Population
advertisement

Mindfulness-based Attention Training as an effective component in treating
Emotional Disorders: a comparison study
Short title:
Mindfulness-based Attention Training & Emotional Disorders:
a comparison study
F. Giommi1,5, H. Barendregt1, L. Oliemeulen2, J. van Hoof2, J. Tinge3, A. Coenen4,
P. van Dongen2
1
Faculty of Science, Mathematics and Computing Science,
Nijmegen University, Nijmegen, The Netherlands.
2
Institute for Mental Health, GGZ Oost Brabant, Oss, The Netherlands.
3
Tinge Training & Therapy.
4
Faculty of Social Sicences, Nijmegen University, Nijmegen, The Netherlands.
5
<fabiog@cs.kun.nl>.
Abstract
The clinical application of mindfulness, a concept coming from traditional Buddhist
insight meditation, has been recently studied. A clinical comparison study was
performed with a sample of 25 patients suffering from several DSM-IV diagnosed
Emotional Disorders assigned, in a matched randomised design, to the Mindfulnessbased Attention Training (MBAT) or to a concomitant treatment Psycho-education
(PE), a well-established standard intervention for psychiatric settings in the Netherlands. The study focussed on symptoms reduction, but also on general mental
functioning, as attention. The former was assessed, pre and post, by means of 5
standard clinical scales for depression and anxiety, and a quality of life assessment;
the latter, by 6 standard neuropsychological tests. In addition, EEG recordings were
taken. Results: a) comparing the two trainings MBAT resulted significantly more
effective than PE; b) also it resulted in significantly improving attentional performances of the patients, and c) their relaxation, as measured by EEG.
1. INTRODUCTION
The development of mindfulness has been a longstanding method used in traditional
Buddhism to decrease mental suffering. The Mindfulness-based Attention Training
used in this clinical and experimental study is based on this traditional concept.
Mindfulness is a mental act of attention in which one makes a reflexive nonjudgmental observation of the phenomena that are presented, thereby obtaining a
certain detachment. If, for example, one sees a desirable object, then the act of
mindfulness is not directed to that object, but to the mental state of 'desiring'. The
cultivation of mindfulness is the main purpose of the meditation training. This
consists, thus, in the effort to intentionally pay attention to present-moment
experience and sustain this attention over time; the aim is to develop a stable and
non-reactive present moment awareness. During the training the meditator makes a
1
conscious effort to apply mindfulness all the time. At a moment of clear 'insight' and
surrender, mindfulness 'takes over' and the person will have less disturbance factors.
This method has been applied to a psychiatric clinical setting by several
researchers: (Kabat-Zinn et al., 1992), (Teasdale et al., 1995) and (Schwartz et al.,
1997a), each in a slightly different way. We follow the method of (Kabat-Zinn, 1990)
who has introduced it as the 'Mindfulness-Based Stress Reduction' (MBSR) program,
a form of training based on mindfulness meditation. The training has been applied in
a variety of healthcare settings to a remarkably wide range of medical diagnoses.
Several studies have given evidence of major reductions of medical and
psychological symptoms. Evidences towards the effectiveness in this2 sense of the
program have been given for: chronic pain (Kabat-Zinn et al., 1986) and (Randolph
et al., 1999), psychosomatic disorders as psoriasis (Bernhard, 1988) and Kabat-Zinn
et al., 1998b), breast and prostate cancer (Kabat-Zinn et al., 1998a). Previous studies
have also demonstrated that mindfulness-based programs are an effective component
in treating a broad spectrum of patients in several diagnostic categories of emotional
disorders. The effect of Mindfulness-based Attention Training has been studied in
anxiety disorders such as Generalised Anxiety Disorder (GAD) and Panic Disorder
(PAD) with and without agoraphobia (Kabat-Zinn et al., 1992) and (Miller et al.,
1995). More recently, Mindfulness-Based Cognitive Therapy (MBCT) has been
developed by (Segal et al., 1995), combining Kabat-Zinn’s method with some
techniques drawn from Cognitive Therapy (CT). It has led to conceptual advances in
the modelling of affective change in mood disorder (Teasdale et al., 1997) and it has
proven to be particularly effective in the prevention of depressive relapse (Teasdale
et al. 2000). The same research group also showed that the MBCT was able to
modify a specific memory bias of depressed patients (Williams et al. 2000).
Moreover, the hypothesis is that there are many other possible applications of
Mindfulness-based Attention Training to clinical psychology. For example, Teasdale
and colleagues have applied a form of mindfulness-based program with recovered
depressed patients, obtaining quite promising results.
Besides that—to our knowledge—no studies have been performed to
compare the effectiveness of Mindfulness-based Attention Training with other
treatments well established in psychiatric settings. Also, no study has included
neuropsychological measurements in order to investigate the functioning of
attentional mental processes supposed to be particularly involved in the application
of Mindfulness-based Attention Training.
The present study deals with these two points. A sample has been selected
consisting of 25 patients suffering emotional disturbances comprising Anxiety
Disorders and Mood Disorders. All participants had a DSM-IV diagnosis and several
hospitalised patients were included. The patients have then been divided into two
groups, an experimental group (n=14) receiving the Attention training and a
comparison group (n=11) receiving another treatment, Psycho-education. The latter is
a standard psychosocial intervention for both hospitalised and out-patient psychiatric
populations in The Netherlands (see 2.1). During the experiment all patients
continued receiving the usual clinical treatment. In two sessions, before and after the
2
treatments, patients of both groups underwent the following four sets of
measurements: clinical psychiatric rating scales, neuropsychological tests related to
attentional and psychomotor processes, neurophysiologic monitoring (EEG), and a
quality of life assessment. Qualitative data concerning health perception and effects
of therapy were also collected.
The general aims of this pilot study are the following. (a) To assess the
efficacy of treating patients diagnosed with Anxiety Disorders and Mood Disorders
by means of Mindfulness-based Attention Training. (b) To investigate whether
beneficial effects of the training are correlated with the improvement of attentional
and psychomotor mental processes. (c) To find more evidence for the claimed
characteristic wide-range effects of treatments based on developing mindfulness.
The Mindfulness-based Attention Training is a highly structured program in
mindfulness meditation and its application developed by Kabat-Zinn and others. It is
an 8-week long course in which the participants attend a weekly 2.5-hour group
session. In the group sessions the participants are guided through the program,
motivated, inspired and supported by a MBSR experienced trainer (J.T.). The
training includes 1 h. homework of formal and informal exercises, 6 days a week,
supported by workbook and tapes. The training has formal and informal exercises.
Formal exercises are structured ones and are used to learn the practice of attention
training supported by guided exercises on tapes. The main formal exercises used in
the training are: a) body scan, a gradual attentive sweeping through the body from
feet to head, focusing on proprioception with regular suggestions of awareness of
breath and relaxation, usually done laying down. b) Simple stretch- and hatha yoga
exercises, as a way of practising attention-mindfulness on the body and mental
concomitants during movement. c) Attention-mindfulness to the breath, thoughts,
feelings and other mental and physical objects as they arise in the field of perception,
usually done sitting. Informal exercises are meant to practice mindfulness and to
integrate the practise into the participants’daily life. The training program has been
described in detail in (Kabat-Zinn, 1990). Post-interviews of 1 hour per person have
been taken. In this interview the participant can reflect on his/her practice and the
effects of the training. Experiences of the participant can be clarified if necessary.
The meeting with the participants in the post-interview provided the qualitative data
of the training.
The specific questions we intended to answer in the present study are the
following. 1. Is there some evidence that Mindfulness-based Attention Training is
able: (a) to favour clinical symptoms improvements in emotional disorders patients;
(b) to improve attentional and psychomotor performances on standard
neuropsychological tests, in comparison with a well-established treatment for
psychiatric settings, as Psycho-education? 2. Are the data from EEG pre-post
treatment changes comparable to those from previous research on meditation in nonclinical populations?
2. METHOD
2.1 Participants and design. Sample. At the onset the study included 33 psychiatric patients
suffering from emotional disorders: anxiety disorders and mood disorders. All patients were
recruited in the Institute for Mental Health Care GGZ, Oost-Brabant, the Netherlands, and
3
had a DSM-IV diagnosis. They were hospitalised during the period of the research or within
five years before. All patients were receiving standard pharmacological treatments and they
had no severe neurological or physical illness that could influence the tasks. Prior to
participating in the study patients gave their informed consent. Exclusion criteria for
entering the group were any psychotic state as related to a diagnosis of Schizophrenia or to
another Psychotic Disturbances and to Mania (DSM-IV Bipolar Disturbance I). None of the
subjects showed any signs of alcohol or drug abuse at the time of testing.
Design. The study has been conducted following a matched randomised betweenwithin design. Due to Dutch law and the recommendations of the Regional Ethical
Committee it was mandatory, in this clinical setting, to give to any control group also extra
treatment, besides the usual (medication) therapy. As concomitant treatment it was decided
to offer Psycho-education to the control group during the same 8 weeks. Psycho-education is
a standard psychosocial intervention for both hospitalised and out-patient psychiatric
populations in The Netherlands. As Mindfulness-based training, it is a group-format
training. Moreover, research has showed its efficacy in reducing symptoms in emotional
disorders (Rush, 1999), (Cuijpers, 1998,1996), (White, 1998) and (Parikh S. et al., 1997). It
consisted of 8 weekly group meetings of 2.5 hour. In each session a psychiatrist (T.V. B.)
explained patients about diagnosis and treatments of symptoms, facilitating the group
discussion about personal experiences, improving the patients’ knowledge, awareness and
understanding, and teaching how to improve their managing-capability of the symptoms and
disturbances.
Assignment. The participants were randomly assigned to the experimental group and
to the comparison group after the first measurements had been performed. First, the patients
names were coded with numbers. Then a number was extracted randomly, and the data
related to such number has been paired with another patient's number. Each pair was
matched on the following variables: Sex, Age, Education, Hamilton Depression Scale score,
and Continuous Performance Test score. Of this group of participants seven patients did not
undergo the post-treatment set of measurements because of various reasons. Moreover, one
patient diagnosed as Unipolar Major Depressive resulted to be in remission at the time of
first set of measurements and his data has been removed. Thus, the analysed data are derived
from a sample of 25 patients who met inclusion criteria and attended both the pre and post
sessions of measurements. These participants were both in-patients (N=14) and out-patients
(N=11). Of these 25 patients included in the study 19 (76%) received a diagnosis of Mood
Disorder, and 6 (24%) patients were diagnosed as suffering an Anxiety Disorder. None of
the bipolar patients included within the group who received a diagnosis of Mood Disorder
were in the manic state at the time of the experiment.
The average age of the sample was 41.00 (SD 11.42), with a minimum of 22 and
maximum of 69. The group consisted of 5 males and 20 females. The median of educational
level was 4 (in a 1-7 scale), corresponding to the secondary education level. Of these 25
patients included in the data analysis, 14 were in the experimental group (Attention
Training-MBRS) and 11 in the comparison group (Psycho-education).
In the Attention Training-MBSR group, 10 subjects had a diagnosis of Mood Disorder (4
Unipolar Major Depressive Disorder, 3 Distimic Disorder, 3 Bipolar Disorder) and 4 a
diagnosis of Anxiety Disorders (1 Anxiety Disorder NAO, 1 Post Traumatic Stress Disorder,
2 Panic Disorder with Agoraphobia). In the Psycho-education group, 9 subjects had a
diagnosis of Mood Disorder (7 Unipolar Major Depression, 2 Distimic Disorder) and 2 a
diagnosis of Anxiety Disorder (1 Anxiety Disorder NAO, 1 Panic Disorder without
Agoraphobia).
To check the efficacy of the random assignment procedure, experimental and
control groups were compared by one-way ANOVAs computed for the matched variables.
No significant difference between the groups was found: Sex [(F(.613), p=.442), Age
4
[F(.051), p=.823], Education [F(.551), p=.466], Hamilton Depression Scale [F(.555),
p=.464] Continuous Performance Test [F(.047) p=.831].
2.2 Measurements. Thirteen variables divided in three classes have been measured in this
study: five variables were derived from clinical-symptoms rating scales, two variables were
related to a quality of life assessment, and six variables were coming from (five) different
neuropsychological tests. The variables are introduced as C1, …, C5, Q1,Q2, N1, …, N6.
Moreover EEG measurements have been taken.
Clinical variables. To assess the effects of the treatments on the clinical symptoms,
five standard rating scales have been administrated in two sessions, before and after the
treatment. These scales were Hamilton for Depression and Hamilton for Anxiety, Zung SelfRating Scale for Depression, Visual Analogue Scale for Depression and Visual Analogue
Scale for Anxiety.
C1. The Hamilton Depression (Hamilton Rating Scale for Depression (Hamilton,
1960); (Williams, 1988) is a rating scale (17-items version; total score range: min. 0 - max.
52) administered by a clinician-interviewer for measuring the severity of depression, widely
used in clinical trials, having reliability coefficients ranging between 0.84-0.90. In the
present study it was scored by a psychiatrist (M.R.).
C2. The Hamilton Anxiety (Hamilton Rating Scale for Anxiety (Hamilton, 1959) is
an interviewer administered rating scale (14-items version; total score range: min.0 - max.
56) for measuring severity of anxiety disorders symptoms. Hamilton has a reported an interrater reliability of 0.90. In the present study it was delivered by a psychiatrist (M.R.).
C3.The Zung Depression (Zung Self-Rating Depression Scale (Zung, 1965) is a selfadministered rating scale (20 items; total score range: min. 20 – max. 80.) by which the
patients rate their agreement with the presented statements. Items are based on those clinical
diagnostic criteria most commonly used to characterise depressive disorders. In this study it
was done with the assistance of a psychiatrist (M.R.).
C4, C5.The Visual Analogue Scales (VAS) for Depression and for Anxiety are two
very simple analogue indicators for anxiety and depression (Zealley et al., 1969). The VASs
are self-rating scales, the rater is asked to locate each of the variables in question by marking
a point along a 10 cm line which runs between two extremes, representing 0 to 100 intensity.
High inter-rater reliability can be obtained (Lader and Marks, 1971). In this study they have
been scored in presence of a clinician (M.R.).
Quality of life assessment. To assess change in the quality of life perception, two
variables derived from the extended Dutch version of the Lancashire Quality of Life Profile
(LQLP) (Schene & Nieuwenhuizen, 1990) and (Nieuwenhuizen, 1998) were used. It is a
questionnaire consisting of 156 items, covering eleven different topics (named 'domains')
related to various aspects of life. These domains are: 1) living situation, 2) leisure & social
participation, 3) health, 4) finances, 5) family relations, 6) safety, 7) negative affect (affect
should be regarded here as equivalent to mood, for example: “In the last month did you ever
had the feeling that everything is going easy?”), 8) positive self-esteem (“Do you have the
feeling that you have some good qualities?”), 9) negative self-esteem (“Sometime you feel
completely worthless"), 10) life regard index of framework (the degree to which an
individual can envision his/her life as having some meaningful perspective), 11) life regard
index of fulfilment (the degree to which an individual has derived a set of life-goals from the
framework). The first six domains are rated according to 1-7 point satisfaction scale and
refer to the perception of the different socio-economic aspects of life. The last five domains
are rated according to a 1-3 point scale (“yes”, “no” or “don’t know”) and refer to the
perception of the 'self-related' aspects of life. The psychometric properties of the extended
Dutch version of the LQLP (Lancashire Quality of Life Profile) have been found sound and
in agreement with those contained in (Olivier et al., 1997) which reports reliabilities mainly
5
in the .60-.80 range (Nieuwenhuizen, 1998). As for the reliability of the 11 domains of the
extended Dutch version, in term of Cronbach’s alpha, it is 'sufficient' (.70< alpha) for 8
domains. The reliability of 3 domains (safety, family relations, negative affect) needed
further investigation being in the range of .60<alpha<.70. For validity, evidence in support
of the content validity was obtained from the construction process of the instrument, and in
support of construct validity from the correlation pattern with related concepts measured by
others scales. As to content validity, results of a second order factor analysis showed that,
within the 11 quality of life domains, there are 2 distinct dimensions. An 'internal' dimension
related with the attitude of individuals towards themselves and to their sense that life has
meaning and purpose, and a second dimension which regards the more 'external' features of
quality of life. The first 'internal' dimension comprises the following five domains: positive
and negative self-esteem, negative affect, framework and fulfilment, for details see
(Nieuwenhuizen, 1998).
For the purpose of this study, we were interested in assessing whether the 'internal'
and the 'external' dimensions could be differently affected by the Mindfulness-based
Attention Training. For such reason we measured two different variables: one incorporating
the six 'external' domains and the other incorporating the five 'internal' domains. Because all
the five domains are rated with a 3-point scale, the variable expressing the mean of the
scores of such five 'internal' domains is named LQLP_3 (Q2). Otherwise, the variable
incorporating the mean of the scores from the six 'external' domains is named LQLP_7 (Q1).
The questionnaire was rated by two clinical researchers (L.O., M.P.), who were
trained in its administration and interpretation.
Neuropsychological variables. To assess the effects of the treatment on the
attentional and 'executive' processes, a test battery was administrated. The battery consisted
of five experimental tasks: two attentional tasks and three psycho-motor or 'executive
function' tasks. From these five tasks six variables have been measured (one of the tasks
giving rise to two different ones).
Two standard neuropsychological attentional tests have been used: the Stroop Test
(Stroop, 1935), considered to measure selectivity of attention, and the Continuous
Performance Test (CPT), which has been one of the few tests originally designed to measure
sustained attention (Rosvold et al., 1956).
N1. Stroop test (Stroop Colour-Word Test) is considered to measure selectivity of
attention. The test includes three cards. On the first card there are ten rows with ten words in
each row. The words can be: yellow, green, blue, red. Subjects are asked to read the card in
reading order. On the second card there are ten rows with each 10 coloured blocks. The
colour again can be yellow, green, blue or red. Subjects have to name the colour in reading
order. The time needed to complete the task is recorded. On the third card there are again ten
rows with ten words in each row. However this time the words are printed in different ink
colours. The instruction is to name the colour that sometimes is not matching the meaning of
the word. Because the reading automatic process is dominant, intentional effort is requested
to neglect the meaning of word in favour of colour perception. The time needed for the
second card is subtracted from the time needed for the third card and the result in named
'interference' score. In the present study this score is the computed variable. Time has been
measured with a chronometer. When selectivity of attention decreases the difference in time
needed will increase, therefore decreased scores mean improvement.
N2. CPT (Continuous Performance Test) is considered to measures sustained
attention, it is an experimental task that involves a rapid identification of a target and
withholding response to distracting stimuli. The correct-positive (hit) and incorrect-positive
(false alarm) are registered. In this study the task has been programmed on a microcomputer
according with the specifications drawn up (Nuechterlein et al., 1986). In this test a digit is
displayed each second, for 40 milliseconds, in the middle of a monitor. The background is
6
paperblack and the digit white. After a stimulus is projected, a black screen is projected over
the stimulus, which causes the presentation time to be very accurate. The size of the digit is
20 x 15 mm. the distance to the screen is about 60 to 70 cm, the projection to the fovea is 2
degrees. The subjects are asked to push a mouse with a finger each time a '3' is directly
followed by a '7'. 600 Digits are presented within 10 minutes and 90 '3-7' target sequences
are presented in a quasi-random series. Correct-positive and incorrect-negative reactions are
registered. The actual test is preceded by practice trials. The correct comprehension of the
instruction is checked. Sensitivity (d') is an index for discrimination between target and nontarget stimuli. We particularly focused on this index of overall signal/noise discrimination
level from signal-detection-theory (McNicol, 1972), (Davies et al., 1982) and (Nuechterlein
et al., 1988), which is closely related to the level of attentional arousal. The perceptual
sensitivity (d') is the calculated outcome variable in this study. Higher scores mean better
performances.
Three standard neuropsychological tasks related to psycho-motor functioning were
used: Trail-making Test B (N3), Wisc-Mazes (N4), and Test Digit Symbol SubstitutionTask
form which two different variables (N5, N6) have been measured). The term 'psychomotor'
is used to characterise the variety of actions involving both cognitive and sensorimotor
processes.
In performing all these tasks, a relatively new experimental apparatus has been used in order
to take more precise measures.
Apparatus. The Digit Symbol Substitution Test, the Trail-making Test and the
Mazes Test were all been administered on a digitising tablet allowing the precise recording
of the pen movements made during the tests. This technique (Teulings and Maarse, 1984)
had been used in the study of writing and drawing (Thomassen and van Galen, 1992) but has
only recently been applied in psychiatry (van Hoof et al., 1993, 1988), (Hulstijn, 1996) and
(Sabbe et al., 1996a,b, 1997). The three test forms were placed on a Wacom 1218 RE
digitising tablet. This apparatus, in combination with a special pressure-sensitive ball-point
pen, allows the registration of the X and Y co-ordinates of the pen tip when in contact with
the digitizer as well as up to 5 mm. above the writing surface. The position of the pen and
the axial force exerted on the tip of the pen were sampled with a frequency of 200 Hz and a
spatial accuracy of 0.2 mm. See (Teuling and Maarse, 1984) for details. By means of an
interactive computer programme and on the basis of pen pressure, the movements were
defined as either pen-up periods or pen-down periods (pressure threshold: 24 gr.).
Furthermore, pen-down periods during which the movement velocity remained below 0,57
cm/sec. were defined as pause intervals, whereas the remaining pen-down periods were
defined as movement time.
N3. Trail Making Test B is one of the tests from Halstead-Reitan Battery (HRB)
(Reitan & Davison, 1974), widely employed to test visual-motor ability, specifically:
flexibility of attention, set-switching and visuomotor speed. The subject first connects 25
numbered circles in sequential order drawing a line as fast and accurate as possible (TrailMaking A). The digits are scattered over a piece of paper. Then (s)he connects 25 letters and
numbered circles, in a sequence alternating between numbered and alphabetical circles
(Trail-Making B). A short practice before each test is provided. The Trail Making test B is
related to the ability to flexibly switch between different search criteria: the-next-digit and
the-next-letter. Working memory is involved in the task execution because while the next
stimulus is being searched, the last has to be memorised. By means of the digitizer tablet the
following measurements have been calculated: time to complete the task or 'end-time' (ET)
containing 'moving-time' (MT), 'stop-time' (ST) and 'jump-time' (JT); then 'velocity' (V) and
'pen pressure' (P). For the purpose of this study for each participant only the 'end-time' (N3)
on the Trail-Making B has been used as experimental variable. The lower the score the
better the performance.
7
N4. WISC-Maze Test is a part of the Adult Intelligence Scale (Wechsler, 1981),
Dutch version (de Bruyn et al., 1986). It is a task considered to measure psychomotor and
planning processes. Seven mazes were selected from the WISC Mazes. The instruction is to
draw an uninterrupted line from the person drawn in the centre of the maze to the exit. Lines
may not be crossed and the dead ends must not be entered. The time needed to complete the
maze is the experimental variable. The lower the time the better the performance (van der
Gaag, 1992, p.91).
N5, N6. DST (Digit Symbol Substitution Test) is one of the most frequently used
psycho-motor task and is a small subset of the Wechsler Adult Intelligence Scale. Subjects
are requested to substitute as fast as possible symbols for digits during 90 seconds,
according to a key consisting of nine symbol-digit pairs given at the top of the form. The
standard measure of this performance is the raw score (N5), i.e. the number of correct
responses. In the English version, symbols have to be filled in instead of digits. We used the
Dutch revised version in which numbers have to be filled instead of symbols. It has the
advantage that it elicits the more familiar response of number writing. The DST owes its
clinical sensitivity to the fact that it makes demands on several processes, i.e. perception,
selective attention, sustained attention, working memory, and visuomotor co-ordination. All
these processes need to function properly for a successful completion of the task (Lezak,
1983). Nonetheless, the DST has the disadvantage that it gives only one score, which make
it impossible to identify the contributions of the different processes. In order to obtain a
differentiation between the motor component of the task (i.e. visuomotor coordination) and
the cognitive components (i.e. perception, sustained attention, working memory), in the
present study the standard format used for DST was administered on a digitising tablet. This
technique allows a differentiation between 'writing time' i.e. the time taken to write a symbol
and what is often called 'matching time' (N6), i.e. the intervals between the writing of the
successive symbols, which is the time needed to find the correct symbol, or the time to
'match' the current digit with the proper symbol. The first is a measure of the psychomotor
component, the latter of the cognitive component (van Hoof et al., 1997), JogemsKosterman et al. 2000). This separation is based on the assumption that the writing of a digit
is a somewhat automatic process, thus the time the pen is moving on the tablet is considered
to represent motor activities such as visuomotor coordination. Otherwise, the intervals
during which the subject pauses above and on the writing tablet between two successive
digits are assumed to incorporate higher processes such as attentional ones and working
memory. Because this study is focused on attentional performances, the two computed
variables were: 1) raw score (N5), i.e. the number of correct digits produced within 90s;
higher scores indicate better performance; 2) matching time (N6) operationalized as the
accumulated pen-up periods of time between two successive digits, together with the pause
interval at the beginning and at the end of these digits; lower scores indicate improvement.
EEG measurements. The EEG of 21 patients (16 with Mood Disorders and 5 with
Anxiety Disorders) was recorded before and after the two treatments. Electrodes placed
according to the International 10-20 system on eleven locations (F3, F4, C3, C4, P3, T3, T4,
P4, Fz, Cz, Pz) while the right mastoid was used as reference. During recording the patients
were quietly laying on a medical bed in a room isolated from the recording equipment. After
placing the electrodes, a rest period of 15 minutes was taken into account. Then the EEG
was recorded during 5 minutes when the eyes were open and subsequently when the eyes
were closed.
2.3 Procedure. Two cycles of the program have been completed: the first during the period
October to December 1998 including 14 patients, the second during April to June 1999
including 19 patients. All the participants who attended the first cycle of the program were
in-patients, while in the second cycle 3 were in-patients and 16 out-patients. The program
8
has been given in a large and quite room in the same hospital where all the patients received
their metal health care. At the beginning of each of the two cycles, patients who met the
diagnostic criteria and agreed to join the experiment were informed that they would be
assigned randomly to one of the two groups after the first common session of measurements.
After their agreement they were asked to make four different appointments to complete the
first session of measurements. For each of the participants four individual appointments
have been arranged within the span of the week preceding the first week of administration of
the treatments. a) One of the appointments was for completing the clinical ratings scales,
which were performed or assisted by a psychiatrist. b) One was set to perform
neuropsychological tests and the Lanchashire Quality of Life Profile questionnaire. To
avoid, as much as possible, the experimenter effect the assessments and the tests were
administered by two trained clinical researchers, who were not involved in the design of the
research or in the interpretation of the data. For the same reason the MBSR-program
experienced trainer (J.T.) was also not involved in such activities.
While performing the writing and drawing tasks as well as the attentional tasks, the subjects
were seated in a quiet room. c) Another appointment was both with the trainer of the MBSR
and with the trainer of the Psycho-education program. d) Finally the EEG measurements
have been made.
The sequence of these variable measurements was randomly alternated for different
subgroups of patients. The same procedure has been followed at the end of the program,
with the set of measurements completed within two weeks from the end of the last week of
administration of the training. To minimise bias in data collection related to expectancy of
change, calculation of the neuropsychological tasks was done after all data were collected.
3. RESULTS
3.1 Data. To summarise, thirteen output variables and EEG alpha-power have been
determined in this study. Five variables measured clinical symptomatology:
C1=Hamilton Depression, C2=Hamilton Anxiety, C3=Zung Depression, C4=VAS
(Visual Analog Scale) Depression and C5=VAS Anxiety. Two of them derived from
the Lancashire Quality of Life Profile (LQLP) questionnaire: Q1=LQLP_7 and
Q2=LQLP_3. Six other variables, calculated from five different neuropsychological
tests, were related to attentional processes. These were named: N1=Stroop Test,
N2=CPT-d' (Continuous Performance Test perceptual sensitivity d'), N3=TrailMaking B, N4=WISC-Maze, N5=DST (Digit Symbol substitution Test) Raw-score,
and N6=DST Matching-time.
Four variables: N1=Stroop Test, N3=Trail-Making, N4=WISC-Maze and
N6=DST Matching-Time were checked as being not normally distributed and have
been normalised applying a natural-logarithmic transformation, indicated in the text
with (Ln).
For various accidental reasons it was not always possible to obtain a complete
data set for each of the patients included in the study on all the 13 pre and post
measurements. A completed data set was obtained for 17 subjects. Two patients
missed their post appointments for completing the clinical ratings scales because
were involved at the same time in other hospital activities, another patient resulted
later as having misunderstood the instructions about the two VAS self-rating scales
during his pre-training session. Technical problems with the digitising tablet
apparatus arised during the recording of the pre-training measurements of N3 for one
subject and of N5 and N6 for another subject; for the same reason the data from N3,
9
N5and N6 of one other subject in the post session were not avaiable. The posttraining Q2 assessment of the of one patient was unfortunaly lost, and the C4, C5, N5
and N6 post training records of one other subject were deteriorated because of an
accident occured to his file.
First we decided to perform a standard missing analysis procedure, and the
subsequent statistical analysis were run on a data matrix filled with estimations of
missing data. Later, however, we realized that this procedure did destroy part of the
correlation structure between the different variables, and therefore did alter the
multivariate nature of the effects of the trainings. We therefore decided to perform a
new analysis on the raw data. We have not taken any attitude with respect to the
missing data, except that the fact of missing is supposed not to be related to the value
that would have been measured. This means that we consider that a missing datum is
not related, in any way, to the value that would have been measured, nor to the other
measurements of the subject.
3.2 Analysis. Descriptive statistics and boxplots of the distributions of the
Mindfulness-based training and the comparison group variables (with data at the two
time points for the five clinical variables, the two variables related to the quality of
life assessment, and the six neuropsychological variables) are shown (listwise) in
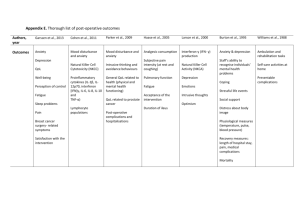
Table 1, in Fig. A and in Fig. B.
The effect of the training is considered to be the difference of the measurements of
the 13 variables after the training minus those before the training. In order to compare
the effect of Mindfulness-based Attention Training with respect to the effect Psychoeducation, a Multivariate Analysis of Variance (MANOVA) was run, comparing the
intervention and the comparison group along the thirteen outcome variables (SPSS
10, GLM-Multivariate). The comparison indicated a significant difference in the
sample means [p =,007; Wilks’ Lambda =,006; F = 35,589; df = (13,3)]; Eta Squared
=, 994]. The Mindfulness-based Attention Training showed improvements with
respect to all the variables, while the effect of Psycho-education showed univocal
improvements for all the variables only in the two sets of variables related to
depression (C1, C3, C4) and to quality of life (Q1, Q2). Moreover, considering the
pre-post sample mean differences for each variable (listwise), the Mindfulness-based
Attention Training showed a larger improvement for three (C3, C4, C5)of the clinical
variables, and for five of the neuropsychological, attention-related variables
(N1,N2,N4,N5,N6). Therefore we interpreted the multivariate significant difference
in favour of the Mindfulness-based Attention Training. Univariate analyses
confirmed such interpretation (see below).
The significance of the effect of each of the two interventions was then
assessed by means of an extension of the MANOVA procedure, based on the
homoscedasticity assumption that is already implicit in the MANOVA procedure for
assessing the difference of effects between trainings1. The extension was needed
because the sample sizes for the two trainings were too small to make inference on
them separately. For both the treatments resulted (very) significant effects:
Mindfulness-based Attention Training [p =,0010; Hotelling’s T Squared = 8175,223;
F = 125,772, df = (13,3)]; Psycho-education [p =,0002; Hotelling’s T Squared =
22500,30; F = 346,158; df = (13,3)].
10
Considering the mean differences both treatments, therefore, seemed effective
in producing positive changes. However, the effect of Mindfulness-based Attention
Training resulted significantly better than the effect of Psycho-education.
Moreover, the 13 outcome variables can be conceptually separated in 4
different classes measuring different constructs: Depression (C1, C3, C4), Anxiety
(C2, C5), Quality of Life (Q1, Q2), Attentional-processes (N1,..,N6). To assess the
effect of the two trainings on the different classes of variables, the same extension of
the MANOVA analysis was performed on each of the different classes, for each of
the two training. The Mindfulness-based Attention Training resulted to have a
significant effect on Anxiety [p =,020; Hotelling’s T Squared = 10,226; F = 4,844; df
= (2,18)], a trend for significance on Depression [p =,052; Hotelling’s T Squared =
10,501; F = 3,132; df = (3,17)], and, notably, a significant effect on Attentionalprocesses [p =,036; Hotelling’s T Squared = 26,692; F = 3,213; df = (6,13)], which
might be all interpreted as improvements. Psycho-education had a significant
(positive) effect on Depression [p =,015; Hotelling’s T Squared = 15,483; F = 4,617;
df = (3,17)], a trend for significance on Quality of Life [p =,055; Hotelling’s T
Squared = 16,977; F = 3,330; df = (2,21) (p=,003)]; but, on the other hand, a
significant effect that can be interpreted as a worsening on Anxiety [p =,003;
Hotelling’s T Squared = 17,079; F = 8,090; df = (2,18)]. Such results might be
interpreted as evidence that the mindfulness training, while favouring positive
changes of symptomatology, is specifically effective in improving attentional
processes.
Univariate analyses were also performed in order to evaluate within–groups
changes. Paired t tests (pairwise) have been calculated on pre and post treatment
measurements of each outcome variable for the two treatments. Such.evaluation
indicates for Mindfulness-based Attention Training a sta-tistically significant
improvement for ten out of the thirteen variables; in the Psycho-education group, on
the other hand, only three variables showed a significant improvement;(see Tables
2a, 2b for descriptive statistics; and Tables 3a, 3b for Paired T Tests and Effect Size).
Hence, within-groups analysis as well indicates that both treatments seemed
able to produce improvements, Mindfulness-based Attention Training reaching more
frequently statistical significance, as showed in more details in the next paragraphs.
Clinical variables. Univariate analysis suggests that Mindfulness-based
Attention Training has been effective in reducing the level of psychological
symptoms. Four of the five clinical rating scales reached a significant pre-post mean
difference, respectively of: -4,25 (SD=4,99) (p<0,05) on the Hamilton Depression, of
–6,25 (SD=6,22) (p<0,01) on the Hamilton Anxiety, of –6,5 (SD= 9,56) (p<0,05) on
the Zung Depression, of –18,20 (SD=22,28) (p<0,05) on the VAS Depression; and a
trend for significance (p<0,1) on the fifth, VAS Anxiety: – 19,40 (SD=28,15)
(p=,056).
For the Hamilton Depression and Anxiety scales these represented mean
reductions of 23% and 34%, which were aligned to the reductions of 23% and 34%
for Hamilton Depression and Hamilton Anxiety, respectively, observed in previous
research on Mindflulness-based training with patients suffering of anxiety disorders
(Kabat-Zinn et al. 1992, 1995). The effect size of such mean reductions, as assessed
by Cohen’s d, resulted in a value of 0,85 and 1,00, respectively, which Cohen
11
described as indicating a large effect size2. The mean reductions for Zung
Depression, VAS Depression, and VAS Anxiety were of 11%, 24% and 30%, and the
related effect sizes values were of 0.67 (medium), 0,82 (large), 0,69 (medium). These
last three clinical scales had not been used in previous studies on Mindfulness-based
Attention Training.
The Psycho-education group showed statistical significant improvements for
two variables:
-5,72 (SD=4,54) (p<0,01) on the Hamilton Depression, and -5,0 (SD=4,94) (p<0,01)
on Hamilton Anxiety, with mean reductions respectively of 33% and 33% and large
effect size values: 1,25 and 1,00. Of the three other clinical variables that did not
reached statistic significance, Zung Depression showed a trend for significance with
mean reduction of 8%: 4,64 (SD=7,23) (p=,059). VAS Anxiety resulted in an
increase (worsening) of 24% .
Considering that Hamilton scales are rated by an external observer, while the
three others are self-rating scales, these findings could bring some evidence to the
hypothesis that, parallel to an improvement of clinical symptoms, Mindfulness-based
Attention Training is particularly effective in modifying the 'subjective' experience of
such symptoms, making the patients’ attitude toward the experience of them more
'detached'.
Quality of life profile. On the Lancashire Quality of Life Profile the Psychoeducation group variables improved but did not reached significance. As to the
Mindfulness-based Attention Training, LQLP_3 reached a significant pre-post
change of +0,14 (SD=,22) (p<0,05).This is the variable derived from the Lancashire
Profile section concerning the perceptions of the self-related or 'internal' aspects of
the quality of life (Negative Affect; Positive Self-esteem; Negative Self-esteem;
Goals Fulfilment) as distinguished from the perceptions related to the socioeconomic, 'external' aspects of life expressed in LQLP_7. Such outcome may be
interpreted as another data in favour of the hypothesis of a specific influence of the
Mindfulness-based Attention Training in modifying the 'subjective' perception of the
patients’ life experience.
Neuropsychological variables. In the Mindfulness-based Attention Training
group, five of the six neuropsychological variables reached a statistical significant
pre-post improvement: Stroop Test (p<,05), CPT-d' (p<,05), Trail-Making Test B
(p<,05), DST Raw-score (p<,05), DST Matching-time (p<,05). In the Psychoeducation group, otherwise, only one neuropsychological variables, CPT-d', had a
significant change (p<,05), as measured by Paired t tests (see Table 3a, 3b). Effect
size values are discussed in the context on the Section 4.
3.3 EEG. Analysis was focussed on the occurrence of alpha-rhythm. The alpha power
was calculated as the mean power of frequencies in range of 8 till 13 Hz. Data were
log transformed for statistical analysis. To determine the experimental effects
repeated measures ANOVA with pre-treatment – post treatment, condition (eyes
opened, eyes closed) and electrode placement as within subjects, and
treatment (attention training, psycho-education) as between subjects factor was
carried out.
A statistical significant increase in alpha power as a result of the treatments at
all electrode locations was found for the whole sample (both groups): F(1,19)=6,06;
12
p<,05 (see Fig. C). A wealth of evidence indicate that in adults the power in this
frequencies band is inversely related to cortical activation (Davidson, 1995). The
increase in alpha power is interpreted as an enhancement of the amount of relaxation
or a decrease in tension or stress (Coenen, 1995) due to the experimental treatments,
both as a result of attention training and psycho-education.
In this respect such result give evidence for both treatments to be regarded as
effective therapies. Though the alpha power was more increased in the patients
treated with Attention Training procedure, no statistically significant differences
could be established in this study between the two different treatments.
4. DISCUSSION
4.1 Attention and Emotional Disorders. It is now widely accepted that emotional
disorders are associated with a number of deficits in many cognitive processes, such
as in memory or in the 'executive' function, in which attentional processes are of
primary importance.
Memory-related cognitive processes have been shown impaired in depressed
clinical patients (Weingartner et al., 1981), (Cohen et al., 1982), (Wolfe et al., 1987)
and (Austin et al., 1992, 1999). For example, several studies evidenced in depressed
patients a stable tendency to overgeneral memory, which has been linked with
impaired problem-solving ability and slowed recovery (Williams, 1996) for a review.
Recently Segal, Williams and Teasdale developed Mindfulness-Based
Cognitive Therapy (MBCT) (Teasdale et al.1995) and Segal et al. in press), which
combine Kabat-Zinn’s mindfulness technique (MBSR) with others derived from
Cognitive Therapy (CT), as a treatment tailored to train depressed patients in skill
relevant to the prevention of depressive relapse. In the same context, Williams et al.
2000) showed that, although overgeneral memory may arise in depressives from
long-standing tendencies to encode and retrieve events generically, which tend to be
quite stable over time, such a style is nonetheless open to modification due to the
intervention with MBCT.
Impairment of the 'executive' function has been reported in depression
(Goodwin, 1997) for a review. As well, low-level attentional and selective processing
biases, that operate within the cognitive systems of anxious and depressed
individuals, favouring the processing of emotionally negative information, have been
demonstrated by a large number of studies (Mac Leod and Rutherford, 1998; for
review: Schatzberg et al. 2000) reported that patients with psychotic and nonpsychotic major depression showed impairment, at different degree, on a battery of
neuropsychological tests assessing attention, response inhibition and declarative
verbal memory; and both patient groups performed worse than healthy comparison
subjects.
To date no study has specifically investigated the effect of the Mindfulnessbased Attention Training on attentional processes, neither in normal subjects nor in
clinical populations. Assuming that a training based on mindfulness should affect
attentional processes, one of the aim of the present study is to support evidence in
favour of the hypothesis that low-level, automatic, attentional processes may also, as
showed in other studies for high-level memory processes, be modified by mean of the
mindfulness training.
13
4.2 Mindfulness-based Training and attentional processes. Although Stroop
Test and CPT are usually considered as 'attentional' tasks, whereas the others tests
used in the present study are regarded as 'psychomotor' tasks, it has to be emphasized
that all six of them involve attentional processes as one of their main component.
Between the psychomotor ones, Trail Making B is usually viewed as a task
measuring, among the rest, the flexibility of attention to switch between different
sets: working memory as well as selective attention are of importance here (van der
Gaag, 1992). Similarly, DST task is another standard psychomotor test which own its
clinical sensitivity to the fact that, for its successful completion, several different
processes need to function properly, i.e. working memory, sustained and selective
attention and visuomotor coordination (van Hoof et al., 1998).
Moreover, in this study the only variable that did not reached a significant
change in the Mindfulness Training group was the WISC MazeTest, which is related
to a task that is mainly a visuomotor one measuring the ability in planning, and for
which the attentional processes seem less relevant to the performance than in the
other tasks.
For many of the neuropsychological measures used in this study (N1,…,N6)
research data evidence neuropsychological deficits associated to many the DSM-IV
diagnoses included within the Emotional Disorders (see below).
Notably, the Mindfulness-based Attention Training group showed significant
changes on these neuropsychological measures, as assessed both by multivariate
analysis (see 3.1) and by univariate Paired t tests. The mean pre-post differences
correspond to effect size values (see below) that attained a medium magnitude for
five out of six of such variables (Table 2a, 2b).
N1. Stroop Color-Word tests the ability to screen out automatic verbal
responses that conflict with the required response. Thus selective attention, as
measured by Stroop, is the ability to focus on one source of information and to
actively inhibit automatic responses to information from other source. Heightened
distractibility by failing selective attention is the clinical counterpart. Performance on
the standard Stroop Colour-Word test have been showed impaired in major
depression patients (Lamelin S. et al., 1996, 1997). (Mc Neil, 1999) found that major
depressed and anxiety disorders (PTDS and OCD) patients, all showed response
slowing to the modified 'emotional' as well as to the standard Stroop. Anxiety has
been shown to effect Stroop performance in a vast body of literature (McLeod, 1991)
for a review. In this study, for the Mindfulness-based Attention Training group, the
pre-post improvement on the Stroop task consisted in a mean reduction in time
corresponding to medium effect size of d=0.64.
N2. There is evidence that CPT is impaired in depressed and patients. In (Hart
et al., 1998) it was found that depressed patients made more errors and that their
reaction times were slower than for normals. They found their pattern of findings
consistent with a failure of effort-demanding cognitive processes. (Nelson et al.,
1998) showed that CPT scores of patients with major depression with psychosis were
significantly worse than those of patients with major depression without psychosis
and normals. (Cornblatt et al., 1985a, 1985b) discovered that both depressed and
schizophrenic patients were characterised to the same extent by response decrements
due to external distraction while performing CPT: in normals the performances
14
improved under distracting conditions. Anxiety also seems to impair CPT
performance, (Cox, 1997) showed that children and adolescent with OCD anxiety
disorder had attentional and inhibitory deficits on CPT. From a cognitive perspective
CPT was designed as an energetical task, computations are kept simple and are
supposed not to affect performance, but sustain-ing attention over a long period of
time would result in performance decrement in patients with energetical failure. Yet,
Cornblatt found that performance did not drop below initial levels. So there is no
relevant time-on–task effect. Poor performance on the CPT must be attributed to
'computational' failure and not to energetical failure as was meant at the construction
of the task (van der Gaag, 1992). Similarly, (Neuchterlein et al., 1984, 1988) noted in
a study with schizophrenic patients, that their observed CPT deficit appears related to
ongoing selection of target stimuli rather than to deficient target selection specifically
at the end of a vigilance period. Accurate signal discrimination in the '3-7' version of
the CPT task presented here, requires substantial effortfull, capacity-demanding
processing. (Kahneman, 1973). The stimulus-input load are high and the conditions
of these task do not facilitate the development of automatic processing (Schneider et
al., 1977) and (Treisman et al., 1980). So it seems possible to see CPT as a task
sensitive to deficit in effortful, attentional, 'executive function' processing. For such
reason in this study the signal/noise discrimination indices (d') has been chosen as the
measured variable (N2). The Mindfulness-based Attention Training group had an
increase to an amount of d=0.59 (medium effect size).
N3. Trail Making has been used to assess the 'executive functions' in
emotional disorders patients. Veterans with PTSD anxiety disorder showed
impairment on the Trail Making Test B (Beckham, 1998) and (Curran et al., 1993)
found that elderly patients with depression had poorer than controls performance on
Trail Making. (Franke, 1993) found both depressed and schizophrenic patients
significantly worse than controls on Trail Making. For the Mindfulness-based
Attention Training group the pre-post change on the Trail Making B corresponded to
a medium effect size (d=0.62).
N5,N6. In several psychiatric disorders such as depression and schizophrenia
a slowing in motor and mental activities can be observed (White, 1997). DST has
been one of the tests often used to measure such psycho-motor slowing. The
performance on the DST has been found impaired in depression In a research
comparing endogenous and neurotic depressed patients, (Austin et al., 1992, 1999)
found that the performance on the DST was most impaired in the endogenous
patients. Data form subsequent research reconfirmed the result of a marked
psychomotor slowness in depressed patients (van Hoof et al., 1993) and (Sabbe et al.,
1996a, 1997). Using DST performed on the digitising tablet technique, (van Hoof et
al., 1998) showed that in depressed patients slowing involves both cognitive and
motor processes. In the present study the Mindfulness-based Attention Training
group outcome on the DST Raw-score corresponded to an improvement equivalent to
a medium effect size (d=0.67). It has to be noted that also the improvement on DST
Matching-time, which is specifically related to the cognitive and attentional
components of the task, consisted of a reduction in time corresponding to a medium
to large effect size (d=0.72).
Considered together, these findings of significant increases in several
neuropsychological performances, seem to bring some convincing evidence to the
15
hypothesis that the Mindfulness-based Attention Training is able to generate an
improvement in the low-level, automatic, attentional processes involved in the
neuropsychological tasks; as well as an improvement of the clinical symptomatology
of patients with emotional disorders.
Q1, Q2. As to regard to the Lancashire Quality of Life Profile, a comparison
of the 11 domains means with unpublished data of van Nieuwenhuizen 2000) showed
no relevant differences between the means of the two groups in this study with her
data for depressed and anxious patients. Indeed, the two research groups in general
showed lower scores on the domains, as predicted because of the fact that we
included hospitalised and acute depressed patients also. The pre-post increase for the
Mindfulness-based Attention Training resulted in a medium effect size (0.64) for the
LQLP_3 (Q2) variable (expressing the self-related aspects of quality of life).
4.2 Attention and depression. Teasdale and colleagues 2000) have recently applied
MBCT as a group-based psychological approach to preventing relapse and recurrence
in patients recovered, at the moment of the study, from Major Depression. They
showed that in patients with a history of three or more episodes of depression MBCT
approximately halved rates of relapse and recurrence over a one-year follow up
period compared with the patients who continued with the usual treatment. In the
theoretical background of MBCT it is assumed that vulnerability to relapse of
depression arises from repeated associations between depressed mood and a pattern
of negative, self-devaluative, hopeless thinking experienced during the depressive
episodes. It is suggested that in recovered depressed dysphoria may reactivates these
patterns of thinking. These can act to maintain and intensify the dysphoric state
escalating in self-perpetuating cycles of ruminative cognitive-affective processes,
that, in turn, increase the risk of further onsets of episodes of Major Depression. The
processes mediating relapse and recurrence appear to become progressively more
autonomous. The mindfulness-based training allow individuals from disengage from
habitual ('automatic') dysfunctional cognitive routines, in particular depressionrelated ruminative thoughts (Teasdale et al. 2000), p. 618. Their study, thus, seemed
to show evidences that the mindfulness-based training is able to produce positive
changes in the high-level cognitive and attentional routines, as the ruminative selfrelated thoughts, of depressed patients. Meditation practitioners were found to report
significantly fewer spontaneous, intrusive thoughts than non-clinical controls in a
working memory task (Fabbro et al., 1999).
Besides, Teasdale and colleagues deliberately chosen to exclude from their
study patients who were not largely recovered or remitted because it was assumed
that depression-related difficulties in concentration would interfere with the
application of the program, and thereby that such difficulties in concentration and the
intensity of negative thinking may preclude acquisition of the attentional control
skills, central to the training. The results of the present study, instead, seem to offer
some support the applicability of the mindfulness training also to non-recovered
Mood Disorders patients. Similar evidence come also from the qualitative data
collected during the present research, which will be presented in a later time.
One possible interpretation of our result could be found in recent data from a
study of Schatzberg and collegues (Schatzberg et al. 2000) on non-recovered
depressed patients, showing that patients with psychotic major depression had a
16
significantly greater impairment than patients with non-psychotic major depression
on a battery of neuropsychological tests assessing: attention, response inhibition and
declarative verbal memory. However, both depressed groups demonstrated
significant lower scores than did healthy subjects in a comparison group. But the
effect sizes of between-group differences in the test battery for non-psychotic patients
compared with comparison healthy subjects were generally below 0.40 (a mediumlow value). That is, non-psychotic depressed are not so far from normal subjects’
performance on attentional and control processes, at least the low-level ones, to
prevent the hypothesis that most of them could display enough concentration and
attentional control to implement the mindfulness training. Nontheless, from the same
data it seems plausible that depressed psychotic patients could not support such an
effort. Actually, with one possible exception, none of the depressive patients in the
present study sample was in a psychotic condition.
4.3 EEG findings. The result can be seen as giving evidence for both treatments to be
regarded as effective therapies in enhancing relaxation of the patients. Mindfulness
training showed a greater effect (but not to a statistically significant extent) than
Psycho-education on the induction of a decrease of cortical activity. The result of a
general significant increase in alpha power is consistent with previous findings from
research on meditation effects, which repeatedly indicated an increase of the alpha
power waves in non-clinical populations while practicing different form of
meditation. For reviews on the research on the psychophysiology of meditation see
(Jevning et al., 1992) and (Friedman et al., 1996). It is therefore of interest that a
form of meditation could attain a similar effect on a clinical population.
4.4 Limitations of this study. Although this study found promising results using a
well-controlled design, there are several limitations. Four main limitations need to be
discussed. 1. In order to obtain a sample sufficiently large for the adopted
experimental design, we decided to include patients suffering from different
emotional disorders, implying a mixed nature of our sample. In the treatment
literature it is usually accepted that it is meaningful to ask about the effectiveness of a
particular intervention in relation to a specific clinical disorder. The reason is that it
is unlikely that any one intervention is going to be equally effective for different
disorders, so that by mixing up different diagnoses it could be possible to conceal
effects of the intervention on one disorder in the lack of its effectiveness in other
disorders. Still, because we were interested in a better understanding of the peculiar
effectiveness of the mindfulness-based training as a “general purpose” treatment, as it
emerges from the research literature, this limitation might result in a useful way to
study such a wide range of applications of mindfulness. 2. The interpretation of
within-subject changes falls under the usual prudence needed with pre-post designs.
There could be other factors that have favoured these changes: the other treatments
that the patients were receiving, “spontaneous” improvement, the “practice effect” on
the assessments and the tasks. 3. It was not in the scope of this study to assess the
long-term effects of the intervention; thus it cannot be concluded that the short term
changes produced are enduring as the mindfulness practice is continued: this question
should be answered by future research.
17
On the other hand, the points of our experimental setting that improved
previous research consisted of the following. 1. The participants have been assigned
to the two treatments following a well-controlled matched randomised design. 2. The
trainer who administered the Mindfulness-based Attention Training, as well as the
clinical researchers who administered the assessments and the tests, were not
involved in the design or in the interpretation of data, in order to minimize the
experimenter effect. 3. It is the first time, in our knowledge, that a comparison study
is conducted in researching the effect of mindfulness-based intervention. 4. Another
positive aspect was that, using a comparison group a possible bias due to patients’
expectation was avoided in the mindfulness group.
5 CONCLUSION
5.1 Summary. The following main results derived from the present study.
(a) In order to compare the effects of Mindfulness-based Attention Training
with respect to the effects Psycho-education, a Multivariate Analysis of Variance
(MANOVA) was run, comparing the intervention and the comparison group along
the thirteen outcome variables (SPSS 10, GLM-Multivariate). Results indicated a
significant difference in the sample means in favour of Mindfulness-based Attention
Training [p =,007; Wilks’Lambda =,006; F (35,589); df = 13; Eta Squared =,994].
The significance of the effects of each of the two interventions was then
assessed by mean of an extension of the MANOVA procedure1. For both the
treatments resulted a (very) significant effects: Mindfulness-based Attention Training
[p =,0010; Hotelling’s T Squared = 8175,223; F = 125,772, df = (13,3)]; Psychoeducation [p =,0002; Hotelling’s T Squared = 22500,30; F = 346,158; df = (13,3)].
Summarizing: both treatments resulted in producing positive effects, and the
EEG results confirmed this interpretation. Moreover, the Mindfulness-based
Attention Training appeared significantly more effective compared to Psychoeducation (a skill-training group treatment for psychiatric settings well-established in
The Netherlands) in favouring patients’ improvement on several outcome variables.
Univariate analysis has also been performed in order to evaluate within–
groups changes. Paired t tests have been calculated on pre and post treatment
measurements of each outcome variable for the two treatments. Such evaluation
indicates for Mindfulness-based Attention Training a statistically significant
improvement for ten out of the thirteen variables; in the Psycho-education group, on
the other hand, only three variables showed a significant improvement. Therefore,
univariate within-groups analysis as well, indicates that both treatments seemed able
to produce improvements, Mindfulness-based Attention Training reaching more
frequently statistic significance.
(b) To assess the effect of the two trainings on the different classes of
variables (Depression, Anxiety, Quality of Life and Attentional-processes ) the
extended MANOVA analysis was performed on each class (listwise), for each of the
two trainings . Mindfulness-based Attention Training resulted to have a significant
effect on Anxiety (p =,020), and, notably, on Attentional-processes (p=,036), together
with a trend for significance on Depression (p=,052). Psycho-education had a
significant effect on Depression (p=, 015) and a trend for significance on Quality of
Life (p=,055), but, on the other hand, showed a significant (p=,003) worsening on
18
Anxiety. Such result might be interpreted as an evidence that the mindfulness
training, while favouring positive changes of clinical symptomatology, is specifically
effective in improving attentional processes.
Moreover, in the Mindfulness-based Attention Training group, five of the six
neuropsychological variables reached a statistical significant pre-post improvement,
as assessed by univariate Paired t tests. The mean pre-post differences corresponded
to effect size values that attained a medium magnitude for such five variables. In the
Psycho-education group, on the other hand, only one neuropsychological variable had
a significant pre-post change.
Taken together, these findings of significant increases in several
neuropsychological performances, seem to bring some convincing support to the
hypothesis that the Mindfulness-based Attention Training is able to generate an
improvement in the low-level, automatic, attentional processes involved in the
neuropsychological tasks.
In conclusion, the results of the present study seem to confirm previous
research and give some new evidences in favour of the effectiveness of Mindfulnessbased Attention Training in: a) reducing the clinical symptomatology of patients
suffering for several DSM-IV diagnosed Emotional Disorders; b) in increasing the
attentional performances of the patients; c) favouring an increase of relaxation, as
measured by EEG, in a clinical population similar to that already showed in normal
subjects practicing maditation.
5.2 Possible explanatory mechanisms. It has been recognised for a long time that
individuals suffering from emotional disorders commonly experience pronounced
elevations of negative cognitive processing. A vast body of research in the ’80 and in
the ’90 have attributed these dysfunctional negative thought contents associated with
emotional disorders to low-level selective processing biases that operate within the
cognitive systems of individuals. These cognitive biases are assumed to favour the
automatic selective processing of emotionally negative information. According to
such accounts, therefore, the mind of patients suffering such disorders are
systematically distorted by processes that operate 'behind the veil', automatically
exerting an implicit influence on subjective experience without either intention or
awareness (Mac Leod and Rutherford, 1998).
So far there is a growing number of studies suggesting the effectiveness of
mindfulness-based clinical intervention (Attentional Traning-MBSR) in treating
several symptoms or syndromes. In the chronic Pain, General Anxiety Disorder and
Panic Disorder (Kabatt-Zinn et al., 1986, 1992) and (Miller et al., 1995). In anxiety
reduction in a normal population (Astin, 1997), in a non-clinical population exposed
to stressful conditions (Shapiro et al., 1988). In decreasing mood disturbances and
stress symptoms in patients with cancer diagnoses (Speca et al. 2000). In preventing
Major Depression recurrence/relapse (Teasdale et al. 2000); modifying depressionrelated long-standing tendencies in memory processes of depressed patients
(Williams 2000). Similarly, the effectiveness of cognitive-behavioural programs
incorporating a substantial mindfulness component in reducing self-harm in
Borderline Personality Disorder (Linehan et al., 1991), in reducing symptomatology
in Obsessive-Compulsive Disorder (Schwartz, 1996) and in binge eating disorder
19
(Kristeller et al., 1999) has been shown. One could wonder why the clinical
application of mindfulness is so 'general purpose' as suggested by these studies.
The 8-week course of the Attentional Training-MBSR program is a
multimodal intervention, including experiential exercises, didactic material, and
providing group social supporting addition to the formal meditation practice.
Although at the basis of each of these components there is mindfulness (Shapiro et
al., 1988), it is a research question to determine to what degree each component
contributes to the effects found. The present study seems to bring some evidences
that attentional processes are specifically affected by the mindfulness-based training.
First of all it should be emphasized that the increased mindfulness does at
first not cure the symptoms, but it changes one's consciousness about them. But then
for emotional disorders changing consciousness is crucial and may very well be the
key to an effective treatment. Mindfulness appears to be strictly linked with attention.
Still, a careful distinction has to be made in order to avoid confusion between the
passive 'automatic pilot ' kind of usual conscious attention, on the one hand, and the
extremely active nature of the attentional aspect present in mindfulness and its
clinical application, on the other hand (Schwartz, 1999). The key point is that the
quality of attention that one places on a sensory or mental 'object' has a critical
implication for the type of conscious states that arise with respect to it. Teasdale used
the term 'meta-awareness' to describe the key feature of active attentional process of
this type (Teasdale, 1997). A distinction has also to be posed between to different
way of 'working' with attention in meditation, that is mindfulness and concentration.
Most of the meditative traditions acknowledge this two basic approach to meditation,
giving then different emphasis to them.
Then there are contemporary research findings that might confirm such
distinction. In an EEG study significant differences were obtained between
concentration and mindfulness states at all bandwidths suggesting that they may be
unique forms of consciousness and not merely degree of a state of relaxation (Dunn
et al., 1999). In a study using a test of sustained attention, meditators were superior in
performance compared to controls. In particular, mindfulness meditators were
superior to concentrative meditators when the stimulus was unexpected but there was
no difference when the stimulus was expected (Valentine et al., 1999).
One possible explanation for the consciousness changing power of
mindfulness might be derived from its nature and application, as described for
example in (Barendregt, 1988, 1996). A person who has developed it, becomes an
aware but detached observer of the mental and physical phenomena to which he or
she has access. Rather than to suffer one is involved in seeing suffering. With this
mental capacity, one then clearly 'sees' the functioning of automatic cognitive
processes. It is this intuitive insight that makes one able to step out from it.
Mindfulness-based training, through the development of 'bare attention', seems to be
able to decrease dysfunctional automaticity of high-level attentional and memory
processes, as ruminative thinking and overgeneral memory. Since data of the present
study indicates that Mindefulness-based attention training does affect low-level
attentional processes also, this is an evidence that its clinical effectiveness actually
could derive from what it was supposed to do, namely enhancing attention.
Mindfulness, as a source of active, aware attentional processes combined with
insight, could make it possible to reduce or even 'dissolve' the dysfunctional
20
automaticity in the mind's processes at different levels. Such a fundamental effect
might explain why Mindfulness Based Attention Training is able to improve
symptoms in several different disorders. Recent research conducted at neurophysiological level had begun to bring experimental data suggesting that the practice
mindfulness, nested in a cognitive-behavioural program, might even be capable of
influencing the generation of new brain circuits (Schwartz, 1997b, 1998). An f-MRI
study showed that the practice of meditation activates neural structures involved in
attention and control of the autonomic nervous system (Lazar et al. 2000).
Both the effects and the nature of mindfulness as well as the underlying
neural mechanisms deserve to be studied further.
Acknowledgements. We like to thank the following persons: Toine van Bakel for
directing the psycho-education group, Michael Kunicki, Eli Wronka, Annika Smit
and Anke Sambeth for EEG recordings and data elaboration, Mariëtte Rijtema,
Marieke van Gool, Mariëlle Pier and Imke Sturkenboom for recording clinical and
neuro-psychological measurements; Han Oud for support on working with SPSS;
Harrie Hendriks for careful advice on statistical methodology and providing an
extension of the MANOVA algorithm. John Teasdale gave critical and useful
comments on a draft of this paper. We also are grateful to the Board of Directors of
Nijmegen University that provided funds for this research.
References
Aitken R., Zealley A., Rosenthal S. 1969. Psychological and physiological measures
of emotion in chronic asthmatic patients. Journal of Psychosomatic Research. 13,
289-297.
Astin J. A. 1997. Stress reduction through mindfulness meditation: Effect of
psychosocial symptoma-tology, sense of control, and spiritual experiences.
Psychotherapy and Psychosomatics. 66, 97-106.
Austin M., Ross M., Murray C., O’Carrol R., et al., 1992. Cognitive function in
major depression. Journal of Affective Disorders. 25, 21-29.
Austin M., Mitchell P., Parker W., Hickie B., Broadty H., Chan J., et al.1999.
Cognitive function in depression: a distinct pattern of frontal impairment in
melancholia?. Psychological Medicine.29, 73-85.
Barendregt H. 1988. Buddhist Phenomenology. In dalla Chiara (Ed.) Proceedings of
the Conference on Topics and Perspectives of Contemporary Logic and Philosophy
of Science, CLUEB, Bologna www.cs.kun.nl/~henk/BP/bp1.htlm, 37-55.
Barendregt H. 1996. Mysticism and beyond, Buddhist Phenomenology II. Eastern
Buddhism, new series. 29, 262-287 www.cs.kun.nl/~henk/BP/bp2.htlm, 262-287.
21
Beckham J., Crawford A., Feldman M., 1998. Trail Making Test performance in
Vietnam combat veterans with and without posttraumatic stress disorder. Journal of
Traumatic Stress.11, 811-819.
Bernhard J., Kristeller J. and Kabat-Zinn J. 1988. Effectiveness of relaxation and
visualization techniques as a djunct to phototherapy and photochemotherapy of
psoriasis. Journal of American Academic Dermatology. 19, 572-573.
de Bruyn B., Hakwoort-Koomen E. 1986. The Dutch WISC-R and it
predecessor. Kind en Adoloscent. 10, 175-182.
Coenen A. M. 1995. Neuronal Activities Underlying the Electroencephalogram and
Evoked Potentials of Sleeping and Waking: Implication for Information Processing.
Neuroscience and Biobehavioural Reviws. 19, 447-463.
Cohen R., Weingartner H., Smallberg S., Pikar D., & Murphy D. 1982. Effort and
cognition in depression. Archives of General Psychiatry. 39, 593-598.
Cornblatt B. and Erlenmeyer-Kimling L. 1985a. Global attentional deviance as a
marker of risk for schizophrenia: Specificity and predictive validity. Journal of
Abnormal Psychology. 94, 470-486.
Cornblatt B., Lenzenweger M., Dworkin R. and Erlenmeyer-Kimling L. 1985b.
Positive and negative schizophrenic symptoms, attention, and information
processing. Schizophrenia Bulletin. 11, 397-408.
Cox C. 1997. Neuropsychological abnormalities in obsessive-compulsive disorder
and their assessment. International Review of Psychiatry. 9, 45-60
Cuijpers P. 1998. A psycho-educational approach to the treatment of depression: a
meta-analysis of Lewinsohn’s 'Coping with depression' course. Behaviour Therapy.
29, 521-533.
Cuijpers P. 1996. Pycho-education in the treatment of unipolar depression.
Tijdschrift voor Psychiatrie. 38, 545-557.
Curran S., Murray C., Van Beck M., Dougall, N. 1993. A single photon emission
computerised tomography study of regional brain function in elderly patients with
major depression and with Alzheimer. British Journal of Psychiatry. 163, 155-165.
Davidson R. J. 1995. Cerebral Asymmetry, emotion and affective style. In R. J.
Davidson & K. Hugdahl (Eds.) Brain asymmetry. Mit Press. Cambridge Mass.
Davies D. & Parasuraman R. 1982. The Psychology of Vigilance. Academic Press.
London.
22
Dunn B., Hartigan J., Mikulas W. 1999. Concentration and mindfulness meditation:
Unique forms of consciousness? Applied Psychophysiology & Biofeedback. 24. 147165.
Fabbro F., Muzur A., Belen R., Calacione R., Bava A. 1999. Effects of praying and a
working memory task in participants trained in meditation and controls on the
occurrence of spontaneous thoughts. Perceptual & Motor Skills. 88. 765-770.
Franke P., Maier W., Hardt J., Frieboes R. 1993. Assessment of frontal lobe
functioning in schizophrenia and unipolar major depression. Psychopatology. 26, 7684.
Friedman R., Steinman M. and Benson H. 1996. The Relaxation Response:
Physiological Effects and Medical Application. In Haruki Y., Ishii Y. & Suzuky M.
(Eds.) Comparative and Psychological Study on Meditation. Eburon. Delft.
van der Gaag M. 1992. The Results of Cognitive Training in Schizophrenic Patients.
Eburon. Delft.
Goodwin G. 1997. Neuropsychological and neuroimaging evidence for the
involvement of the frontal lobes in depression. Journal of Psychopharmacology. 11,
115-122.
Halstead W. 1947. Brain and intelligence: a quantitative study of frontal lobe.
University of Chicago Press, Chicago.
Hamilton M. 1959. The assessment of anxiety states by rating. British Journal
Medical Psychology. 32, 50-55.
Hamilton M. 1960. A rating scale for depression. Journal of Neurology,
Neurosurgery and psychiatry. 12, 56-62.
Hart R., Wade J., Calabrese V., Colenda C. 1998. Vigilance performance in
parkison’s desease and depression. Journal of Clinical & Experimental
Neuropsychology. 20, 111-117.
van Hoof J. J., Hulstijn W., van Mier H., Pagen M. 1993. Figure drawing and
psychomotor retardation: preliminary report. Journal of Affective Disorders. 29, 263266.
van Hoof J. J., Jogems-Kosterman B. J., Sabbe B. G., Zitman F. G., Hulstijn W.
1998. Differentiation of cognitive and motor slowing in the Digit Symbol Test
(DST): differences between depression and schizophrenia. Journal of Psychiatric
Research. 32, 99-103.
23
Hulstijn W. 1996. Writing and Drawing in Neuropsychology: Studies on
Psychomotor Slowness. In Simmer L., Leedham C., Thomassen A. (Eds.).
Handwriting and Drawing Research: Basic and Applied Issues. IOS. Amsterdam.
Jevning R., Walace R. and Beidebach M. 1992. The Pysiology of Meditation: a
Review. A Wakeful Hypometabolic Integrated Response. Neuroscience and
Biobehavioral Review. 16, 415-424.
Jogems-Kosterman B. J., Zitman F. G., van Hoof J. J. and Hulstijn W. 2000.
Psychomotor slowing and planning deficit in schizophrenia. Schizophrenia Research.
Kabat-Zinn, J., 1990. Full Catastrophe Living: The program of the Stress Reduction
Clinic at the University of Massachusset Medical Center. New York. Delta.
Kabat-Zinn, J., Lipwort L., Burney R., & Sellers W. 1986. Four-year follow-up of a
meditation-based program for the self-regulation of chronic pain: Treatment
outcomes and compliance. Clinical Journal of Pain. 2, 159-173
Kabat-Zinn, J., Massion A. O., Kristeller J., Peterson L. G., Fletcher K., Pbert L.,
Lenderking W., Santorelli K. 1992. Effectiveness of a meditation-based stress
reduction program in the treatment of anxiety disorders. American Journal of
Psychiatry. 149, 936-943.
Kabat-Zinn J., Massion A., Hebert J., Rosenbaum E. 1998a. Meditation. In Textbook
of Psycho-oncology, Holland J. (ed.). Oxford U. P., Oxford. 767-779.
Kabat-Zinn J., Wheeler E., Light T., Skillings A., Scharf M., Cropley T., Hosmer D.,
Bernhard J. 1998b. Influence of a mindfulnedss-based stress reduction interventionon
rates of skin clearing in patients with modrate to severe psoriasis undergoing UVB
and PUVA. Psychosomatic Medicine. 60, 625-623.
Kahneman D. 1973. Attention and effort. Prentice Hall. New Jork.
Lader, M. and Marks, I. 1971. Clinical Anxiety. Grune and Stratton. New York.
Lamelin S., Baruch P., Vincent A., Laplante L., Everett J., Vincent P. 1996.
Attention disturbance in clinical depression. Journal of Nervous & Mental Disease.
184, 114-121.
Lamelin S., Baruch P., Vincent A., Everett J., Vincent P. 1997. Distractibility and
processing resource deficit in major depression: Evidence for two deficient
attentional processing model. Journal of Nervous & Mental Disease. 185, 542-548.
Lazar S., Bush G., Gollub R., Fricchione G., Khalsa G., Benson H. 2000. Functional
Brain Mapping of relaxation response and meditation. Neuroreport. 11. 1581-1585.
24
Linehan M. M., Armstrong H., Suarez A., Allmonn D., & Heard H. 1991. CognitiveBehavioural treatment of chronically parasucidal borderline patients. Archives of
General Psychiatry. 48, 1060-1064.
Lezak M. 1983. Neuropsychological Assessment (2d ed.). Oxford U.P. Oxford.
Lockhart R. 1997. Introduction to Statistic and Data Analysis for the Behavioural
Sciences. Freeman and C. New York.
McLeod C.1991. Half a century of research on the Stroop effect: an integrative
review. Psychological Bulletin.109, 163-203.
MacLeod C. and Rutherford E. 1998. Automatic and strategic cognitive biases in
anxiety and depression. In Kisner K. et al. eds.) Implicit and explicit mental
processes . London. Erlbaum.
McNeil D., Tucker P., Miranda R., et al. 1999. Response to Depression and Anxiety
Stroop stimuli in PTSD disorder, OCD disorder, major depressive disorder. Journal
of Nervous & Mental Disease. 187, 512-16.
McNicol, D., 1972. A Primer of Signal Detection Theory. London. George
Allen&Unwin.
Miller J., Fletcher K., and Kabat-Zinn J. 1995. Three-year follow-up and clinical
implications of a mindfulness-based stress reduction intervention in the treatment of
anxiety disorders. General Hospital Psychiatry. 17, 192-200.
Muirhead R. .J. 1982. Aspects of multivariate statistical theory. Wiley Series in
Probability and Mathematical Statistics. New York. John Wiley & Sons.
Nelson E., Sax K., Strawoski S., 1998. Attentional performance in patients with
psychotic and non-psychotic major depression and schizophrenia. America Journal of
Psychiatry. 155, 137-139.
van Nieuwenhuizen C. 1998. Quality of life of persons with severe mental illness: an
instrument. Thesis Publishers Amsterdam.
van Nieuwenhuizen C. 2000 Unpublished data
Nuechterlein K. and Dawson M. 1984. Information processing and attentional
functionong in the developemental course of schizophrenic disorder. Schizophrenia
Bulletin. 10, 160-203.
Nuechterlein, K., Edell, W., Norris, M., and Dawson, M. 1988. Attentional
Vulnerability Indicators, Thought disorder, and negative Symptoms. Schizophrenia
Bulletin. 12, 408-426.
25
Olivier J., Huxley P., Priebe S., & Kaiser W. 1997. Measuring the quality of life of
severly mentally ill people using the Lancashire Quality of Life Profile. Social
Psychiatry and Psychiatric Epidemiology. 37, 76-83.
Parikh S., Kusumakar V., Haslam D., et al. 1997. Psychosocial intervention as an
adjunct to pharmacotherapy in bipolar disorder. Canadian Journal of Psychiatry. 42,
745-785.
Randolph P., Caldera Y., Tacone A., et al. 1999. The long-term combined effect of
medical treatment and a mindfulness-based behaviuoral program for the
multidisciplinary management of chronic pain in West Texas. Pain Digest. 9, 103112.
Reitan, R., Davison, L. 1974. Clinical Neuropsychology: Current Status and
Application. Wiley. New York.
Rosvold, E., Mirsky, A., Sarason, I., Bransome, E., Beck, L. 1956. A continuous
performance test of brain damage. Journal of Consulting Psychology. 20, 343-350.
Rush, A. 1999. Strategies and tactics in the management of maintenance treatment
for depressed patients. Journal of Clinical Psychiatry. 60, 21-26.
Sabbe, B. G., Hulstijn W., van Hoof J. J., Zitman F. G. 1996a. Fine Motor
Retardation and depression. Journal of Psychiatric Research. 30, 295-306.
Sabbe, B. G., van Hoof J. J., Hulstijn, W., Zitman F. G. 1996b. Changes in the fine
motor retardation in depressed patients treated with fluoxetine. Journal of Affective
Disorders. 40, 149-157.
Sabbe, B. G., Hulstijn W., van Hoof J. J., Zitman F. G. 1997. Depressive retardation
and treatment with fluoxetine: assessment for the motor component. Journal of
Affective Disorders. 43(1), 53-62.
Schatzberg, A. F., Posener J.A., DeBattista C., Kalehzan B. M., et al. 2000.
Neuropshychological Deficits in Psychotic Versus Non-psychotic Major Depression
and No Mental Illness. American Journal of Psychiatry. 157, 1095-1100.
Schneider, W. & Shiffrin R. 1977. Controlled and automatic human information
processing: Detection, search and attention. Psychological Review. 84, 1-66.
Schwartz, J.M., Stoessel, P.W. et al. 1996. Systematic changes in cerebral glucose
metabolic rate after succesful behavior modification treatment of obsessivecompulsive disorder. Archives of General Psychiatry. 53, 109-13.
Schwartz, J. M., 1997a. Obsessive Compulsive Disorder. Science & Medicine. 4 (2),
14-23.
26
Schwartz, J. M., 1997b. Cognitive-behavioural self-treatment for obsessivecompulsive disorder
systematically alters cerebral metabolism: A mind-brain interaction paradigm for
psychotherapists, in Obsessive Compulsive Disorders: Diagnosis, Etiology
Treatment, ed. E. Hollander and D.J. Stein. New York. Marcel Dekker.
Schwartz, J. M., 1998. Neuroanatomical aspects of cognitive-behavioural therapy
response in obsessive-compulsive disorder: An evolving perspective on brain and
behaviour. British Journal of Psychiatry. 173 (suppl. 35), 38-44.
Schwartz, J. M., 1999. First steps toward a theory of mental force: PET imaging of
systematic cerebral changes after psychological treatment of obsessive-compulsive
disorder. In Toward a Science of Consciousness III, Hameroff A., Kaszniak D.,
Chalmers D. . MIT Press, Cambridge Mass., 111-122.
Segal, Z. V., Williams, J. M., Teasdale J. D. (in press). Mindfulness and prevention
of depression: A guide to the theory and practice of mindfulness-based cognitive
therapy. Guilford Press. New York
Shapiro, S., Schwartz G. E. And Bonner J. 1988. Effects of Mindfulness-based Stress
Reduction on Medical and Premedical Students. Journal of Behavioral Medicine.21
(6), 581-598.
Speca, M., Carlson L., Goodey E., Angen M. 2000. A randomised, wait-list
controlled clinical trial: The effect of a mindfulness meditation-based stress reduction
program on mood and symptom of stress in cancer patients. Psychosomatic
Medicine. 62. 613-622.
Stroop, J. R. 1935. Studies of interference in serial verbal reactions. Journal of
Experimental Psychology. 18. 643-662.
Teasdale, J.D., Segal Z., Williams J. M. 1995. How does Cognitive Therapy prevent
depressive relapse and why should attentional control mindfulness) training help?.
Behaviour Research and Therapy. 33, 25-39.
Teasdale, J. D., Segal Z. V., Williams, J. M., Ridgeway V.A., Soulsby J.M., Lau
M.A. 2000. Prevention of Relapse/Recurrence in Major Depression by MindfulnessBased Cognitive Therapy. Journal of Consulting and Clinical Psychology. 68.615623.
Teasdale, J.D. 1997. The relationship between cognition and emotion: The mind-inplace in mood disorder. In Clark M. D. & Fairburn C. G. (Eds.) Science and practice
of cognitive behaviour therapy. Oxford U.P, Oxford.
Teulings, H. and Maarse F. 1984. Digital recording and processing of handwriting
movements. Human Movement Science. 3, 193-217.
27
Thomassen, A. and van Galen G. 1992. Handwriting as a motor task:
Experimentation, modelling, and simulation. In Summers J. (Ed.). Approaches to the
study of motor control and learning. North Holland. Amsterdam.
Treisman, A. and Gelade G. 1980. A feature-integration theory of attention.
Cognitive Psychology. 12, 97-136.
Valentine, E., Sweet L 1999. Meditation and attention: A comparison of the effect of
concentrative and mindfulness meditation on sustained attention. Mental Health,
Religion & Culture. 2. 59-70.
Wechsler, D. 1981. Wechsler Adult Intelligent Scale-Revised Test Manual. The
Psychological Corporation. New York.
Weingartner, H., Choen R., Murphy D., Martello J. & Gerdt C. 1981 Cognitive
processes in depression. Archives of General Psychiatry. 38, 42-47.
White, D., Myerson J., Hale S.1997. How cognitive is psychomotor slowing in
depression? Evidence from a meta-analysis. Aging Neuropsychology and Cognition.
4, 166-174.
White, J. M., 1998. 'Stress control' large group therapy for generalised anxiety
disorder. Two years follow-up. Behavioural and Cognitive Psychotherapy. 26, 237245.
Williams, J. M. 1996. Autobiographical memory in depression. In Rubin D. ed.)
Remembering our past: studies in autobiographical memory. Cambridge University
Press, Cambridge.
Williams, J. W. 1988. A structured interview guide for the Hamilton Depression
Rating Scale. Archive of General Psychiatry. 45, 742-747.
Williams, J. M., Teasdale J.D., Segal Z., Soulsby J. 2000. Mindfulness-Based
Cognitive therapy reduces overgeneral autobiographical memory in formerly
depressed patients. Journal of Abnormal Psychology. 109, 150-155.
Wolfe, J., Granholm E., Butters N., Saunders E.& Janowski D. 1987. Verbal memory
deficit associated with major affective disorders: a comparison of unipolar and
bipolar pateints. Journal of Affective Disorders.13, 83-92.
Zung, W., 1965. A self rating depression scale. Archive of General Psychiatry. 12,
65-70.
28
Table 1.
Treatment
Mindfulness-based Att ention Training
a
Outcome variables
Hamilton Depression PRE
N
(listwise)
Mean
Std.
Deviation
Psy choeducation
N
(listwise)
Mean
Std.
Deviation
9
17,67
4,97
8
17,50
7,01
Hamilton Depression POST
9
13,33
6,50
8
10,50
6,97
Hamilton Anxiety PRE
9
16,22
4,76
8
16,13
7,26
Hamilton Anxiety POST
9
11,67
7,66
8
9,50
5,37
Zung Depression PRE
9
56,00
8,46
8
52,38
9,32
Zung Depression POST
9
48,89
11,88
8
46,25
11,93
VAS Anxiety PRE
9
61,33
18,91
8
52,50
25,34
VAS Anxiety POST
9
41,77
22,17
8
59,75
28,39
VAS Depression PRE
9
77,00
16,30
8
60,50
24,83
VAS Depression POST
9
56,33
30,66
8
57,75
30,70
Lqlp_7 PRE
9
4,30
,65
8
4,62
,70
Lqlp_7 POST
9
4,41
,70
8
4,92
,81
Lqlp_3 PRE
9
1,76
,25
8
1,79
,27
Lqlp_3 POST
9
1,97
,36
8
2,03
,43
Stroop Test (Ln) PRE
9
3,72
,45
8
3,30
,29
Stroop Test (Ln) POST
9
3,53
,44
8
3,34
,30
CPT_d' PRE
9
3,37
,95
8
3,35
1,07
CPT_d' POST
9
3,86
,75
8
3,62
,96
Trail-M aking B (Ln) PRE
9
4,52
,58
8
4,32
,41
Trail-M aking B (Ln) POST
9
4,37
,40
8
4,17
,28
WISC-M aze (Ln) PRE
9
3,37
,35
8
3,53
,50
WISC-M aze (Ln) POST
9
3,33
,42
8
3,51
,54
DST Raw-score PRE
9
41,56
13,18
8
49,75
15,08
DST Raw-score POST
9
44,78
11,77
8
53,25
16,24
DST M atching-time (Ln) PRE
9
,544
,388
8
,270
,439
DST M atching-time (Ln) POST
9
,403
,320
8
,192
,429
a. (Ln) = natural-logaritmic tranformation
29
Table 2 a. Mindfulness-based Attention Training Pai red S amples S tati stics
N
(pairwis e)
12
Mean
18,75
Std . Deviation
6,28
Hamilto n Depres sion POST
12
14,50
6,63
Hamilto n An xiet y PRE
12
18,33
6,23
Hamilto n An xiet y POST
12
12,08
6,82
Zu ng Depressio n PRE
12
56,75
8,41
Zu ng Depressio n POST
12
50,25
10,46
VA S A nxiet y PRE
10
64,30
20,15
VA S A nxiet y POST
10
44,90
23,12
VA S Depres sion PRE
10
77,30
15,40
VA S Depres sion POST
10
59,10
30,20
Lq lp_7 PRE
14
4,23
,66
Lq lp_7 POST
14
4,31
,66
Lq lp_3 PRE
14
1,70
,22
Lq lp_3 POST
14
1,83
,36
Stroop Test (Ln) PRE
14
3,86
,60
Stroop Test (Ln) POST
14
3,55
,52
CPT_d ' PRE
14
3,19
,98
CPT_d ' POST
14
3,52
1,01
Trail-M akin g B (Ln) PRE
14
4,56
,53
Trail-M akin g B (Ln) POST
14
4,39
,43
W ISC-M aze (Ln ) PRE
14
3,39
,37
W ISC-M aze (Ln ) POST
14
3,34
,45
DST Raw-score PRE
12
40,58
13,06
DST Raw-score POST
12
43,67
13,70
DST M atch ing-t ime (Ln) PRE
11
,60
,37
DST M atch ing-t ime (Ln) POST
11
,49
,35
Hamilto n Depres sion PRE
30
Table 2b. Psycho-education Paired Samples Statistics
Hamilton Depression PRE
N (pairwise)
11
Mean
17,09
Std. Deviation
6,12
Hamilton Depression POST
11
11,36
6,67
Hamilton Anxiety PRE
11
15,00
6,78
Hamilton Anxiety POST
11
10,00
5,27
Zung Depression PRE
11
53,82
8,48
Zung Depression POST
11
49,18
11,23
VAS Anxiety PRE
11
48,82
23,58
VAS Anxiety POST
11
60,45
25,37
VAS Depression PRE
11
63,73
23,83
VAS Depression POST
11
58,64
26,66
Lqlp_7 PRE
11
4,37
,73
Lqlp_7 POST
11
4,62
,86
Lqlp_3 PRE
10
1,78
,25
Lqlp_3 POST
10
1,97
,40
Stroop Test (Ln) PRE
11
3,26
,33
Stroop Test (Ln) POST
11
3,29
,33
CPT_d' PRE
11
3,27
,95
CPT_d' POST
11
3,61
,98
Trail-M aking B (Ln) PRE
9
4,27
,41
Trail-M aking B (Ln) POST
9
4,12
,30
WISC-M aze (Ln) PRE
10
3,41
,55
WISC-M aze (Ln) POST
10
3,38
,58
DST Raw-score PRE
10
51,30
14,03
DST Raw-score POST
10
52,70
17,31
DST M atching-time (Ln) PRE
10
,25
,40
DST matching-time (Ln) POST
10
,24
,44
31
TABLE 3a.
Paired T Tests Mindfulness-based Attention Training
Pre-Post Mean
a
Difference
-4,25*
Std. Deviation
4,99
Hamilton Anxiety
-6,25*
6,22
12
,005
1,00
Zung Depression
-6,5*
9,56
12
,038
,67
VAS Anxiety
-19,4*
28,15
10
,057
.69
VAS Depression
-18,2*
22,28
10
,030
,82
0,07*
,40
14
,486
,18
c
Outcome Variables
Hamilton Depression
Lqlp_7
Lqlp_3
N
(pairwise)
12
b
p (2-tailed)
,013
Effect Size
(Cohen's d)
,85
0,14*
,22
14
,035
,64
-0,31*
,48
14
,032
,64
0,33*
,56
14
,049
,59
Trail-M aking B (Ln)
-0,16*
,26
14
,035
,62
WISC-M aze (Ln)
-0,05*
,17
14
,257
,29
3,08*
4,62
12
,041
,67
-0,11*
,15
11
,044
,72
Stroop Test (Ln)
CPT_d'
DST Raw-score
DST M atching-time (Ln)
a. The * indicat es positive change/improvement of the M ean Difference
b. Values displayed in boldface indicate p< 0.05; values disp layed in italic indicate a trend for significance (p<0.1)
c. (Ln) = natural-logaritmic transformation
TABLE 3b. Paired T Tests Psychoeducation
c
Outcome variables
Hamilton Depression
Pre-Post Mean
a
Difference
-5,72*
Std. Deviation
4,54
N
(pairwise)
11
b
p (2-tailed)
,002
Effect Size
(Cohen's d)
1,25
Hamilton Anxiety
-5,00*
4,94
11
,007
1.00
Zung Depression
-4,64*
7,23
11
,059
,64
VAS Depression
-5,09*
26,80
11
,543
,19
VAS Anxiety
11,64
26,11
11
,170
,44
Lqlp_7
0,25*
,39
11
,056
,64
Lqlp_3
0,19*
,31
10
,084
,61
,03
,20
11
,632
,15
Stroop Test (Ln)
CPT_d'
0,33*
,46
11
,035
,72
Trail-M aking B (Ln)
-0,14*
,22
9
,087
,73
WISC-M aze (Ln)
-0,02*
,17
10
,672
,11
1,4*
8,37
10
,610
,17
-0,01*
,23
10
,862
,04
DST Raw-score
DST M atching-time (Ln)
a. The * indicat es positive change/improvement of the M ean Difference
b. Values displayed in boldface indicate p< 0.05; values disp layed in italic indicate a trend for significance (p<0.1)
c. (Ln) = natural-logaritmic transformation
32
Figure A. Pre and post distributions (listwise) of the Clinical and
Quality of Life variables
40
30
20
10
Pre
0
N=
Post
9
9
8
Mindfulness-based
8
Psychoeducation
Hamilton Depression
40
30
4
20
10
9
0
N=
Pre
Post
9
9
Mindfulness-based
8
8
Psychoeducation
Hamilton Anxiety
33
70
60
50
40
30
Pre
20
N=
Post
9
9
8
Mindfulness-based
8
Psychoeducation
Zung Depression
100
80
60
40
20
Pre
0
N=
Post
9
9
8
Mindfulness-based
8
Psychoeducation
VAS Anxiety
100
80
60
40
8
20
0
N=
Pre
Post
9
9
Mindfulness-based
8
8
Psychoeducation
VAS Depression
34
6,0
5,5
5,0
4,5
4,0
3,5
3,0
N=
Pre
Pos t
9
9
8
Mindf ulness -based
8
Psy choeducation
Lqlp_7
3,0
2,7
2,4
2,1
1,8
1,5
1,2
N=
Pre
Post
9
9
8
Mindfulness-based
8
Psychoeducation
Lqlp_3
35
Figure B. Pre and post distributions (listwise) of the
Neuropsychological variables
5,0
4,5
4,0
3,5
3,0
Pre
2,5
N=
Post
9
9
8
Mindfulness-based
8
Psychoeducation
Stroop Test (Ln)
5
4
3
2
Pre
1
N=
Post
9
9
8
Mindfulness-based
8
Psychoeducation
CPT_d'
36
6,0
5,5
5,0
4,5
4,0
3,5
N=
Pre
Post
9
9
8
Mindfulness-based
8
Psychoeducation
Trail-Making B (Ln)
4,5
4,0
3,5
3,0
Pre
2,5
N=
Post
9
9
Mindfuless-based
8
8
Psychoeducation
WISC-Maze (Ln)
37
90
80
70
60
50
40
30
Pre
20
10
N=
Post
9
9
8
Mindfulness-based
8
Psychoeducation
DST Raw-score
1,5
1,0
,5
0,0
-,5
-1,0
N=
Pre
Post
9
9
Mindfulness-based
8
8
Psychoeducation
DST Matching-time (Ln)
38
Figure C
Treatments Main Effect
whole sample (both groups)
F(1,19)=6,06; p<,0236
0,035
Alpha Power
0,03
0,025
0,02
0,015
0,01
0,005
0
Pre Treatment
1
Post Treatment
A slight modification is used of the test described in Muirhead 1982), Theorem 3.2.13, pg. 98. In the
formula we use
T 2 N ( X )' S 1 X with X being the average effect of a given Training, say Training
1, and S the estimated covariance structure of the effect of both Trainings. So given the individual
effects X 1 ... X k for the patients of Training 1, and Y1...Yl for Training 2, one may take
1
(( X i X )( X i X )'(Y j Y )(Y j Y )' )
k 1 l 1
and N k . Moreover, m denotes the dimensionality of the X values, m 13 when considering all
variables. Then under the null-hypothesis that the expected value of X is 0, the statistic
T 2 k l m 1
is Fisher distributed with degrees of freedom m, k l m 1. The formula
k l 2
m
S
has been implemented by means of a Splus program.
The estimated Cohen’s d effect size for within-subject design is calculated as the ratio between the mean
of pre-post difference scores and the SD of difference scores. According to Cohen, a d-value of 0.8 or
more is a large effect size; a d-value of 0.5 or more is a medium effect size; a d-value of 0.2 or more is
considered small. (Lockhart, 1997; cap. 3).
2
39