in the episode index (from that
during the pre-lithium period);
NR: showed <50% reduction, no change, or worsening of
the episode index.
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, from that during
the pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index
ER: had no affective episodes on lithium;
PR: showed 50% reduction in the episode index (from that
during the pre-lithium period);
(86)
The BDNF/TrkB signaling pathway
BDNF
88 BD
Yes
characterized
for response to
lithium
NTRK2
108 BD
(25ER, 55PR,
28NR)
Yes
Retrospective
134 BD I
No
Retrospective
184 BD
(92R, 92NR)
121 BD
(31ER, 54PR,
26NR)
No
Retrospective
Yes
Retrospective
161 BD
No
Retrospective
101 BD
(24ER, 51PR,
26NR)
Yes
Retrospective
108 BD
(25ER, 55PR,
28NR)
No
Retrospective
184 BD
(92R, 92NR)
Yes
(in BD with
suicidal
ideation)
No
Retrospective
101 BD
(24ER, 51PR,
26NR)
Yes
Retrospective
101 BD
(24ER, 51PR,
26NR)
Yes
Retrospective
105 BD
(24ER, 53PR,
28NR)
No
Retrospective
101 BD
(24ER, 51PR,
26NR)
FYN
GRIN2B
Retrospective
(73)
(40)
(84)
(61)
(74)
(86)
(73)
(84)
(75)
(86)
(76)
19
101 BD
(24ER, 51PR,
26NR)
Other signaling pathways
CREB1
249 BD (180R,
69NR)
and 127
controls
No
Retrospective
Yes
Prospective
CREB2
CREB3
249 BD (180R,
69NR)
and 127
controls
No
Prospective
PREP
249 BD (180R,
69NR)
and 127
controls
No
Prospective
XBP1
66 BD
Yes
Retrospective
BCR
161 BD (43R,
118NR)
134 BD I
Yes
Retrospective
No
Retrospective
155 BD
(43R, 112PR +
NR)
a) 213 BD I
b) 170 BD
No
Retrospective
a) Yes
b) Yes
Retrospective
109 BD (26ER,
55PR, 28NR)
No
Prospective
101 BD
(24ER, 51PR,
26NR)
No
Retrospective
AP2-B
PDLIM5
CACNG2
MMP-9
NR: showed <50% reduction, no change, or worsening of
the episode index.
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, from that during
the pre-lithium period
NR: < 50% reduction, no change or worsening of the
episode index
(86)
ER: Each patient had to fulfill several criteria: A)
Diagnosis of primary episodic bipolar disorder based on
the SADS-L (lifetime version) interview and Research
Diagnostic Criteria (RDC); B) High recurrence risk; and C)
Unequivocal response to lithium
NR: had to experience at least two recurrences during
lithium treatment with confirmed therapeutic levels of
lithium
ER: Each patient had to fulfill the following criteria: A)
Diagnosis of primary episodic bipolar disorder based on
the SADS-L (lifetime version) interview and Research
Diagnostic Criteria (RDC) ; B) High recurrence risk ; and
C) Unequivocal response to lithium
NR: had to experience at least two recurrences during
lithium treatment with confirmed therapeutic levels of
lithium
ER: Each patient had to fulfill the following criteria: A)
Diagnosis of primary episodic bipolar disorder based on
the SADS-L (lifetime version) interview and Research
Diagnostic Criteria (RDC) ; B) High recurrence risk ; and
C) Unequivocal response to lithium
NR: had to experience at least two recurrences during
lithium treatment with confirmed therapeutic levels of
lithium
R: Less frequent and/or severe relapse, including no
relapse, than during the period before the initiation of
lithium treatment
R: full response without any affective episode during
lithium treatment (=ER).
R ‘‘ Good responders’’: no recurrence of impairing
symptoms, or recurrence of mild symptoms, promptly
controlled by adjusting the lithium dose or with short
courses of benzodiazepines but no other medication.
PR: lithium level ≥0.6 mEq/l with improvement of the
recurrence pattern in spite of being mildly depressed or
hypomanic while on monotherapy.
The response to lithium was assessed using the scale
developed by Grof et al. (24)
(77)
NR: no improvement or worsening of illness
PR: minor or modest improvement in frequency of
episodes or admissions; significant morbidity
R: partial good response (marked improvement but not
episode-free)
FR: good response (complete remission).
ER: no affective episodes during lithium treatment;
PR: 50% or more reduction in the episode index;
NR: less than 50% reduction, no change or worsening of
the episode index.
ER: no affective episodes on lithium
PR: 50% reduction in the episode index, since the prelithium period
NR: < 50% reduction, no change or worsening of the
episode index
(83)
(77)
(78)
(80)
(81)
(40)
(82)
(85)
(86)
BD: bipolar disorder; MD: major depression; RU: recurrent unipolar; ER: excellent responders; FR: full responders; R:
responders; PR: partial or poor responders; NR: non responders; UN: unclassified. 5-HT1A: 5-hydroxytryptamine receptor 1A; 5HT2A: 5-hydroxytryptamine receptor 2A; 5-HT2C: 5- hydroxytryptamine receptor 2C; 5-HTT: solute-carrier family 6 member 4
(serotonin transporter); 5-HTTLPR: serotonin-transporter-linked promoter region; AP2-B: activating enhancer- binding protein 2
beta 3; BCR: breakpoint cluster region; BDNF: brain-derived neurotrophic factor; CREB1: cAMP-responsive element-binding
protein 1; COMT: catechol-O-methyl transferase; CREB2: cAMP-responsive element-binding protein 2; CREB3: cAMPresponsive element-binding protein 3; CRY1: cryptochrome-1 ; DAT1: dopamine transporter 1; DGKH: diacylglycerol kinase,
eta; DRD1: dopamine receptor D1; DRD2: dopamine receptor D2; DRD3: dopamine receptor D3; DRD4: dopamine receptor D4;
GABRA1: gamma-aminobutyric acid A receptor, alfa 1; GABRA3: gamma-aminobutyric acid A receptor, alfa 3; GABRA5:
gamma-aminobutyric acid A receptor, alfa 5; GABRB3: gamma-aminobutyric acid A receptor, beta 3; Gβ3: G protein beta 3;
GRIN2B: NMDA receptor 2B subunit ; GRK3: beta-adrenergic receptor kinase 2 (BARK2); GSK3B: glycogen synthase kinase 3
beta; FYN: Src-family tyrosine kinases; IMPA1: inositol(myo)-1(or 4)-monophosphatase 1; IMPA2: inositol(myo)-1(or 4)monophosphatase 2; INPP1: inositol polyphosphate-1-phosphatase; MAO-A: monoamine oxidase A; MARKS: myristoylated
20
alanine-rich C-kinase substrate; group D, member 1; MMP-9: matrix metalloproteinase-9; NR1D1: nuclear receptor subfamily 1,
group D, member 1; NR3C1: nuclear-receptor subfamily 3, group C, member 1 ; NTRK2: neurotrophic tyrosine kinase, receptor,
type 2; PDLIM5: PDZ and LIM domain 5; PLCG1: phospholipase C, gamma 1; PREP: propyl endopeptidase; TH: tyrosine
hydroxylase; TPH: tryptophan hydroxylase; XBP1: X-box-binding protein 1.
21
Table 2. Pharmacogenetic studies of the response of bipolar disorder patients to non-lithium mood stabilizers
Gene
Sample
Valproate (VPA)
51 BD patients
XBPI
Association
(Yes/No)
Yes
Lamotrigine
DRD2
Yes
DRD3
No
DRD4
No
85 lamotrigineDBH
Yes
treated, BD I
depression patients
HRH1
Yes
ANKK1
No
MCR2
Yes
NR3C1
Yes
Atypical antipsychotics
DRD2
No
DRD3
Yes
88
DRD4
No
olanzapine/fluoxetine
DBH
No
combination (OFC)HRH1
Yes
treated BD I
ANKK1
No
depression patients
MCR2
No
NR3C1
No
SLC6A2
88
Yes
olanzapine/fluoxetine
MCR3
Yes
combination (OFC)TPH2
Yes
treated BD I
depression patients
COMT
42 BD patients
No
characterized for
response to
olanzapine
Common to Lithium, VPA and carbamazepine
144 BD patients
characterized for
response to mood
COMT
Yes
stabilizers (Li, VPA,
CBZ)
and 157 controls.
Study design
Definition of response
References
Retrospective
Less frequent and/or severe relapse, including no relapse, than
during the period before the initiation of valproate treatment
(91)
Prospective
Reduction in Montgomery-Asberg Depression Rating Scale
(MADRS) total score between baseline and week 7.
(93)
Prospective
Reduction in Montgomery-Asberg Depression Rating Scale
(MADRS) total score between baseline and week 7.
(93)
Prospective
Reduction in Montgomery-Asberg Depression Rating Scale
(MADRS) total score between baseline and week 7.
(95)
Prospective
Prospective
Clinical status evaluated before treatment, after 4 days of
treatment and subsequently every week, with the Young scales
for mania and the Andreasen scale for positive symptoms.
Response defined as subjects exhibiting a decrease of at least
50% in the YMRS score after 6 weeks of medication.
(96)
(92)
BD: bipolar disorder; R: responders; NR: non responders. ANKK1: ankyrin repeat and kinase domain containing 1; COMT:
catechol-O-methyl transferase; DBH: dopamine beta-hydroxylase; DRD2: dopamine receptor D2; DRD3: dopamine receptor D3;
DRD4: dopamine receptor D4; HRH1: histamine H1 receptor; MCR2: melanocortin 2 receptor; MCR3: melanocortin 3 receptor ;
NR3C1: nuclear receptor subfamily 3, group C, member; SLC6A2: norepinephrine transporter ; TPH2: tryptophan hydroxylase 2
; XBP1: X-box-binding protein 1.
Figure 1. Goals of the pharmacogenomics research in bipolar disorder.
Running title: Predicting response to mood stabilizers