Explanatory memorandum
advertisement

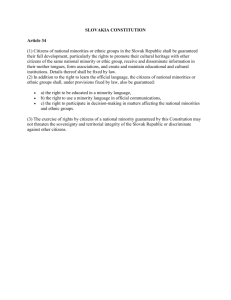
________________________ COMMITTEE OF EXPERTS ON HEALTH SERVICES IN A MULTICULTURAL SOCIETY (SP-SSM) EXPLANATORY MEMORANDUM ADAPTING HEALTH CARE SERVICES TO CULTURAL DIVERSITY IN MULTICULTURAL EUROPE EXPLANATORY MEMORANDUM I. INTRODUCTION Thanks to migration Europe grows in diversity and continues to develop into a multicultural society. Quantitative information on the health status of ethnic minorities remains scarce in most European countries. Still, there are many indications that when compared with the indigenous population, ethnic minorities are more susceptible to illness and suffer from a wider variety of ailments. In addition, relatively little information exists on the accessibility of the health care system for ethnic minorities, the quality of care they receive, their satisfaction with care and problems experienced by them in the health care system. A growing body of research literature seems to indicate, however, that health care services are often insufficiently adapted to the cultural diversity of the clientele they are trying to serve. The term “ethnic minority” refers to those groups of individuals that feel kinship with each other because of a (subjective) belief in a common origin, in some cases a common language, a shared culture, a sort of collective consciousness shared by everyone in the group regardless of social position. Although the recommendation and this explanatory memorandum focus mainly on the issue of (cultural) diversity and its management in relation with the presence of ethnic minorities in Europe, the experts want to stress that diversity should be viewed as a feature of the population as a whole. For that reason, diversity management should become an integrated part of the organisation of health care for the general population. A. A few notes on the health status of ethnic minorities Research has made clear that certain diseases and causes of death are much more frequent in certain ethnic groups than others. Thalassemia does not exist in the indigenous Western-European population but is a rare – but important – health problem among people coming form the Mediterranean region (Schulpen, 1994). Sickle cell anaemia is another case in point: this disease is in Western Europe only found in black ethnic minorities (especially in the UK) (Ahmad, 2000). Relatively well studied is the domain of perinatal and infant mortality: it tends to be much higher in ethnic minority groups than in the indigenous population. Among “North-Africans”1 living in Belgium, it is 14.4 per thousand, among “Turks” 17.7 per thousand as compared with 10.7 per thousand in the indigenous Belgian population (Peeters & De Muynck, 1994). Data on perinatal death are important as they are 1 . Turks, Moroccans etc. are used to refer to the national origin, not the actual nationality of the persons involved. 2 considered to be one of the most objective indicators of the health of a population (Schulpen, 1996). In addition, Dutch research indicates that the mortality in ethnic minority children with a Moroccan or Turkish background is twice as high as among the Dutch (Van Steenbergen et al., 1996). In Germany it was found in 1999 that out of 1000 healthy born migrant children, an average of 5,4 died in the first year if their lives. In the German comparison group, their number amounted to 4,4 (German Federal Bureau of Statistics, 2000). Data on other health problems are limited. Type 2 diabetes has been found to be twice as common in the UK among people coming from the Indian subcontinent. Roderick et al. (1994) found that the chances that these people developed final stage renal disease (leading to renal replacement therapy or to a renal transplant) was no less than 10 times as high as among the British. In addition, evidence exists that in some countries barriers may exist to equitable access to transplantation, as was recently observed in Australia for indigenous Australians (Cass, Cunningham, Snelling et al., 2003). Even more importantly, a number of studies indicate that the overall health status of ethnic minorities is worse. The Netherlands is one of the few countries that organised health surveys among a number of ethnic groups.2 From the health survey among Turkish inhabitants of Holland it was concluded that all the data collected indicated that the perceived (and up to a limited degree objective) health of the Turks compared unfavourably with that of the Dutch. About 25% of the Turks described their own health status as ‘not so good’. Among the Dutch, this was the case for about 11% of the population. More than 33% of the Turks were suffering from at least one chronic condition (25% among the Dutch). The prevalence of obesity (defined as a Quetelet index > 27) was 33% among Turks; this is more than twice as high as among the Dutch (CBS, 1991). B. Explaining the ethnic patterning of health The analysis of ethnic health patterns has been informed by the debate on class (or socioeconomic) inequalities in health. Attention to this question first rose with the publication of the Black Report in 1980 in the UK. To account for the inverse association between social class and premature mortality the Black report proposed four categories of explanation: artefact, selection, cultural and material, arguing in favour of material explanations (i.e. the direct or indirect effects of environmental and economic deprivation) as the principal factor. Andrews and Jewson (1993) and Smaje (1996) have expanded this framework for examining the ethnic patterning of health. It incorporates the following categories: Biological/genetic factors Cultural factors Material factors – socio-economic factors 2 . A number of authors have argued that general health surveys are ill-suited to collect data on the health of ethnic minorities (see e.g. Bhrolchain, 1990). 3 Migration factors Racism Selective impact of health care – quality of care As the discussion on the determinants of ethnic health patterns is of crucial importance for every initiative aiming to improve the health of ethnic minorities, we will give a brief overview of current views on the subject. The theme was also discussed at length during the meetings of the Committee of Experts. 1. Biological/genetic factors: up to date, it remains unclear up to which degree biological/genetic factors may contribute to ethnic health patterns (Bradby, 1995; Smaje, 1996; Senior & Bhopal, 1994). Certain diseases and causes of death are much more frequent in certain ethnic groups than others: thalassemia and sickle cell anaemia are classic examples. In general, a number of studies indicate that the overall health status of ethnic minorities is worse, but the data are limited. 2. Cultural factors have also been used to explain ethnic health patterns. Reference has been made to types of behaviour that are considered to be typical of certain ethnic minorities. A very controversial example in many Western-European countries is female circumcision as practised in countries like Somalia, Egypt etc. Research has made clear that culture may play an important role in shaping the help seeking behaviour of people. The fact that first generation Moroccan women do not consider pregnancy to be a condition that requires medical attention, is, without doubt, one of many reason why they do not show up in time at pre-natal clinics in Belgium (Verrept & Timmerman, 2001). Views of the majority population as ‘impure’, as exist among travellers and Roma, may also constitute a barrier to the use of the health care system. Explanatory models employed by certain ethnic groups – but not shared by the majority – may lead to the consumption of traditional health care services in the host country or the country of origin. In addition, certain sectors of the health care system may be perceived as too stigmatising to rely on it. This has been found to be the case for psychiatric treatment in ethnic groups in the UK (Donovan, 1984). Results of medical anthropological and psychiatric research indicate the existence of culture-bound syndromes, especially in the domain of mental health (Kleinman & Good, 1985; Kleber, 1996). These are a group of folk illnesses, each of which is unique to a particular culture or geographical area. Each is a specific cluster of symptoms, signs or behavioural changes recognized by members of those cultural groups, and responded to in a standardized way (Helman, 1990). As they do not correspond with biomedical categories, health professionals may deny their existence which – to members of the cultural groups involved – is self-evident. As such, culture-bound syndromes may be a source of confusion and misunderstanding between health professionals and patients. Explaining ethnic health differences using cultural factors, has been bitterly attacked by many social scientists for ethnocentrism, covert racism, diverting attention from racism, ‘blaming the victim’, reification and gross oversimplification (Andrews & Jewson, 1993). This critique is increasingly being voiced by researchers who themselves are members of ethnic minority groups. The operationalisation of ‘culture’ is often described as unclear 4 and inadequate (Sheldon & Parker, 1992). The specific cultural phenomena that lead to health inequalities and or an inadequate use of health care services are rarely spelled out. Cultural factors seem to be used when no other factors can be called in to account for observed health disparities between different ethnic groups. What is meant by culture often comes down to aspects of lifestyle, diet, contraceptive practice etc. A number of authors have pointed out the falsification involved in emptying the concept of culture of its complexity and reducing it to lifestyle. The culture of ethnic minorities is frequently reduced to a series of backward opinions and types of behaviour, which may not even be very specific for the ethnic minority concerned. This reduction of culture implicitly confirms the majority’s opinion of their own cultural superiority. Once culture has been ‘proved’ to be the cause of health problems of ethnic minorities, ‘changing the culture’ may be viewed as a useful strategy to resolve them (Donovan, 1984; Van Dijk, 1989). Over the last decades, many projects have been set up to change a number of aspects of the behaviour of ethnic minorities as ways to improve their health status. A number of these, for instance the Asian Mother and Baby Campaign that ran in the UK in the eighties, have met with fierce opposition from the groups they were supposed to be helping (Verrept, 1995). Authors like Smaje (1996) have in addition pointed out that cultural values and practices of ethnic minorities that differ from those of the majority population are easily considered to be deviant or pathogenic in what they describe as a racialised society. The social construction of normality tends to be based on majority middle class behaviours. Bowler (1993) argues that black and working class mothers were excluded from studies of normal motherhood in the UK, but were included in studies of deviance. A narrow focus on cultural issues denies the importance of class or socio-economic status, age, sexual orientation, gender identity, geographic location, physical and mental ability that may all distinctly affect any group’s health needs, interests and concerns. The scientific literature suggests that cultural differences may account for less of the health inequalities between ethnic minorities and the dominant majority population, than used to be thought. 3. Material / socio-economic factors may very well account for most of the ethnic health disparities. Ever since the publication of the Black Report (1990), it has been argued that factors such as poverty, unemployment, unhealthy living conditions, occupational hazards etc. negatively affect life expectancy and health. Interestingly, a number of studies have been carried out trying to investigate independent effects of ethnicity on health. In such studies, the health status of ethnic minorities was compared with that of the majority: in the analysis of the data, the effects of socio-economic status were controlled for. Unfortunately, this research did not always clarify matters. It was found that socio-economic inequalities roughly seemed to correspond with health disparities as well for the ethnic minorities as for the majority population. Still, ethnic minorities were observed to be most vulnerable for health problems within every socio-economic class. This phenomenon may not be caused by cultural differences however. The cross-cultural validity of traditional instruments to 5 measure socio-economic status has been questioned by a number of researchers. They argue that ethnic minorities may systematically occupy the least favourable positions within each socio-economic class (Andrews & Jewson, 1993; Smaje, 1996). As regards the possible influence of cultural and material factors on ethnic health disparities, Smaje says that: [the] “debate has become ensnared in a largely political opposition between, on the one hand, a (radical) emphasis on the material or structural determinants of health, and, on the other, a (conservative) privileging of cultural explanations (…)”. 4. Migration factors Although migration itself may lead to live saving and health improvement, especially for people who managed to escape from poverty, violation of human rights or torture, migration factors, or rather, processes related with the migratory experience, have traditionally been linked with health problems of ethnic minorities. This is self-evident for first-generation migrants. Findings in recent research seem to indicate that migration may even exert influence on the health of third generation migrants (Meurs, 2003). Health determinants in the country of origin and import pathology both affect the health of ethnic minorities. Selection mechanisms (e.g. the selection of workers organised by host countries) may positively affect the overall health status of ethnic minorities (the so-called healthy migrant effect). This is not the case, however, for refugees who may, in addition, be suffering from PTSD as a result of persecution and torture. Finally, a number of authors have suggested that negative selection mechanisms may also be relevant for the health of ethnic groups, as with socially marginal, and perhaps mentally ill, people moving from communities that cannot support them. It is generally accepted that the psychosocial effects of migration may exert an influence on the health of the migrant. The ‘culture shock’, the feelings of loss and alienation that accompany the migration process of many immigrants may act as important stress factors. As a result, migrants may suffer more mental health problems. Unfortunately, reliable data on the mental health status of migrants and ethnic minorities remain scarce. Migration-related stress may affect the well being and health of the children of migrants. This is especially true for children of refugees (Begemann, 1996). The loss of social relations in the country of origin, the separation from loved-ones, changes in gender relations in the host country, financial commitments to those who stayed in the country of origin and tensions between parents and their more acculturated (often called ‘westernised’) children have been argued to be important stresses affecting the health of migrant families (Smaje, 1995). 5. Racism and discrimination, without any doubt, exert an influence on the health status of ethnic minorities. Although poorly researched, the experience of racism and discrimination seems to have a direct and negative impact upon health (Smaje, 1995). As racism inflects the socio-economic position of ethnic minority groups, it also indirectly affects the health of 6 these groups. The existence of racist and discriminatory practices in health care has been poorly investigated in Western Europe, but much more in Central Europe, especially in the context of health care delivery to Roma-people (EUMC, 2003; Brazinova, 2003). From this research, it has become clear that the access and outcome of health care services may be seriously hampered by the widespread existence of structural discrimination in society and health care. 6. Selective impact of health care and social services – quality of care of care received by ethnic minorities3 are factors that are increasingly linked to ethnic health inequalities (Murray-Garcia, 2002). Reference has been made to problems of access, the lack of culture competence in health care providers, lack of special provisions (such as interpreter services, translated health education material) which may all be structural barriers to quality care. Because of legal, financial, linguistic or cultural reasons, it may be impossible or very difficult for ethnic minorities to access the health care system, or to receive the same quality of care as the majority population. In Member States such as Armenia, health care services are financially inaccessible for a large section of the indigenous population and even more so for settled and non-settled refugees. 35% of the indigenous Armenian population can not access the health care system because of financial barriers. The situation of non-settled and settled refugees is even worse in this respect with 46% of non-settled and 44% of settled refugees that are unable to pay to access the health care system (Melikyan, 2003). Mental health services seem to be very inaccessible for ethic minorities in some countries such as Austria (Csitkovics & Schmidl, 2004), Belgium (Verrept & Timmerman, 2001) and the USA (Smedley, Stith & Nelson, 2003). Many prevention programs do not or insufficiently reach ethnic minorities (Csitovics & Schmidl, 2004; Naish, Brown & Denton, 1994; CEMG, 1997). But problems are not limited to access. Once ethnic minority patients have accessed health care services, the quality of care they receive may be lower than that received by patients of the majority population. Research on the management of diabetes has made clear that glycaemia is often less well-controlled in ethnic minority patients (Hawthorne, 1990; Chin, Zhang & Merrell, 1998). In this last study, it was observed that even after controlling for patients’ gender, education and age, African-Americans were less likely to undergo a measurement of glycosylated haemoglobin, lipid testing, ophthalmologic visits, and influenza vaccinations than white patients. They were also more likely to use hospital emergency departments and had fewer physician visits. These phenomena can be interpreted as indicators of less adequate care provision for this group. This may be one of the reasons why ethnic minority diabetics develop more complications, such as blindness, renal failure, and diabetic feet. Guadagnoli et al. (1995) found that AfricanAmericans were twice as likely as whites to undergo above-knee amputation, controlling for co-morbid disease, prior hospitalizations, geographic region, hospital teaching status, and other factors. 3 . We define quality of care as ‘the degree to which health services and individuals increase the likelihood of desired health outcomes and are consistent with current professional knowledge’ (SMEDLEY, STITH AND NELSON, 1999). 7 Health education material on e.g. the management of diabetes have been found to be inadequate for ethnic minorities: cultural factors, such as eating habits, were insufficiently taken into account and led to poor adherence to treatment (O’Neil, Kaufert & Koolage 1986). Differential treatment of ethnic minorities has been studied in some detail in the USA, but much less in Europe. Differential impact of health care services may be linked to discriminatory practices in the health care system, inadequate health care concepts and structures dealing with diversity but also to a lack of skills of the health professionals. As a result, the health care interventions may be less effective and patients may be less satisfied (Borde, 2001). This may in its turn affect their willingness to make use of the health care system. Even more so than in other areas of health and medicine, mental health services seem to be plagued by the disparities in the availability and access to its services (US DHHS, 2001). Research in Holland has demonstrated that ethnic minority patients were very dissatisfied with the quality of care received in mental health care centres. As a result, treatments were very often prematurely abandoned. Interestingly, health professionals seemed to agree with their patients on the fact that quality of care they delivered was below standards Unresolved language barriers have been proved to dramatically affect the quality of care received by allophone ethnic minority patients (Bowen, 2001; Jacobs et al., 2003). The inability to communicate with health care providers, may lead to the postponement of necessary consultations. Patients’ rights may not be respected when health care providers and patients are unable to communicate with each other. A point of special concern in this respect is the obtaining of meaningful informed consent: Canadian research has made clear that informed consent was often obtained from patients with limited English proficiency using methods that are normally relied upon for patients who are mentally ill, demented or in a state of coma (Kaufert & Putsch, 1997). Systematic studies of the effects of culture barriers are very scarce. This may be related to the elusiveness of the concept of culture. Still, consensus seems to exist that inadequate handling of cultural differences may affect the quality of care and that the development of culture competence or cultural responsiveness would add to the efficiency and effectiveness of health care provision to ethnic minorities (Bischoff, 2003). C. Tasks of the committee of experts on heath services in a multicultural Europe As Europe grows in diversity, health care providers will be increasingly challenged to understand and address the cultural needs of an ethnically diverse clientele. This led to the European Health Committee’s decision to set up a Committee of Experts on Health Services in a Multicultural Society. It was argued that the concepts of health, illness and 8 death are profoundly embedded in the culture of a group or a country and that the manner of treatment and rituals surrounding the dying are conditioned by this culture. This fact is not always sufficiently recognised by the health care services and institutions of Member States. In the terms of Reference, it was further argued that respect for human rights and the dignity of the individual requires that this cultural diversity is taken into account in the delivery of health services. The international interest in ‘culturally responsive care’ parallels recent developments in medicine such as patient-centred care, the enactment of charters of patients’ rights, and the growing importance attached to the outcome of health care interventions and to patient satisfaction. The Committee of experts was asked to: - examine the type of issues with which the health services of Member States are confronted in different cultural contexts and the way they deal with them; propose a model framework for Member States which allows for dealing with patients of different cultural traditions in a practical manner at the various stages of health services and particularly: o the adaptation of the various health services to meet the cultural needs of the patients concerned while taking into account the budgetary and staff implications, as well as the impact of the management of the health services; o Training of health care staff and particularly nurses to be aware of the different cultural needs of patients and their family, and to respond sensitively to such needs. During the discussion of the terms of reference, many experts pointed out that cultural differences might be less of a barrier to equitable health and equitable access to health care services, than other factors. Reference was made to the factors discussed above. It was also argued that it may be unrealistic to draw a clear line between barriers and problems in health care related to cultural factors on the one hand and socio-economic (or other) ones on the other. Because of the well-established link between material factors and ethnic health disparities, and because of the interrelatedness of the different determinants of ethnic health patterns, it was decided to: - - Include recommendations that encourage the development of an integrated social/health policy. This clearly goes beyond the adaptation of health care services to cultural diversity; to adopt a broad definition of culture that recognizes cultural sub-categories based on shared attributes (such as gender) or shared life experiences (such as trauma, education, occupation, socio-economic status, homelessness, being undocumented, …). It is the convergence of multiple memberships in various cultural and subcultural groups that contribute to an individual’s personal identity and sense of their own ‘culture’. Understanding how these factors affect how a 9 - person seeks and uses medical care, as well as their group’s historical relationship to the medical establishment, is an integral part of providing culturally competent care according to the US Department of Health and Human Services (2001); to emphasize that the reduction of health inequalities in multicultural Europe requires the development of a diversity-based analysis policy examining ideas, policies, programs and research to assess their potentially different impact on specific groups of men, women, boys and girls. A narrow focus on cultural issues denies the importance of class or socio-economic status, age, sexual orientation, gender identity, geographic location, physical and mental ability that may all distinctly affect any group’s health needs, interests and concerns (based upon Health Canada’s Gender-based Analysis Policy, 2000). Therefore, the experts advocate a general diversity-based approach that takes into account all sources of diversity that may be relevant to health and health care issues rather than an approach that is limited to dealing with cultural diversity. The experts want to stress that the issue of (cultural) diversity and its management should not be exclusively linked to the presence of ethnic minorities. It is argued that cultural diversity should rather be viewed as a feature of the population of present-day Europe as a whole. D. A note on terminology Unfortunately, there still is no universally accepted terminology to describe migrants and non-native ethnic groups and their off-spring. According to historically and socially determined views on migration, the terms migrants, immigrants, ethnic minorities and ethnic communities may sound perfectly legitimate in one country and offensive in another. In this report, the term ethnic minorities refers to those groups of individuals that feel kinship with each other because of a (subjective) belief in a common origin, in some cases a common language, a shared culture, a sort of collective consciousness shared by everyone in the group regardless of social position (following Weber cit. in Sundquist, 1995). It may be important to point out that the historical background of the presence of ethnic minorities varies enormously between different member states. Some, like Slovakia for example, have harboured large numbers of Roma for centuries. In many WesternEuropean states, such as Germany and Austria, the presence of ethnic minorities is mainly linked to migration processes that accompanied the economic development in the sixties. Some Eastern European Member States have, after the collapse of Communist regimes, developed into sending countries, rather than countries attracting immigrants. This is e.g. the case for Georgia. It is estimated that not less than 600.000 persons have emigrated from Georgia in the years 1990-1996 (Rachvelishvili, 2003). The general term ethnic minorities includes the following groups: 10 - migrants and their off-spring; national minorities (e.g. travellers, ethnic groups that have acquired the citizenship of the country they are living in but that consider themselves to be ‘culturally different’, and/or are considered by the majority as such); - asylum seekers and refugees; - victims of trafficking; In the context of this recommendations many other groups have been identified, which contribute to the societal diversity: - undocumented persons (illegal immigrants, members of ethnic groups that do not have access to documented legal status). people with other than white skin colour religious minorities (for discrimination reasons) linguistic minorities specific disability groups, like deaf persons The experiences of these groups may be very different from each other. As a result, it may be necessary to develop different strategies to adapt health care services to specific health needs of various groups. . Diversity in the population as a whole requires the attention of member states in the domain of health and health care provision. For this reason, the expression ‘ethnic minority’ is used together with expressions such as ‘multicultural populations’ and ‘multicultural society’. II. STRATEGIES FOR THE IMPROVEMENT OF THE HEALTH AND HEALTH CARE FOR MULTICULTURAL POPULATIONS. NON-DISCRIMINATION IN ACCESS TO HEALTH CARE In the following pages, a number of general strategies are recommended to the governments of the Member States and briefly discussed. In addition, a number of particular problem areas that have been identified in the literature and during the discussions of the Committee of Experts, are presented. In some cases, reference is also made to interventions that have been found to be effective to reduce ethnic health (care) disparities. Reference is also made to a number of strategies that are frequently recommended in studies on health policies for ethnic minorities, but that have been insufficiently researched to draw final conclusions on their effectiveness. Recommendations related to specific areas of particular concern 1. Discrimination, racism, respect for patient/human rights It is important to note that discrimination and racism are found in many sectors in the Member States, e.g. in the domains of housing and employment. Racism and 11 discrimination are morally unacceptable, and contribute to the marginalisation and social vulnerability of ethnic minorities. In addition, findings of research suggest that ethnic minorities’ experiences in the world outside the health care practitioner’s office are likely to affect their perceptions and responses in the care settings (e.g. leading to mistrust which in its turn may lead to poor adherence to treatment, delays in seeking care, …) (Smedley, Stith & Nelson, 2003). Discrimination and racism have also been observed in the domain of health care, and this as well at a systemic level as at the level of individual institutions and/or health care providers. In many member states, some ethnic minority groups (e.g. undocumented immigrant) have only very limited access to the health care system (e.g. limited to emergency care). In some member states, certain health care institutions refuse to treat ethnic minority patients. This has been particularly well-documented for Roma patients. In practice, this has led to ethnic segregation of health care services. Ethnic minorities may, as a result of these strategies, only have access to institutions that offer basic or even substandard health care services. Although the idea of racism and discrimination is undoubtedly abhorrent to most health care professionals, racist and discriminatory behaviour in health care settings has repeatedly been reported in the literature. 2. Socio-economic status of ethnic minorities As ethnic health patterns broadly reflect socio-economic differences between ethnic minorities and the majority population, it is essential that governments develop policies to improve the socio-economic status of these minorities. Of special importance is equitable access to food, housing, a healthy environment, education, employment, social and health care services. Improving the socio-economic status of ethnic minorities is the promotion of healthy environment and health behaviour without any doubt, the most effective way to reduce ethnic health disparities. For more details we refer the reader to the Recommendation Rec(2001)12 and explanatory memorandum ‘The adaptation of health care services to the demand for health care and health care services of people in marginal situations” 3. Quality of care Accessibility As Bischoff (2003) has argued, the quality of care is not adequate if it is not provided to all patients. As such access issues should be viewed as quality issues. Smedley, Stith& Nelson (2003) have added that substandard care for some groups, be it related to problems of access or of quality of services delivered, should raise the concern that the provision of care may be inconsistently and subjectively administered. Inequities in care, therefore, expose a threat to the population as a whole. We have already mentioned the existence of legal barriers in some Member States to (publicly funded) health care services. Legal barriers preventing access to health insurance systems (access to the health insurance system may not be possible without 12 legal status and/or working permit, etc.), creates financial barriers to care in different member states. Language barriers pose a problem for many patients where health systems lack the resources, knowledge or institutional priority to provide adequate interpretation services. There is compelling evidence that language barriers have an adverse effect on initial access to health care services. These barriers are not limited to encounters with physician and hospital care. Patients face significant barriers to health promotion/prevention programs (lack of translated health promotion and education material, lack of appropriate methods for reaching marginalized populations with these programs), (Smedley, Stith & Nelson, 2003; Bowen, 2001; Jacobs et la, 2003). Recent research that includes the variables of both ethnicity and official language proficiency suggests that in many cases, language, rather than cultural beliefs and practices of patients, may be the most significant barrier to initial contact with health services. Evidence demonstrates that patients lacking official language fluency also have reduced access to mental health and counselling-related services (Bowen, 2001). Linguistic barriers, combined with low socio-economic status, may also reduce access to information on the functioning and possible benefits of health care services. A lack of knowledge on the health care system and how to use it may hamper access and lead to inadequate use of health care services When cultural differences and cultural needs are insufficiently taken into account (e.g. lack of respect for the values and convictions of ethnic minority patients), this may make health care services culturally unacceptable for these groups, leading to cultural barriers to care. In cultures where modesty is a particular issue, the lack of access to staff members of the same sex may e.g. lead to an unwillingness to rely on health care services for certain health problems. The same holds true when patients are not offered the possibility to have meals that suit their religious and cultural needs at the hospital (Henley & Schott, 1999). When health care institutions lack cultural competence, this may affect the accessibility of the health care system.4 Geographical factors , e.g. the relative scarcity of health care providers and health care services in minority communities and insufficient (affordable) transportation have been found to be significant barriers to equitable care for ethnic minorities (as well in Central and Eastern Europe as in the US) (EUMC, 2003; Oana, 2003; Smedley, Stith & Nelson, 2003). Quality of care delivered to ethnic minorities Especially in the US, research has made clear that ethnic disparities in health care exist. As described in the introduction, a large body of research indicates that ethnic minorities tend to receive a lower quality of health care even when access-related factors, such as 4 . Cultural competence may be defined as the ability to provide effective health care services taking into consideration the individual’s gender, sexual orientation, disability, age and religious, spiritual and cultural beliefs (Bischoff, 2003). 13 patients’ insurance status and income are controlled for. Collectively, the findings of these studies support the hypothesis that patients’ ethnicity significantly predicts the quality and intensity of care that they receive (Smedley, Stith & Nelson, 2003). Unfortunately, data on ethnic health care disparities in Europe are scarce. Still, results of available research and the material collected by the experts should raise the concern of the Member States. Below, we refer to a number of quality issues that have to be addressed if we want to avoid, reduce and ultimately eliminate ethnic health care disparities. Recommendations are advanced that should help Member States to respond adequately to the issues discussed. 4. Quality of communication – language barriers Good patient-provider communication has been shown to have lasting effects over time and directly to improve adherence and health outcomes. The quality of patient-provider communication is therefore a strong indicator of the quality of the health care provided (Bischoff, 2003). A lot of research has been carried out on the effects of language barriers on the quality of care (Bowen, 2001; Jacobs et al., 2003). In the US and Western Europe, resolving language barriers is considered to be the most urgent, evident and straightforward area in which interventions are needed. The following effects of language barriers have been observed:5 - - - - - 5 Relatively little is known on the effects of language barriers on health outcomes. Still, research suggests that there are many intermediate effects (such as reduced comprehension and compliance). Language barriers have been associated with increased risk of hospital admission, increased risk of intubation for asthmatics, differences in prescribed medication, greater number of reported adverse drug reactions, and lower rates of optimal pain management. Language barriers may also be related to less adequate management of chronic diseases such as asthma and diabetes. As a result of language barriers, health care providers may fail to meet ethical standards in providing health care. Language barriers may result in failure to protect patient confidentiality, or to obtain meaningful informed consent (Kaufert & Putsch, 1997). Language barriers have a negative effect on patient satisfaction. A review of the literature reveals consistent and significant differences in patients’ understanding of their conditions and compliance with treatment when a language barrier is present. Language barriers have been found to have a negative effect on provider effectiveness and satisfaction. They make it difficult for health care providers to meet professional standards of care, and may, in certain countries, increase their exposure to the risk of liability. Finally, but not unimportantly, there is some evidence that language barriers may have important effects on health care costs, through their impact on service utilisation and health outcomes. Based on Bowen & Kaufert, 2001. 14 Using untrained interpreters, especially family member, is the most frequently used method of trying to solve the problem of language barriers. A growing body of evidence suggests that the use of informal, untrained interpreters can lead to serious miscommunication, and so to inadequate care. Untrained interpreters may be proficient in both languages but may lack interpreting skills. Poor interpreting leads to misunderstandings, wrong diagnoses and low adherence. Untrained interpreters who are insufficiently familiar with both cultures are unable to provide the necessary intercultural mediation. Relatives, especially children, are also at a high risk of stress disorders themselves, if they have to translate emotionally charged interviews (e.g. about their parents experiences of violence or forced migration) (Bischoff, 2003). Informal interpreters have been found to manipulate messages uttered by health care providers and/or patients to serve their own interests or the perceived interests of the interlocutors (e.g. hiding bad news from the patient) (Es Safi, 1996, ; Verrept, Perissino & Herscovici, 2000). Consensus exists that the provision of professional health care interpreters is an important prerequisite to guarantee equitable access to and quality of care to many ethnic minorities. Professional interpreters may have an important impact on the acceptability of health care services and patient satisfaction in ethnic minority groups. Considerable controversy, however, surrounds the precise definition of the role of the health care interpreter (Bowen, 2001; Tribe & Raval, 2002). Finally, more research is needed to adequately assess the language needs of ethnic minorities in health care and the effects of health care interpreting programs on the quality of care. 5. Responsiveness to health and socio cultural needs of ethnic minorities In some Member States, e.g. the UK, the health care system has been criticized because it did not respond adequately to health problems that were mainly found in ethnic minority groups (e.g. sickle cell disease, Ahmad, 2000). The same may be true for the treatment of health problems that are related to the migration history of ethnic minorities (e.g. the treatment of PTSD in refugees who have been tortured), and mental and other health problems related to the stress of living as an undocumented person or victim of trafficking (Gushulak & MacPherson, 2000). Partly culturally determined beliefs, concepts, types of behaviour, traditions and religious convictions may have a profound impact on the expectations and interactions of ethnic minorities with the health care system. In the literature we find many references to examples of ‘cultural diversity’ that may affect the cross-cultural health care encounter: e.g.: views on nutrition/diet, explanatory models, different types of traditional healing systems, views on surgery and transplantation, autopsy, on communication with the diseased (e.g. the communication of bad news), visiting ill persons, the process of dying and death, religious rituals to be executed at birth/death, gender relationships (acceptability of a health care provider of the opposite sex to the patient), (female) 15 circumcision (infibulation), etc (see e.g. Henley and Schott, 1999). A large body of literature exists that stresses that health care providers should respond adequately to patients’ cultural needs. Cultural competence training has been found to be effective in improving knowledge and behavioural aspects of health care providers and building effective communication strategies. Despite progress in the field, however, several challenges exist, including the need to define educational core competencies, reach consensus on approaches and methodologies, determine methods of integration into the medical and nursing curriculum, and develop and implement appropriate evaluation strategies (Smedley, Stith & Nelson, 2003). The most important aspect of culture competence may well be the ability to communicate clearly, sensitively and effectively with ethnic minority patients, their relatives and colleagues who belong to ethnic minorities. Intercultural communication should, therefore, be part of every program aimed at improving culture competence in health care professionals. Many authors point out that cultural competence training may easily lead to stereotyping of ethnic minorities, especially when they are limited to the transmission of ethnographic knowledge (courses of the ‘cookbook-type, Bischoff, 2003). It has been argued that cultural competence courses should not only focus on knowledge, but also on attitudes (cultural sensitivity, the influence of prejudices), self- assesment of one’s own attitude or behaviour and cross-cultural skills. In addition, the health care sector should try to address issues of cultural diversity in a systematic way (Hoge Raad voor Volksgezondheid, 2001). There is a need for systematic reflection on how to respond to culturally determined wishes and requirements of ethnic minority patients. As was said earlier, cultural differences may only account for a small portion of the health problems experienced by ethnic minorities. The same holds true for the problems experienced by ethnic minority members and health professionals alike during the health care encounter. Structural discrimination in the health care system, the experience of racist and discriminatory practices inside and outside the health care system may seriously affect the expectations of ethnic minority patients and their interaction with the health care system. It is important that health professionals are made aware of these processes learn to detect them, understand their possible impact on the meeting between health care providers and ethnic minority patients, and learn to address these issues. 6. Patient education, empowerment and participation Issues such as improved patient-provider communication and patient-centred care have moved to the forefront in the last decade. As a result, patient education, participation, activation and empowerment have received more attention. Information that flows in both directions is deemed important for increasing patient cooperation, engagement, and 16 adherence to medical regimes (Korsch, 1994 cited in Smedley, Stith and Nelson, 2003). Kaplan & Greenfield (2004) have recently argued that ‘focusing solely on the physicians in the clinical setting is meeting only half the challenge’. They stress the importance of the patient’s role in reducing health disparities. Preparing all patients to make the most of the brief visits to the clinician must be a major focus of future efforts to reduce disparities. Many tested patient training programs have been found to increase patient participation in treatment decisions. In addition, they have been found to be as effective in improving the outcomes among poor and minority populations as in the general population. Some populations may lack the knowledge and skills to use the health care system appropriately and to live a healthy lifestyle. Low ‘health literacy’, as this phenomenon has been recently been labelled, may lead to health problems and to an inadequate use of health services. Undocumented persons and refugees are often insufficiently aware of their (limited) rights to health care, and as such may not seek medical attention for their health problems. In many Member States, it has been noted that ethnic minorities are very poorly informed on the functioning and possible benefits of mental health care services. It is known that ethnic minorities are often poorly reached by health education and promotion programs. Culturally sensitive health/patient education programs are needed to give ethnic minority patients more control over actions and decisions that influence their health. Of special importance are programs that inform patients on how to access and use the health care system in an effective way. Health education material, health promotion campaigns and interventions have to be tailored to the needs and characteristics of ethnic minorities: it may be necessary to translate material, provide audio- or video taped material for (semi)illiterate groups and groups with low educational status, take into account cultural issues (e.g. the use of certain pictures or drawings that may be considered acceptable in one culture and extremely offensive in another). Research makes clear that it is important to involve members of the target groups in the preparation and implementation of health promotion initiatives for ethnic minorities. These can often provide invaluable information on strategies and self-organisations that can help to improve the impact of health promotion activities. At a systemic level, the quality of care could be improved through the active participation of ethnic minorities in needs assessment, program development, implementation and evaluation. 7. Interventions to reduce health care disparities in multicultural society Apart from the strategies recommended so far, some evidence exists that a number of other strategies and interventions may be effective to improve the quality of health care services delivered in multicultural societies. There is some but no conclusive evidence that ethnic concordance between health care providers and patients may be associated with greater patient participation in care 17 processes, higher patient satisfaction, and greater adherence to treatment (Cooper-Patrick et al, 1999; Kaplan & Greenfield, 2004). Ethnic minorities are in many Member States underrepresented among health professionals. To increase the likelihood of ethnic concordance of patients and providers, the ethnic diversity of health care teams should be increased. To reach this goal, it is important to ensure that ethnic minority children get the chance to be trained as health professionals or social workers, and get equitable access to the labour market. In addition, many trained health professionals, especially physicians and nurses, who graduated outside the country they are residing in, often face major barriers to exercise their profession in the Member States. This is, of course, detrimental to the development of ethnically diverse health care teams. A lot of research has made clear that multidisciplinary team approaches (utilizing physicians, nurses, dieticians, and – particularly – social workers may be effective to reduce ethnic health care disparities. Smedley, Stith & Nelson (2003) argue that “multidisciplinary teams coordinate and streamline care, enhance patient adherence through follow-up techniques, and address the multiple behavioural and social risks that patients face, particularly racial and ethnic minority patients”. In a number of countries, e.g. Romania (Oana, 2003), Belgium (Verrept & Louckx, 1997), the USA (Jackson, 1999), the Netherlands (van Mechelen, 2000), United Kingdom (Rocheron, Dickinson & Kahn, 1988), intercultural mediation programs have been developed and implemented in health and social services to improve access and quality of care for ethnic minorities.6 Although the tasks performed by intercultural mediators may vary between different projects and countries, they generally act as interpreters, are culture brokers (explaining the culture of the physician and the health care institution to the ethnic minority patient and explaining the culture of the ethnic minority patient to the health professional, Kaufert 1984), are involved in health education, serve as a liaisons between patients and health professionals, and may act as patient advocates. In general, intercultural mediators are themselves members of the ethnic minority groups that are the target groups of the program they are working for. There is some evidence that intercultural mediators are useful to resolve linguistic and cultural barriers and have an important and positive effect on the quality of care delivered to ethnic minority patients as assessed by health professionals and ethnic minority patients alike. They facilitate the exchange of correct and detailed information between health professionals and ethnic minority patients, respect for patients’ rights, identifying patients’ needs, the provision of culturally sensitive and responsive care, and may have very important and positive effects on patient satisfaction (Verrept & Louckx, 1997; 6 Many – often poorly defined – terms are being used to describe persons engaged in what in a number of Member States if often referred to as intercultural mediation, e.g. : ‘community health worker’, ‘lay health advisors’, ‘neighbourhood workers’ ,‘health aids’. They all have in common that they are community members who serve as connectors between health care consumers providers to promote health among groups that have traditionally lacked adequate access to care (Witmer et al., 1995). Some of them are mainly involved in health education, whereas others mainly assist ethnic minority patients and health professionals during health care encounters. 18 Rocheron, Dickinson & Kahn, 1988). It should be pointed out, however, that a few intercultural mediation programs have met with fierce resistance from ethnic minorities, as was the case with the Asian Mother and Baby Campaign in the UK in the eighties, and intercultural mediation programs among the Inuit in Canada (Rocheron, 1989; 0’Neil, 1989). Ethnic minorities complained in the UK that the program focussed narrowly on ‘cultural difficulties’, failed to take into account the social and political determinants of their health and ultimately blamed Asian mothers for the high perinatal rates. In the case of the Inuit in Canada, intercultural mediators were perceived to be ‘siding with the health professionals’ who belonged to the dominant majority. As such they were felt to further disempower the ethnic minority patient. Finally, despite encouraging results, further research is needed to assess the impact of intercultural mediation on the quality of care (especially at the level of outcome) and the development of professional standards of good practice in this domain. 8. Development of a knowledge base on the health of multicultural populations and the health care they receive Most – if not all - Member States lack the data needed to develop an adequate health policy for ethnic minorities. Insufficient data are available on the health status of ethnic minorities and its determinants, accessibility and utilisation of curative and preventive health care services, ethnic health care disparities (e.g. differences in outcome between different ethnic groups), problems experienced by ethnic minorities (e.g. need for interpreter services) and health care professionals, patient satisfaction among ethnic minorities, discriminatory practices etc. As a result, it is extremely difficult to design a health policy for ethnic minorities, and to assess the effects of interventions aimed at improving the health status of ethnic minorities and or the reduction of ethnic health care disparities. To improve the situation, standardized and systematic data collection on ethnic minorities’ health and health care issues is critically important. Data on the health of ethnic minorities should, in addition, be combined with data on their socio-economic status and other relevant data such as language proficiencies, socio-cultural background etc. Although the systematic collection of data on ethnic minorities (ethnic monitoring) remains extremely controversial in a number of Member States, it seems to be hard to do without if we want to address ethnic minorities’ health problems in an adequate way. Unfortunately, European history bears terrible testimony to the risks associated with every form of ethnic registration. Therefore, it is of the utmost importance that Member States develop strategies that prevent the abuse of a system of ethnic monitoring, avoid stigmatisation of ethnic minorities and guarantee their safety. The development of a standardized data collection system is hampered by a lack of clear concepts and adequate research strategies that can be used to describe and analyse ethnic health and health care disparities, and to disentangle associated factors. The Institute of 19 Medicine in the US argues that while the literature provides significant evidence of racial and ethnic disparities in care, the evidence base from which to better understand and eliminate the disparities in health remains less than clear. They add that several broad areas of research are needed to clarify how race and ethnicity are associated with disparities in the process, structure and outcomes of care. They state that research must provide a better understanding of the contribution of patient, provider, and institutional characteristics on the quality of care for minorities (Smedley, Stith & Nelson, 2003). The situation in the Member States generally compares unfavourably with that in the US and other ‘classical’ immigration countries such as Australia and Canada. Only one Member State, the United Kingdom, has developed strategies that can be used to document the health status, the accessibility and the use of health care services by ethnic minorities. The following problems have to be resolved to improve the situation: Defining ethnic minorities in research and administrative health data Unlike in a number of classical immigration countries where ethnic minorities are defined by so-called ‘races’ in official statistics, most Member States with immigration experience only distinguish between ‘natives’ and ‘foreigners’ (using citizenship as a criterion). Citizenship is ill-suited as a variable to represent ethnic diversity as immigrants and their children may acquire the nationality of the country they have moved to. As a result, health data generated from datasets that rely on the notion of citizenship – which might have been suitable to distinguish between different ethnic groups in the first decades of immigration, should be interpreted with caution at present time. To obtain more reliable data on the health of ethnic minorities, a number of authors have recommended to include variables such as ‘country of birth’ and ‘country of birth of both parents’ systematically in administrative health data sets (Razum & Zeeb, 1998; Verweij, 1995). In the UK and Holland, a question on ethnic self-identification has been used to identify members of ethnic minorities in data sets (Aspinall, 1997; Verweij, 1995). To do justice to the heterogeneity within ethnic groups, it is important that other relevant data (such as socio-economic status, citizenship, duration of residence in the country, mother tongue, self-assessed command of the official language of the host country) are also included in the data sets wherever possible. Inclusion and proportional representation of ethnic minorities in research Ethnic minorities are often systematically excluded and therefore underrepresented in study samples in clinical and health services research because of a number of reasons. First, for operational rather than scientific reasons, ethnic minorities may be excluded because of limited proficiency in the official language or lack of literacy. Second, it is often considered too bothersome to test research instruments, such as testing scales or questionnaires, for their cross-cultural validity. To prevent methodological problems, and because of a lack of skills to develop cross-culturally valid research tools, researchers 20 often decide to exclude ethnic minority members in such cases. Third, ethnic minorities often have second thoughts to participate in biomedical research projects such as biomedical trials for fear of discrimination and of being used as guinea pigs for experimental drugs or treatments which results in recruiting problems. To acquire knowledge about the efficiency and effectiveness of health care services and to gather information needed for the development of patient and demand oriented health services, patient surveys have been carried out in a number of Member States. Unfortunately, different studies show that ethnic minorities are not adequately represented in such surveys (Trojan, 1998; Borde, 2002) and that they do not benefit from improvements based on quality management (although they might need it most). As in classical (bio)medical research, semi- or completely illiterate patients with limited proficiency in the official languages are often not reached in patient surveys. Due to gender-related disadvantages, ethnic minority women tend to be more excluded than their male counterparts. As a result of the above described processes, study samples, and as a consequence, the results of a lot of research are biased and do not adequately represent the diversity of the present-day population of multicultural Member States. Under-representation or exclusion of ethnic minorities may make it impossible to generalize study results to the entire population. As a result, less is known about risk factors, disease prevalence, and response to treatment of specific ethnic groups. In addition, it has to be pointed out that researchers, who have only rarely been trained to conduct research in multicultural settings, will hardly ever be criticized for the exclusion or inadequate handling of issues of cultural diversity in their work. When ethnic minorities are included, the lack of cross-culturally valid research tools, may lead to an inadequate representation of their experience, e.g. when only diagnostic categories based on Western medical concepts are being used in health surveys. Finally, further research is needed to illuminate a whole series of issues related to the health of ethnic minorities: - - the determinants of ethnic health patterns; the determinants of problems of access for ethnic minorities; the determinants of health care disparities; assessing the effectiveness of intervention strategies (such as the creation of interpreter services, cultural competence training for health professionals, patient education programs, …) the development of adequate systems of ethnic monitoring and diversity management in health care services The questions raised above can only be answered using a multidisciplinary approach, combining epidemiological methods with quantitative and qualitative sociological and anthropological research methods. 21 References Ahmad WIU. (ed). Ethnicity, disability and chronic illness. Buckingham: Open University Press, 2000: 154. Andrews A, Jewson N. Ethnicity and infant deaths: the implications of recent statistical evidence for materialist explanations. Sociology of Health and Illness 1993; 15 (2): 137-156. Aspinall P. The conceptual basis of ethnic group terminology and classifications. Social Science and Medicine 1997; 45 (5): 689-698. Begemann F. Systematische misverstanden binnen een cultuur. Hoe beïnvloeden professionale concepten de interpretaties van cliënten? Medische Antropologie 1996; 8 (1): 44-54. Bhrolchain MN. The ethnicity question for the 1991 Census:background and issues. Ethnic and Racial Studies 1990; 13 (4): 542-567. Bischoff A. Caring for migrants and minority patients in European hospitals. A review of effective interventions. Study commissioned by the L.Boltzmann Institute for the Sociology of Health and Medicine, Vienna, 2003: 142. Borde Th. Patientinnenorientierung im Kontext der soziokulturellen Vielfalt im Krankenhaus. Vergleich der Erfahrungen und Wahrnemungen deutscher und türkischsprachiger Patientinnen sowie des Klinikpersonals zur Versorgungssituation in der Gynäkologie. Dissertation. Technische Universität Berlin, Fakultät VIII – Wirtschaft und Management. Http://edocs.tu-berlin.de/diss/2002/borde_theda.htm. Bowen S. Language barriers in access to health care. Canada (s.l.): Health Canada, 2001: 120. Bowler I. 'They're not the same as us': midwives' stereotypes of South Asian descent maternity patients. Sociology of Health and Illness 1993; 15 (2): 159-178. Bradby H. Ethnicity: not a black and white issue. A research note. Sociology of Health & Illness 1995; 17 (3): 405-417. 22 Brazinova A. Country report – Slovakia. (Report prepared for the Committee of Experts on Health Services in a Multicultural Society), 2003: 14. Cass A, Cunningham J, Snelling P et al. Renal transplantation for Indigenous Australians: indetifying barriers to equitable access. Ethnicity & Health 2003; 8 (2): 111-119. CBS. De gezonheidsenquête turkse ingezetenen in Nederland 1989/1990. Amsterdam: CBS, 1991:137. CEMG. Verslag: literatuursearch en opstarten van een intervisiegroep omtrent methodieken van transculturele hulpverlening en gezondheidsvoorlichting. Brussel: CEMG, 1997: 36 + bijlagen. Chin MH, Zhang XJ, Merrell K Diabetes in the African-American Medicare population: Morbidity, quality of care, an resource utilization. Diabetes Care 1998; 21 (7): 1090-1095. Cooper-Patrick L, Gallo JJ, Gonzalez et al. Race, gender, and partnership in the patient-physician relationship. Journal of the American Medical Association 1999; 282 (6): 583-589. Csitkovics M, Schmidl H. Country report – Austria. (Report prepared for the Committee of Experts on Health Services in a Multicultural Society), 2004: 16. David M, Borde Th. Kranksein in der Fremde? Türkische Migrantinnen im Krankenhaus. Frankfurt/Main: Mabuse Verlag 2001 Donovan J. Ethnicity and health: a research review. Social Science and Medicine 1984; 19: 663-670. Es Safi L. La médiation interculturelle en matière de santé: une réponse aux problèmes de communication entre patients migrants et personnel soignant ? Rapport de recherche. Liège: Résonances, 1996: 75 + annexes. EUMC (European Monitoring Centre on Racism and Xenofobia). Breaking the barriers – Romani women and access to public health care. Luxembourg: Office for Official Publications of the European Communities, 2003: V + 118. 23 German Federal Bureau of Statistics, 2000 cit. in Borde Th, Country Report – Germany (Report prepared for the Committee of Experts on Health Services in a Multicultural Society): 14. Guadadagnoli E, Ayanian JZ, Gibbons G et al. The influence of race on the use of surgical procedures for treatment of peripheral vascular disease of the lower extremities. Archives of Surgery 1995; 130: 381-387. Gushulak BD, MacPherson DW. Health issues associated with the smuggling and trafficking of migrants. Journal of immigrant health 2000; 2 (2): 67-78. Hawthorne K. Asian diabetics attending a British hospital clinic: a pilot study to evaluate their care. British Journal of General Practice 1990; 40: 243-247. Helman C. Culture, Health and Illness. London: Wright, 1990: 344. Henley A, Schott J. Culture, religion and patient-care in a multi-ethnic society. A handbook for professionals. London: Age Concern England, 1999: XVII + 602 Jacobs E, Agger-Gupta N, et al. Language barriers in health care settings. An annotated bibliography of the research literature. Woodland Hils (Ca, USA): The California Endowment, 2003: 72. Inequalities in health. The Black Report. London: Penguin Books, 1990. Kaufert J, Putsch R. Communication through interpreters in healthcare: ethical dilemmas arising from differences in class, culture, language, and power. The Journal of Clinical Ethics 1997; 8 (1): 71-87. Kaplan SH, Greenfield S. The patient’s role in reducing disparities. Ann. Internal Medicine 2004; 141: 222-223. Melikyan A. Country report: Armenia. (Report prepared for the Committee of Experts on Health Services in a Multicultural Society): 10 . Murray-Garcia JL. Multicultural Health 2002. An annotated bibliography. Woodland Hils (Ca, USA): The California Endowment, 2002: 85. 24 Kleber R. The begrip posttraumatische stress-stoornis in cross-cultureel perspectief. Mogelijkheden, beperkingen en bedenkingen. Medische Antropologie 1996; 8 (1): 27-43. Kleinman A, Good B (eds). Culture and depression. Berkeley, Ca: University of California Press, 1985: 535. Meurs P, Emde R. Cultuur-snsitieve ontwikkelingsbegeleiding. Preventief werken aan veerkracht in de vroege ouder-kind relatie bij kwetsbare gezinnen van allochtone afkomst. Medische Antropologie 2003; 15 (1): 157-182. Naish J., Brown J., Denton B. Intercultural consultations : investigation of factors that deter non-English speaking women from attending their general practitioners for cervical screening.British Medical Journal 1994;309:1126-1128. Oana SC. Country reports – Romania. (Report prepared for the Committee of Experts on Health Services in a Multicultural Society), 2003: 4. O'Neil JD. The cultural and political context of patient dissatisfaction in cross-cultural clinical encounters: a Canadian Inuit study. Medical Anthropology Quarterly Vol 3 (4), p. 325344, 1989. O'Neil J, Kaufert M, Koolage W. The role of native medical interpreters in diabetes education. Beta Release 1986; 10 (2): 11-14. Peeters R, De Muynck A. De zorg voor allochtonen. De aandacht voor Marokkanen en Turken in de Vlaamse Gezondheidszorg. Gezondheid. Theorie in praktijk 1994; 2 (2): 84-100. Rachvelishvili N. Country report – Georgia. (Report prepared for the Committee of Experts on Health Services in a Multicultural Society), 2003: 10. Razum O, Zeeb H. Epidemiologische Studien unter ausländischen Staatsbürgern in Deutschland: Notwendigkeit und Beschränkungen. Das Gesundheitswesen 1998; 60: 283-286. Rocheron Y, Dickinson R, Khan S. Evaluation of the Asian Mother and Baby Campaign. I. Assessment of the Linkwork Scheme. Leicester: Centre for Mass Communication Research University of Leicester, 1988: 414. 25 Rocheron Y. The Asian Mother and Baby Campaign: the construction of ethnic minorities health needs. Critical Social Policy 1988; 22: 4-23. Roderick P, Jones I, Raleight V, McGeown M, Mallick N. Population need for renal replacement in Thames regions: ethnic dimension. British Medical Journal 1994; 309: 1111-1114. Schulpen TWJ. Internationale en interculturele aspecten van kindergeneeskunde en jeugdgezondheidszorg. Nederlands Tijdschrift voor Geneeskunde 1994; 138 (7)-: 367370. Schulpen TWJ. Mortaliteitsverschillen tussen allochtone en autochtone kinderen in Nederland. Utrecht: Centre for Migration and Child Health, 1996: 105. Senior P, Bhopal R. Ethnicity as a variable in epidemiological research. British Medical Journal 1994; 309: 327-330 Smaje C. The ethnic patterning of health: new directions for theory and research. Sociology of Health and Illness 1996; 18 (2): 139-171. Smedley B, Stith A, Nelson A (eds).. Unequal treatment. Confronting racial and ethnic disparities in healthcare. Washington DC: The National Academis Press, 2003: XVI + 764. Sundquist J. Ethnicity, social class and health. A population-based study on the influence of social factors on self-reported illness in 223 Latin American refugees, 333 Finnish and 126 South European labour migrants and 841 Swedish controls. Social Science and Medicine 40 (6); 1995: 777-787. Tribe R, Raval H. Working with Interpreters in Mental Health. Hove and New York : Brunner-Routledge, 2002 : XIII + 270. Trojan A. Warum sollen Patienten gefragt werden? Zu legimitation, Nutzen und Grenzen patientzentrierter Evaluation von Gesundheitsleistungen (II): In: Ruprecht T (Hrsg.). Experten fragen – Patienten antworten. Patientzentrierte Qualitätsbewertungen von Gesundheitsleistungen – Konzepte, Methoden, praktische Beispiele. Sankt Augustin: Asgard-Verlag, 1998. 26 US Department of Health and Human Services (Health Resources and Services Administration). Cultural competence works. Using cultural competence to improve the quality of health care for diverse populations and add value to managed care arrangements. (document can be downloaded from the HRSA Center for Managed Care’s Website at www.hrsa.gov/cmc.) US DHHS (Department of Health and Human Services. Mental Health: Culture, Race and Ethnicity – A Supplement to Mental Health: A Report of the Surgeon General. MD: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for mental health Services. Van Dijk R. Cultuur als excuus voor een falende hulpverlening. Medische Antropologie 1989; 1 (2): 131-143. Van Mechelen P. Allochtone zorgconsulenten in de eerstelijnsgezondheidszorg. In: De intermediair als bruggenbouwer. Utrecht: FORUM, 2000: 25-46. Van Steenbergen J, Hoogenbeozem J, Van Driel H, et al. Analyse sterftecijfers CBS van 0-14-jarige kinderen, 1979-1993. In: Schulpen T (ed).: Mortaliteitsverschillen tussen allochtone en autochtone kinderen in Nederland. Utrecht: Centre for Migration and Child Health, 1996: 41-62. Verrept H. Evaluatie van het project 'interculturele bemiddelaars in de gezondheidszorg'. Eindrapport. Brussel: Medisch-Sociale Wetenschappen, VUB, 1995: 259. Verrept H, Louckx F. Health advocates in Belgian health care. In: Ugalde A, Cardenas G (Eds.). Health and Social Services among International Labor Migrants: a Comparative Perspective. Austin (Texas): CMAS-books, 1997: 67-86. Verrept H, Timmerman C. Gezondheidsonderzoek bij allochtonen. In: Vrancken J, Timmerman C, Van der Heyden K. Komende Generaties. Leuven: Acco, 2001: 213-224. Verweij AO. Een kwestie van organiseren. De invoering van een etnische registratie in arbeidsorganisaties in het kader van de wet bevordering evenredige arbeidsdeelname allochtonen en het EMO-beleid. Rotterdam: Instituut voor Sociologisch-economisch onderzoek, 1995: 80. 27 Whittle J, Coniglario J et al. Racial differences in the use of invasive cardiovascular procedures in the department of veterans’ affairs medical system. New England Journal of Medicine 1993; 329 (9): 621-627. Witmer A, Seifer SD, Finocchio L et al. Community health workers. Integral members of the health care work. American Journal of Public Health 1995; 85 (8): 1055-1058 28