EMERGENCIES IN PEDIATRIC ENDOCRINOLOGY
advertisement

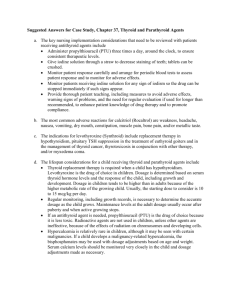
EMERGENCIES IN PEDIATRIC ENDOCRINOLOGY פריס-דר' ליאת דה THYROID STORM Thyroid storm is a decompensated state of thyrotoxicosis that can be fatal unless recognized and aggressively treated. The diagnosis of thyroid storm is based on a high index of suspicion, and treatment must be instituted on an emergency basis prior to the availability of confirmatory thyroid function tests. Pathophysiology: The mechanism causing progression from thyrotoxicosis to storm have not been determined. Serum levels of free T4 and T3 in compensated thyrotoxicosis and in patients suffering from thyroid storm are similar and there is no absolute level above which thyroid storm inevitably occurs. However it seems that an acute elevation of free T3 and T4 (e.g. following withdrawal of antithyroid drugs, surgery or iodine-131 therapy) may cause systemic decompensation and result in thyroid storm. Thyroid storm is a systemic disease, and the effects of excess thyroid hormone result in a spectrum of metabolic responses. Major mechanisms producing thyroid storm are: 1. Sympathetic overactivity which results partially from an increased number of betaadrenergic receptors on target organs, and probably also due to postreceptor supersensitivity. Serum catecholamines are not increased. 2. Increase in metabolic rate due to induction of key enzymes regulating metabolism (such as Na-K-ATPase. Thyroid storm is very rare in children, and may appear during neonatal life or during childhood. NEONATAL THYROTOXICOSIS Neonatal thyrotoxicosis is caused by two mechanisms: 1. Transient thyrotoxicosis caused by transplacental transfer of thyroid stimulating antibodies from a mother who suffers at present or had suffered in the past from Graves’. 2. Congenital persistent thyrotoxicosis caused by an activating mutation in the gene for the TSH receptor, causing constitutive activation of the receptor. Clinical features of neonatal thyrotoxicosis usually include thyromegaly, although this may not always be obvious, and tachycardia. The thyromegaly causes local obstruction or ventilatory compromise. Cardiomegaly and high output congestive heart failure may occur in severe disease. The infants may be preterm or small for gestational age and irritable, restless and febrile (similar to infants born to addicted mothers). The weight loss or poor weight gain despite a voracious appetite, the warm and flushed skin, and the appearance of the infant are also similar to infants born to addicted mothers. Ophthalmic signs are often present and include periorbital edema, stare, lid retraction and proptosis. Less often the infant has hepatosplenomegaly, thrombocytopenia, petechiae, jaundice, lymphadenopathy, and the hyperviscosity syndrome. The onset may be within 24 hours of birth or as late as 6 weeks post delivery. Diagnosis is based on 1 1. A history of maternal hyperthyroidism at present or in the past. 2. Thyroid functions (elevated T3 and free T4, and undetectable TSH) and positive TSH receptor antibodies. 3. Maternal thyroid functions as well as TSH receptor antibodies will confirm the diagnosis of transplacental transfer of antibodies. Radionuclide imaging and uptake or ultrasonography rarely are of value. Differential Diagnosis: 1. Heart failure 2. Sepsis 3. Inborn error of metabolism 4. Infant of an addicted mother 5. Dehydration 6. Thyrotoxicosis 7. Hemolysis. Management Supportive care Adequate hydration with fluid, glucose and nutrient support. Treat fever Digitalis and diuretic therapy for congestive heart failure. Adequate oxygenation. When thyromegaly compromises the airway exchange- elevation and mild extension of the head. Specific therapy 1. Beta-blocker –Propranolol 2mg/Kg/day in 3-4 divided doses. Mechanism of action 1) Blocking the catecholamine-mediated effect. 2) Inhibition of monodeiodination of T4 to T3. 2. Iodine therapy – Lugol solution or 10%KI 1 drop x 3/day Mechanism of action: 1) Inhibition of the secretion of stored T3 and T4. 2) Blocking thyroid hormone synthesis (transiently). 3. Antithyroid drugs Propylthiouracil (PTU) 5-10 mg/Kg/day In 3 divided doses Methimazole (MTZ) 0.5-1 mg/Kg/day Mechanism of action: 1) Both drugs block thyroid hormone synthesis. 2) PTU also inhibits the monodeiodination of T4 to T3 in peripheral tissues, thus is the drug of choice in thyroid storm. THYROID STORM IN CHILDREN AND ADULTS An acute elevation of thyroid hormone in the thyrotoxic patient results in thyroid storm. Causes of thyrotoxicosis 1. Graves’ disease 2. Excess TSH: 1) Pituitary adenoma 2) Pituitary thyroid hormone resistance 3. Toxic adenoma or carcinoma 4. Toxic nodular goiter 5. Iodine induced 2 6. Thyroiditis: infectious, subacute. 7. TSH secreting tumors 8. LT4 ingestion. Precipitating factors in thyroid storm: MEDICAL Infection Pulmonary embolus Diabetic ketoacidosis Iodine-131-therapy Iodine (drugs and dyes) Thyroid hormone excess Cardiovascular accident SURGICAL Thyroid surgery Major and minor surgery Tooth extraction Childbirth Dilatation and curettage Clinical features of thyroid storm General: Hyperkinesis, Hyperpyrexia (up to 41°c), sweating. Cardiovascular: Palpitations, shortness of breath, Tachycardia, Arrhythmias (new onset). Endocrine: Goiter Eyes: Proptosis, stare. Gastrointestinal: Diarrhea, Weight loss, Hepatomegaly, Jaundice. Some patients present with nausea, vomiting and severe diarrhea which may mimic an acute abdominal pain. Nervous system: Restlessness, tremor, psychosis, apathy, coma, and hyperreflexia. Diagnosis The diagnosis and initial treatment must be based on clinical evaluation. 1. Thyroid function test (elevated T3 and free T4, and undetectable TSH. Rarely there is isolated increase in T3: "T3 toxicosis"). 2. A variety of biochemical abnormalities reflecting hepatic, adrenal, and renal decompensation characterize patients with thyroid storm. Liver function tests may reveal elevated bilirubin, SGOT, SGPT, prolonged PT. Hypercalcemia and hyperglycemia may occur. Hypoglycemia is an ominous finding. Renal functions: elevated creatinine and BUN indicate prerenal azotemia. Adrenal insufficiency may be associated and manifest as NaK, Ca. Management Similar to neonatal management. Doses written below are for adult patients (are not to be memorized). Supportive care: As for neonates. Reduction in fever is important because an increased temperature not only increases metabolic demandes, but also the percent of free T4. Acetaminophen is preferred to salicylates, since the latter affect the binding of T4 and T3 to their binding proteins. Specific therapy: 1. PTU. Loading dose 900-1200 mg PO or nasogastric tube, then 300-600mg : 3/day. 3 2. Iodine as sodium-iodine 1gr every 8 hours IV, or Lugol's solution 20 drops x 3/day. Lithium carbonate may be used in patients with a history of iodine allergy as it reduces secretion of thyroid hormones. 3. Propranolol: PO 20-80 mg every 6 h. IV 1-2 mg every 5 minutes up to 10 mg total. Contraindicated in bronchospasm and congestive heart failure. 4. Steroids: Hydrocortisone 100-300 mg as initial bolus, then 50-100 mg tid. Mechanism of action: 1) Inhibition of hormone secretion. 2) Inhibition of T4 conversion to T3. 5. Dialysis. When medial treatment is ineffective or cause unacceptable side effect 6. Surgery. As a last resort in patients who are not responding to intensive therapy. MYXEDEMA COMA Myxedema coma is the end point of chronic hormone deficiency manifested by multiorgan dysfunction affecting respiration, cardiac performance, mental status and thermoregulation. In addition myxedema is associated with a spectrum of hematologic, biochemical, and immunologic derangement. The condition is seen most often in elderly women who have chronic hypothyroidism from a spectrum of causes, and is extremely rare in children. The mortality rate remain high (50% despite optimal therapy). Respiratory system Myxedema causes respiratory decompensation due to a complex interaction of factors: 1. Macroglossia + upper airway edema → upper airway obstruction. 2. Respiratory muscles edema + pleural effusion → Restricted breathing. 3. Depression of hypoxia-mediated-respiratory-response + reduced response to hypercapnia → CO2 narcosis → coma. Cardiovascular manifestation Despite the increase in total body water, myxedema patients have a reduced effective intravascular volume and a propensity to hypotension, cardiovascular collapse and shock. 1. Pericardial effusion. 2. Bradycardia. 3. Hypotension. 4. Reduced myocardial contractility → diminished stroke volume. Impaired thermoregulation Hypothermia, which occurs in many (75%) patients with myxedema coma results from: 1. Decreased basal metabolic rate. 2. Dysfunction of the thermoregulatory center. Renal and electrolytes alterations Dilutional hyponatremia is a common finding resulting from 1. Decreased GFR 2. Decreased delivery of water to the distal tubule. 3. Deficiency of atrial natriuretic factor – probably. 4. Syndrome of inappropriate ADH secretion – in some cases. 4 Gastrointestinal alteration Paralytic ileus is due to both impaired motility and gut wall edema. Infection Myxedema patients are susceptible to infection as hypothyroidism is associated with impaired leukocytic response to infective organisms. Thus, leukocytosis may not develop during acute infection in such a patient. Diagnosis The diagnosis is based on a detailed clinical evaluation of clinical data indicating hypothyroidism and events precipitating coma. Physical findings SKIN – dry, rough, yellowish discoloration, and hyperkeratosis around elbows and knees. Diffuse alopecia. Vitiligo may provide a hint to autoimmune diseases. FACE – puffy face and eyelids with loss of the outer third of the eyebrows. NECK – goiter or a scar consistent with previous thyroid surgery. HYPOVENTILATION AND CYANOSIS HYPOTHERMIA MACROGLOSSIA AUSCULTATION – signs of pleural and pericardial effusion, faint heart sounds and bradycardia. NEUROLOGICAL SIGNS – diminished or absent deep tendon reflexes, diminished muscle power but no cranial nerve deficit. Muscles may appear bulky. Laboratory tests Specific diagnostic tests: Elevated serum TSH Low serum T4 and fT4 Low or normal total T3 and free T3 Nonspecific tests ECG: Bradycardia, low voltage, prolonged QT interval Radiograph: Chest: Pleural effusion, cardiomegaly. Skull: Enlarged sella in secondary hypothyroidism. Arterial blood gases: Hypoxia, hypercapnia. Anemia SGOT, CPK, LDH: abnormal Elevated cholesterol and triglycerides. Hypoglycemia Hyponatremia Hypercalcemia Cortisol (normal or low) Things to be aware of when interpreting thyroid function tests: Serum total and free T3 may be normal or only marginally decreased in hypothyroidism, therefore T3 measurement is not a useful test. In coma associated with pituitary or hypothalamic hypothyroidism TSH will be normal or low. Low serum total and free T4 in the critically ill patient may indicate the euthyroid sick syndrome. Such patients will have normal or slightly elevated TSH (<15 μU/ml), and increased reversed T3. The use of dopamine in the shocked patient may normalize an elevated TSH and the true diagnosis of hypothyroidism may be overlooked. Management 5 Therapy should include aggressive management of any precipitating factor, supportive therapy, and thyroid hormone replacement. Detection of precipitating factor Note that the normal temperature and leukocyte count may be inappropriate in the myxedema coma patient with associated infection. Thyroid hormone replacement: LT4 500 μg IV (bolus) followed by 50-100 μg IV or 100-200 μg PO daily. Respiratory failure: Mechanical ventilation an adequate oxygenation. Hyponatremia: Fluid restriction and careful volume expansion with D5/0.5 NS to treat both hyponatremia and hypoglycemia. Hypothermia: Avoid external heat source. Cover with blankets. Steroids: Adrenal insufficiency may co-exist on the basis of either hypopituitarism or primary autoimmune adrenal failure. In addition it is believed that the ACTH response to stress is relatively deficient in myxedema coma and hypothermia. Hydrocortisone 100 mg IV and 50-100 mg tid daily. ADRENAL CRISIS Acute or chronic adrenal insufficiency. It may present in: A. Patients known to have chronic adrenal insufficiency if 1) Maintenance dose is inadequately raised in stress (e.g. infection, surgery, trauma) 2) As a result of withdrawal of maintenance steroid therapy. 3) Initiation of medical treatment by LT4, Insulin, morphine or barbiturates. B. Adrenal crisis may be the initial presentation in one third of the patients. It may also be the first presentation in an infant with congenital adrenal hypoplasia or congenital adrenal hyperplasia (CAH) or with adrenal hemorrhage. Clinical manifestation of adrenal insufficiency Chronic 1. Fatigue 2. Anorexia 3. Weight loss 4. Hyperpigmentation 5. Hypotension 6. Salt craving 7.Decreased pubic and axillary hair(adrenal androgen deficiency) Acute 1. Abdominal pain (may mimic acute abdomen) 2. Fever 3. Hypotension 4. Dehydration 5. Shock 6 6. Hypoglycemia 7. Tachycardia and piliform pulse Laboratory findings 1. 2. 3. 4. 5. 6. 7. Na K, acidosis Hypoglycemia BUN and creatinine may be elevated (prerenal azotemia) Neutropenia with relative lymphocytosis and eosinophilia Low cortisol level Increased ACTH in primary insufficiency. ECG: peaked T waves first. Later prolonged P-R and widened QRS. Management When there is a decline in clinical status, such as the presence of hypotension, fever, decreasing mental status or acute intercurrent illness, treatment must be administered immediately, even before the diagnosis is made. FLUIDS – to restore intravascular volume, renal perfusion and correct hyponatremia and hypoglycemia. - IV 0.9% NaCl 20cc/Kg over 1 h - If hypoglycemic IV 20% glucose, 2cc/Kg (10% glucose in newborns) Followed by 0.9% NaCl + 5% Dextrose at a rate of 1.5 to 2 times maintenance (2250 to 3000 mL/M2/day). Glucocorticoid replacement Hydrocortisone sodium succinate. IV bolus 50 mg for babies and 100-150 mg for larger children and adolescents. Followed by 100 mg/ M2/day in four doses. (This amount of hydrocortisone has sufficient mineralocorticoid activity). Treatment of hyperkalemia Depending on severity of hyperkalemia and availability of treatment one of the following: 1. Kayexalate (resine) 2. 10% calcium gluconate followed by NaCO3. 3. Insulin + glucose 4. Dialysis Maintenance and repair When the serum sodium is >135 mEq/L , the IV fluid can be changed to 0.45% NaCl with 5% glucose. Monitor electrolytes and BUN every 4 h, glucose every 2 h. Do not give K until serum concentration <5mEq/L, and the patient is urinating. Long term maintenance is 15-20 mg/ M2/day in 3 doses. If aldosterone is deficient, add oral fludrocortisone 0.1 mg. NEONATAL HYPERCALCEMIA 7 Neonatal hypercalcemia can be a life threatening disorder, which can be complicated by: 1. Severe dehydration due to polyuria as a result of resistance ADH (nephrogenic DI) 2. Severe Hypertension: direct vasoconstrictive effect of calcium + increased renin-angiotensin activity. 3. CNS: lethargy, hypertonia and seizures. 4. Metastatic calcification including irreparable nephrocalcinosis and renal stones. Causes of neonatal hypercalcemia 1. Iatrogenic –overtreatment 2. Primary hyperparathyroidism 3. Neonatal hyperparathyroidism secondary to maternal hypocalcemia 4. Following an episode of subcutaneous fat necrosis. 5. Bartter Syndrome 6. Breast milk rickets of prematurity 7. Infantile hypophosphatasia 8. Familial benign hypocalciuric hypercalcemia. 9. Excess of vitamin D in breast milk. 10.Maternal drugs during third trimester: thiazides, lithium vitamin D. 11.Williams syndrome Management of hypercalcemia When serum total calcium concentration is more than 13.5-14 mg/dl emergency intervention is necessary. 1. Hydration with isotonic saline : maintenance x 2. 2. Calciuresis – after hydration: IV Fusid 1mg/Kg (inhibits renal tubular Ca reabsorption. 3. Inhibition of bone resorption – calcitonin, steroids, bisphosphonates, plicamycin and gallium nitrate. The latter three are experimental in children. 4. Treatment of the primary cause to hypercalcemia. 5. Discontinuation of treatment with medication that contribute to hypercalcemia.(Vit A, Vit D, etc.) 6. Reduction of dietary intake of calcium. CHILDHOOD HYPERCALCEMIA Clinical features Most symptoms reflect disturbances in the renal, gastrointestinal, cardiovascular, neuromuscular and CNS systems. 1. 2. 3. 4. CNS – weakness, anorexia, nausea, emesis, depression, confusion and stupor. Cardiovascular – hypertension, arrhythmias. Renal – Nephrogenic diabetes insipidus, nephrocalcinosis, GFR↓. Gastrointestinal – constipation, acute pancreatitis, symptomatic peptic ulcer. Management – as for neonates. HYPOCALCEMIA 8 Early neonatal hypocalcemia – occurs within the first 3 days of life and is mostly encountered in 3 situations; 1) preterm infants, 2) Asphyxiated infants and 3) infants of insulin-dependent diabetes mellitus. Late neonatal hypocalcemia – occurs after three days post gestation. The three major causes of late neonatal hypercalcemia are 1) phosphate loading (overtreatment or cow milk hyperphosphatemia). 2) hypoparathyroidism (primary or secondary to maternal hypercalcemia). 3) hypomagnesemia. Classification of major causes of hypocalcemia 1. Disorders of parathyroid gland (PTH deficiency, suppressed PTH secretion, PTH resistance) 2. Disorders of vitamin D metabolism (deficiency, resistance, increased metabolism, defective 25 or 1-alpha hydroxylation) 3. Ca deficiency (intake↓, excessive bone deposition, hypoproteinemia, chelation and medicines) 4. Critical illness (pancreatitis, toxic shock syndrome, etc.) Clinical manifestations 1. Increased neuromuscular irritability → cramping, carpopedal spasm, Chvostek sign, paraesthesias, laryngospasm, abdominal cramping and hyperreflexia. 2. CNS disturbances: seizures, psychosis, impaired memory & extrapyramidal system dysfunction, basal ganglia calcification (in chronic cases). 3. Ocular: cataract (in chronic hypocalcemia), papilledema and pseudotumor cerebri. 4. Cardiovascular: prolonged QT, in chronic severe cases refractory congestive heart failure. 5. Soft tissue calcifications 6. Macrocytic megaloblastic anemia. Infants may also be lethargic, feed poorly an jittery. Management 1. IV 10% calcium gluconate (1mg/Kg) slowly infused with constant cardiac monitoring. 2. Following step 1 IV Ca infusion of 50-75 elemental Ca/Kg /day until serum concentration is corrected. Maintenance thereafter is by oral Ca with vitamin D. HYPOGLYCEMIA HYPOGLYCEMIA IN TYPE 1 DIABETES Definition: blood glucose level <50mg% Clinical features: weakness, sweating, hunger, nausea, vomiting, headache, abdominal pain, visual disturbances, confusion, difficulty in speech and thinking, shakiness, tachycardia, irritability, restlessness, bizarre behavior. Causes for hypoglycemia: 1. Skipping a meal 2. Excess insulin (inadvertent or on purpose) 3. Intensive physical exercise without adjustment of insulin dose and carbohydrate intake. 9 4. “Honeymoon” 5. Acute intercurrent illness associated with low carbohydrates intake. 6. Alcohol consumption (inhibits gluconeogenesis) 10 Management Mild hypoglycemia – drink juice or eat simple carbohydrate. Moderate hypoglycemia – administer glucose gel or honey on buccal mucosa. Severe hypoglycemia – 1. IM/SC glucagon. 2. IV glucose bolus 0.5 gr/Kg (10% glucose or 25% maximal concentration, followed by 10% glucose infusion(x1.5 maintenance) HYPOGLYCEMIA IN NEONATES AND INFANTS Definition: preterm (older than 24 hours) –glucose < 40 mg% Term (older than 24 hours) – glucose < 50 mg% Symptoms: Cyanotic episodes Apnea Respiratory distress Refusal to feed Brief myoclonic jerks Wilting spells Convulsions Somnolence Subnormal temperature Sweating Blood samples should be taken during hypoglycemia for work up “critical sample” Management 1. IV glucose 10% bolus 2ml/Kg followed by continuous infusion of glucose at a rate of 8 mg/Kg/min. 2. If glucose is not sufficient: IV hydrocortisone 2.5 mg/Kg every 6 hours. HYPOGLYCEMIA IN CHILDREN AND ADOLECENTS Definition: glucose < 50% Symptoms: As mentioned above. Causes: 1. Prolonged fasting, ketotic hypoglycemia, severe malnutrition. 2. Acute infection, severe diarrhea 3. Hormone deficiencies: GH, cortisol, thyroxine, panhypopituitarism. 4. Insulinoma 5. Non insulin secreting tumors. “Big IGF-2”, mostly with mesenchymal tumors. 6. Inborn errors of metabolism. 7. Administration of insulin or oral hypoglycemic. 8. Salicylates or ethanol overdose. Critical sample should be taken during hypoglycemia ! Management: As above. 11 12