III. System Biology Approach To Atherosclerosis
advertisement
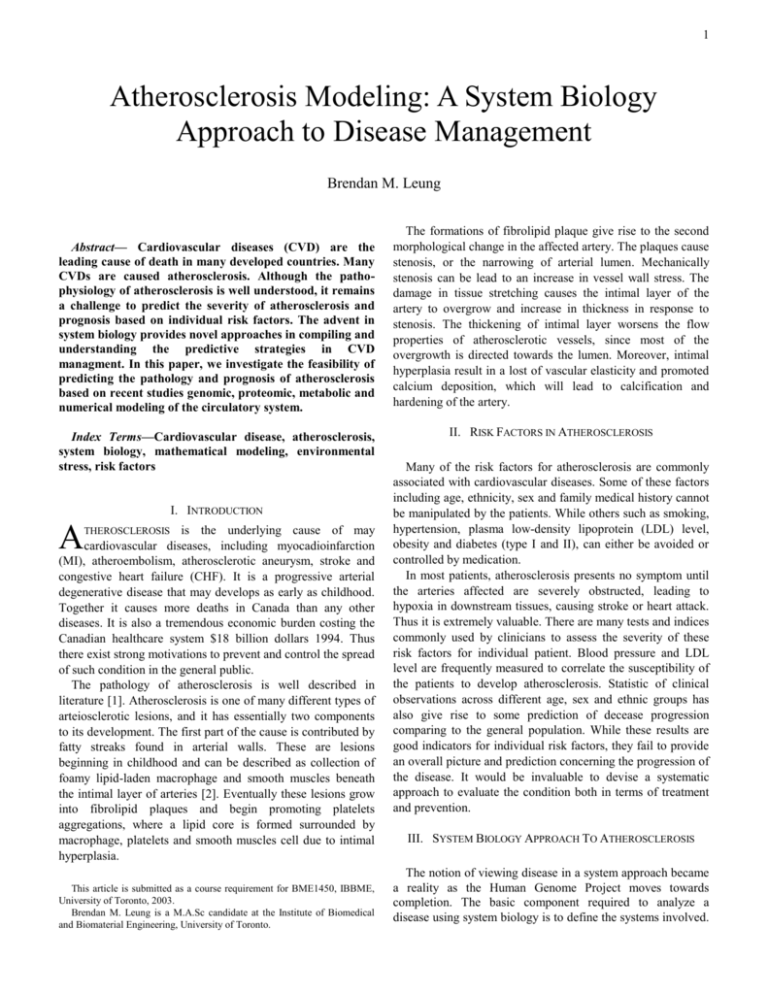
1 Atherosclerosis Modeling: A System Biology Approach to Disease Management Brendan M. Leung Abstract— Cardiovascular diseases (CVD) are the leading cause of death in many developed countries. Many CVDs are caused atherosclerosis. Although the pathophysiology of atherosclerosis is well understood, it remains a challenge to predict the severity of atherosclerosis and prognosis based on individual risk factors. The advent in system biology provides novel approaches in compiling and understanding the predictive strategies in CVD managment. In this paper, we investigate the feasibility of predicting the pathology and prognosis of atherosclerosis based on recent studies genomic, proteomic, metabolic and numerical modeling of the circulatory system. Index Terms—Cardiovascular disease, atherosclerosis, system biology, mathematical modeling, environmental stress, risk factors I. INTRODUCTION A is the underlying cause of may cardiovascular diseases, including myocadioinfarction (MI), atheroembolism, atherosclerotic aneurysm, stroke and congestive heart failure (CHF). It is a progressive arterial degenerative disease that may develops as early as childhood. Together it causes more deaths in Canada than any other diseases. It is also a tremendous economic burden costing the Canadian healthcare system $18 billion dollars 1994. Thus there exist strong motivations to prevent and control the spread of such condition in the general public. The pathology of atherosclerosis is well described in literature [1]. Atherosclerosis is one of many different types of arteiosclerotic lesions, and it has essentially two components to its development. The first part of the cause is contributed by fatty streaks found in arterial walls. These are lesions beginning in childhood and can be described as collection of foamy lipid-laden macrophage and smooth muscles beneath the intimal layer of arteries [2]. Eventually these lesions grow into fibrolipid plaques and begin promoting platelets aggregations, where a lipid core is formed surrounded by macrophage, platelets and smooth muscles cell due to intimal hyperplasia. THEROSCLEROSIS This article is submitted as a course requirement for BME1450, IBBME, University of Toronto, 2003. Brendan M. Leung is a M.A.Sc candidate at the Institute of Biomedical and Biomaterial Engineering, University of Toronto. The formations of fibrolipid plaque give rise to the second morphological change in the affected artery. The plaques cause stenosis, or the narrowing of arterial lumen. Mechanically stenosis can be lead to an increase in vessel wall stress. The damage in tissue stretching causes the intimal layer of the artery to overgrow and increase in thickness in response to stenosis. The thickening of intimal layer worsens the flow properties of atherosclerotic vessels, since most of the overgrowth is directed towards the lumen. Moreover, intimal hyperplasia result in a lost of vascular elasticity and promoted calcium deposition, which will lead to calcification and hardening of the artery. II. RISK FACTORS IN ATHEROSCLEROSIS Many of the risk factors for atherosclerosis are commonly associated with cardiovascular diseases. Some of these factors including age, ethnicity, sex and family medical history cannot be manipulated by the patients. While others such as smoking, hypertension, plasma low-density lipoprotein (LDL) level, obesity and diabetes (type I and II), can either be avoided or controlled by medication. In most patients, atherosclerosis presents no symptom until the arteries affected are severely obstructed, leading to hypoxia in downstream tissues, causing stroke or heart attack. Thus it is extremely valuable. There are many tests and indices commonly used by clinicians to assess the severity of these risk factors for individual patient. Blood pressure and LDL level are frequently measured to correlate the susceptibility of the patients to develop atherosclerosis. Statistic of clinical observations across different age, sex and ethnic groups has also give rise to some prediction of decease progression comparing to the general population. While these results are good indicators for individual risk factors, they fail to provide an overall picture and prediction concerning the progression of the disease. It would be invaluable to devise a systematic approach to evaluate the condition both in terms of treatment and prevention. III. SYSTEM BIOLOGY APPROACH TO ATHEROSCLEROSIS The notion of viewing disease in a system approach became a reality as the Human Genome Project moves towards completion. The basic component required to analyze a disease using system biology is to define the systems involved. 2 Table 1: Sources and databases of cardiovascular transcriptome and proteome In the case of atherosclerosis, there are two related system that needs to be identified. The first system is the disease pathology. It was mentioned previously that the make up of the disease fairly is well described as far as the types of cells involved and pathology is concerned. The second system of interest is the human system in which the disease lies. The genes that make up various components of the human system are currently being uncovered by the Human Genome Project. Their functions will also be elucidated by proteomic studies following the post-genomic era. Functional analysis gives rise to metabolic pathways which generate the basis for normal physiology and pathophysiology comparison. In essence, we can consider the disease model for atherosclerosis as two systems, one with in another. The power of incorporating the human genome into the modeling process means that personalized predictions can be made given the state of the individual as measured using existing parameters such as blood cholesterol level, blood pressure and life styles. A. Systemic Modeling Once the systems involved are defined, we can define the parameters that interact and perturb the system. As mentioned previously, some risk factors in atherosclerosis are related to the human system, such as age, sex and ethnicity. Attempts has been made to models the effect these factors on the cardiovascular system. The effect to aging is probably the most studied systemic cause of atherosclerosis. Non-disease specific mathematical modeling on aging has been attempted [3-4]. Although the results from these studies are invaluable toward the understanding of systemic aging, models that deal more specifically with organ degeneration is needed as a disease prediction tool. The first step in creating such model is to elucidate tissue specific gene expression pattern, so-call tissue transcriptome, similar to that done in BodyMap Database for cardiac myocyte and aortic tissue [5]. Natural it would also be of interest to understand the tissue proteome, the protein expression pattern. Some databases containing cardiovascular gene and protein expressions are listed in Table 1 [6]. Building on the knowledge of genomics and proteomic, the physiology of the cardiovascular system may be incorporated. One such study attempted to model the normal physiology of cardiomyocyte based on the DiFrancesco-Noble model of the Purkinje fiber [6], derived from the Hodgkin-Huxley model of the squid axon form the 60’s. The model aims to create a virtual myocyte in which intra and extra cellular calcium level, membrane ionic potential, membrane transport proteins and bioenergetics via the tricarboxylic acid cycle (a.k.a. Krebs cycle) are all taken into consideration in cellular function and contraction. Such model has been validated and used to model normal versus disease state myocytes. An even more ambitious attempt was made by Hunter et al. [7] from the University of Auckland, New Zealand, where they combined the anatomy of the heart, electrical properties of membrane ionic channels, soft tissue theory described by mechanical elastic deformation equations, homodynamic models based on Navier-Stokes equations and metabolic 3 pathways of cardiomyocytes to generate an overall picture to describe a beating heart. The exploitation of knowledge from the vast number of bio-physical disciplines reiterates the complexity of biological systems. The resulting model was very comprehensive and was able to integrate the various submodels dealing different physical parameters such as stress, electrical potential, flow rate and metabolic state in a 3dimensional fashion using the large deformation mechanic model. B. Environmental Modeling While systemic modeling deals mainly with normal physiology and pathogenesis, environmental modeling takes into consideration the causal as well as degenerative effect of risk factors. While modern clinical practices focus on monitoring and controlling these risks in order to lower their impacts, it does not provide patients and clinicians with a predictive treatment due to the lack of understanding. In such case a model based on measurable risk factor such as blood pressure and plasma LDL level would be useful. While monitoring of arterial blood flow is not a common clinical “check-up” procedure, one may use blood pressure to relate the flow regime occurring in the arteries. However, popularization of non-invasive flow measurement techniques such as ultra-sound Doppler, laser Doppler anemometry and functional magnetic resonance imaging may allow for routine arterial flow monitoring. Perktold et al. have used numerical modeling to investigate local arterial flow conditions associated with atherosclerotic lesions [8]. It was hypothesized that hemadynamic is related to platelet aggregation and vessel wall modification. Platelets in regions of the arteries where turbulent whirls are found experience an increased resident time in contact with the endothelium, thus may promotes plaque formation and growth. Aortic cell morphology can be altered by wall shear stress, especially in regions where flow rate and direction changes with pulsate motion of the heart. Local flow pattern chances mass transfer properties of the endothelium, in turn, such vessel wall permeability and arterial mass transfer contributes to vessel wall shear stress and transendothelium macromolecules transport. The results may lead to intimalmedial remodeling, the first step observed in atherogenesis [9]. The modeling process relies on the basic engineering concepts in fluid mechanic. Blood was modeled as a incompressible, elastic non-Newtonian fluid, and a viscous flow equation was applied (Nanvier-Stokes). The use of computational fluid dynamic (CFD) allows for the identification of two types or near wall flow patters which are of interest in disease development. It can be seen here that system biology approach to disease modeling act as a discovery tool for basic pathogenesis and pathophysiology. Future modeling may also consider the elastic properties on aorta under pressure (current model assumes rigid wall). The effects of plasma cholesterol level on atherosclerosis were under intense investigation over the past two decades. However there remains to be limited effort in creating a computational model correlating cholesterol level and atherosclerosis. A study done by Nedeljkovic et al. [10] attempted to correlate intimal-medial thickening, a hallmark of atherosclerosis, with plasma triglyceride and cholesterol indices. The following mathematical relationship was observed: IMT = 0.005 x TG-0.008 x Chol + 0.28 where IMT, TG and Chol are intimal-medial thickening, triglyceride and cholesterol indices used in the study. While the model is empirical and by no mean transferable between populations, it does provide a basis to understand the impact current laboratory tests results on the disease state. As described before, the effects of blood cholesterol level maybe due in part to the transendothelial transport mechanism, which is heavily dependent on local flow condition. It was observed that mass transfer in the vicinity of stenosis and bifurcation are different that other areas of the arteries [11]. Modeling based on convective mass transport in arterial blood reveals a polarized boundary layer on the arterial wall with respect to LDL concentration, as illustrated on figure 1. The modeling data of LDL accumulation provides a better correlation between measured plasma LDL level and actual local surface LDL concentration. Figure 1: Polarization of LDL concentration at the vessel wall boundary layer as modeled using mass transfer equations. [13] Work done by Back et al. [12] shows that region distal to stenosis suffers hypoxia and increased LDL perfusion. The conceivable effect on stenotic plaque enlargement can be model using a combination of measured plasma LDL level and CFD analysis described before. IV. INTEGRATION OF MODELS: GENERATING A TOOL FOR DISEASE PREDICTION. Currently a unified model that incorporate systemic model and environmental model for the purpose of atherosclerosis progression prediction does not exist. However, gathering from the many advances in individual sciences concerned in vascular biology, it is a feasible and practical approach to develop diagnostic models for the treatment of atherosclerosis. Present clinical measurements 4 of blood pressure and plasma LDL levels may be incorporated into the combined model to predict the effective arterial wall surface cholesterol level and better assess the risk of progression of fibrolipid plaques. On the other hand, genomic and proteomic modeling of arterial aging may be included when modeling the hemadynamics in the patients’ arteries, hence giving a more accurate prediction of arterial wall LDL concentration mention above. To bring the disease modeling concept to an even more proactive level, one can imagine the long term arterial health modeling based on the measured parameters and the patients’ genomic make-up. The concept of preventive disease management may also be applied in other degenerative conditions and may provide vast benefit to public health. V. CONCLUSION The current paper put forth the idea of preventive medicine using a system biology approach to devise models that reflect the state of health of patients’ arteries. The advents in numerical modeling and genomic / proteomic discoveries allows for sophisticated models to be developed, thus the unification of models as a diagnostic tool is deemed both feasible and practical. REFERENCES [1] Herbert C. Stary, Atlas of Atherosclerosis Progression and Regression 2nd ed. April 2003, CRC Press. [2] University of Alberta, Faculty of Medicine and Dentistry, Department of Laboratory Medicine and Pathology course website http://www.med.ualberta.ca/lmp/000p0058.htm [3] Kirkwood TB, Boys RJ, Gillespie CS, Proctor CJ, Shanley DP, Wilkinson DJ, Towards an e-biology of ageing: integrating theory and data, Nat Rev Mol Cell Biol. 2003 Mar;4(3):243-9 [4] Edelstein-Keshet L, Israel A, Lansdorp P, Modelling perspectives on aging: can mathematics help us stay young?, J Theor Biol. 2001 Dec 21;213(4):509-25. [5] Human and Mouse Gene Expression Database. BodyMap, http://bodymap.ims.u-tokyo.ac.jp [6] Raimond L. Winslow, Genomic Informatic: Current Status and Future Prospect, Circ Res 2003,92:953-961 [7] PJ. Hunter, AJ Pullan, BH Smaill, Modeling Total Heart Function, Annual Review of Biomedical Engineering, Aug 2003, Vol. 5, pp. 147177 [8] K Perktold, G. Rappitsch, Mathematical modeling of arterial blood flow and correlation to atherosclerosis, Technology and Health Care 3 (1995) 139-151 [9] Fitzgerald et al., Atheroma and arterial wall shear: observation, correlation and proposal of a shear dependent mass transfer mechanism in atherosclerosis., Proc. Roy. Soc. Lond. (1971) 177: p. 109-159 [10] Nedeljkovic M, Petrovic B, Djuric D., A mathematical model for prediction of the effect of hyperlipidemia on thickness of the intimamedia complex in the carotid artery wall as an indicator of atherosclerosis, Srp Arh Celok Lek. 2002 Sep-Oct;130(9-10):301-5 [11] Ethier CR, Computational modeling of mass transfer and links to atherosclerosis., Ann Biomed Eng. 2002 Apr;30(4):461-71 [12] Back, L. H., J. R. Radbill, and D. W. Crawford. Analysis of oxygen transport from pulsatile viscous blood flow to diseased coronary arteries of man. J. Biomech. 10:763–774, 1977. [13] Wada, S., and T. Karino. Theoretical study on flow-dependent concentration polarization of low density lipoproteins at the luminal surface of a straight artery. Biorheology 36:207–223, 1999.