Answers to Review Questions
advertisement

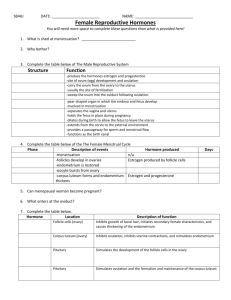
This study aid was based solely off of lecture notes (Embryological Sex Differentiation through Anatomy). Fill in the blanks with the most correct word answers OR circle the correct answer out of two choices. Good luck! 1. Each stage of determination of biological sex is INDEPENDENT of the others. 2. UNDIFFERENTIATED structures that can develop in either the female or male direction are ALWAYS AVAILABLE. 3. The current biological environment DETERMINES the path taken at each stage. 4. The same path DOES NOT have to be taken at each stage. 5. The first stage of biological sex determination occurs on the level of CHROMOSOMAL sex, the second stage pertains to GONADAL sex, the third stage involves the development of INTERNAL GENITALIA, and the fourth stage has to do with the development of EXTERNAL GENITALIA. 6. Typically humans have 23 pairs of chromosomes, one pair of which are SEX chromosomes that are gender specific. The typical human male’s chromosome complement is XY and the typical human female’s XX, but many other chromosome complements can occur. 7. A sperm carrying an X chromosome is LARGER than a sperm carrying a Y chromosome. This is because X chromosomes carrying MORE genetic information than Y chromosomes. 8. Some individuals have only one sex chromosome. When this is the case, the sex chromosome must be an X, which is represented as the XO sex chromosome complement. These individuals CANNOT reproduce. One the other hand, the sex chromosome complement YO cannot survive. 9. An individual with only one sex chromosome is diagnosed with a disorder called TURNER SYNDROME. This occurs due to fertilization of the ovum by a sperm that has NO sex chromosome. These individuals are identified as FEMALE at birth. 10. Individuals with the disorder mentioned above DO NOT develop functional ovaries. At puberty, she DOES NOT develop female SECONDARY sex characteristics because there is no source of estrogen. These individuals typically receive estrogen treatment to stimulate FEMALE development. 11. On the other hand, some individuals are born with more than 2 sex chromosomes. The greater the number of sex chromosomes the LESS likely the combination will occur, the MORE likely the individual will have NON-SEX-RELATED chromosomal differences. 12. Gonads are structures that produce reproductive cells (ova in females and sperm in males). They begin to sex differentiate about six weeks after conception. 13. Undifferentiated gonads have two parts: the cortex and the medulla, which develop into ovaries and testes, respectively. All developing individuals have both, meaning they are bipotential. 14. At three weeks the primordial germ cells begin to migrate from the yolk sac to the site of the undifferentiated gonad. 15. Primordial Germ Cells (PGCs) are the earliest form of ALL the ova a female will ever possess. 16. The development of testes in males requires: the presence of a functional Y chromosome. 17. A functional Y chromosome has a(n) SRY gene that STIMULATES a non-sex chromosome (also know as a(n) autosome) to produce H-Y antigen, which stimulates the development of the medulla of the undifferentiated gonads to develop into testes, while the cortex fades away. 18. The development of ovaries in females require: the migration of the PGCs to the undifferentiated gonads, the absence of a functional Y chromosome, and the presence of at least 2 functional X chromosomes. Upon meeting these requirements, the cortex of the undifferentiated gonads develops into ovaries, while the medulla fades away. 19. The presence of any functional Y chromosome ALWAYS results in the development of testes REGARDLESS OF how many X chromosomes are present. 20. Male internal genitalia include: seminal vesicles, epididymus, and the ejaculatory ducts and tubes. Female internal genitalia include: uterus, oviducts (also known as the Fallopian tubes), and vagina. 21. At eight weeks, BOTH / EITHER the Wolffian ducts and/or Mullerian ducts are found in all developing individuals REGARDLESS OF / DEPENDING ON the paths taken in Stages 1 and 2. 22. Development of male internal genitalia requires: androgens, Mullerian Inhibiting Factor, and inductor substance. All three of these required substances are produced by the testes and stimulate the development of Wolffian ducts into male internal genitalia, while causing the Mullerian ducts to regress. 23. The development of female internal genitalia requires ABSENCE of: androgens, Mullerian Inhibiting Factor, and inductor substance. When these three criteria are met the Mullerian ducts develop into female internal genitalia and the Wolffian ducts regress. 24. In the fourth stage, the undifferentiated raw materials that develop into external genitalia are: genital tubercle, labio-scrotal swelling, and uro-genital fold. They are found in all developing individuals regardless of sex chromosomes, gonads, or internal genitalia. 25. Androgens (normally from the fetus’ testes) result in male development of the undifferentiated structures. The male penis is formed from the genital tubercle, the scrotal sac (or scrotum) from the labio-scrotal swelling, and the urethra from the uro-genital fold. 26. If androgens are not produced or the fetus cannot react to it, the undifferentiated structures develop into female external genitalia. The clitoris is formed from the genital tubercle, the labia majora from the labio-scrotal swelling, and the labia minora from the uro-genital fold. 27. Androgen Insensitivity Syndrome (AIS) occurs when an individual lacks receptors that respond to androgens. Such individuals have an XY sex chromosome complement, NORMAL testes, AMBIGUOUS internal genitalia, and FEMALE external genitalia. They are typically raised as FEMALES and have a FEMALE gender identity. 28. Congenital Adrenal Hyperplasia (CAH) occurs when there is an excess of androgens due to a malfunction of the adrenal gland. Effects vary with when the increased androgen starts and how high the levels are. It may result in ambiguous INTERNAL genitalia and masculinized external genitalia in an XX individuals with OVARIES. 29. The two jobs of ovaries are to: house immature ova and provide space for ova to mature and hormone production. 30. The first half of the monthly cycle runs from the first day of menses (Day 1) to ovulation. The two halves ARE NOT NECESSARILY equal in duration. 31. The first half of the cycle is referred to by three names: Preovulatory Phase (which refers to time), Follicular Phase (which refers to what is happening in the ovaries), and Proliferative Phase (which refers to what is happening in the uterus) is also used but does not refer to the same timeframe as the other two terms. 32. The second half of the cycle is referred to by three names as well, they are: Postovulatory Phase (referring to time), Luteal Phase (referring to what is happening in the ovaries), and Secretory Phase (referring to what is happening in the uterus). . 33. The length of the second half of the cycle is RELATIVELY FIXED, while length of the first half MAY CHANGE from month-to-month. The length of the SECOND half of the monthly cycle is 14 + 2 days. 34. A female has the greatest number of immature ova at 20 weeks POST-conception, after which the number DECREASES AND GETS DOWN INTO THE HUNDREDS AT MENOPAUSE. 35. In the preovulatory phase MANY ovum/ova begin to mature but most quickly die off. During this part of the cycle, the ovum that is “selected” to mature and be released at ovulation INCREASES in size, and there is an INCREASE in BOTH THE NUMBER AND THE SIZE of the follicular cells. 36. During the preovulatory phase, the hormone-producing site is the Ovarian Follicle (also know as the Graafian Follicle). The hormones produced are (list the most prominent hormone first): estrogen (estradiol), androgen, and inhibin. 37. Ovulation is defined as the rupturing of the Graafian follicle and release of the ovum. The peak-like shape that the follicle takes on before it ruptures is called a stigma. 38. Mittelschmerz, which directly translated means “middle pain”, occurs when blood released at ovulation irritates other surrounding organs. 39. The substances released at ovulation are the follicular fluid, ovum, corona radiata, and sticky cumulus. The corona radiata provides nutrients for the ovum from ovulation until the ovum is inside the oviduct. The sticky cumulus is a sticky layer of cells that surrounds the ovum and the corona radiata which helps with the transport of the ovum INTO AND THROUGH the oviduct. 40. During the postovulatory phase, the hormone producing site is the corpus luteum which is formed from old cells remaining after ovulation and produces (list in order of prominence): progesterone, estradiol, androgens, and inhibin. This hormone producing site has a lifespan of 14 + 2 days unless the ovum is fertilized, in which case it stays active throughout the duration of the pregnancy. Once it has died, it becomes the corpus albicans. 41. The hormone Progesterone is only found in the second half of the monthly cycle. 42. The path which the released ovum follows to get to the uterus is as follows: ovary fimbria ampulla isthmus uterus. 43. Upon reaching the oviduct, the corona radiata no longer provides nutrition for the ovum, rather the cells lining the lumen of the oviduct provide nutrition. 44. The Isthmus is the part of the oviduct that is CLOSEST TO the uterus and has much THICKER walls than the ampulla, meaning that the inside opening of the tube (called the lumen) is smaller. 45. When the ovum reaches the ampulla-isthmus junction, the oviduct contracts in front of and behind it trapping the ovum for 2 to 2.5 days. This is the typical place for fertilization to occur. 46. After ovulation, the ovum is most suitable for fertilization for 24 hours. Sperm can stay alive for 3 days in a woman. 47. An ectopic pregnancy occurs any time implantation and development of a fertilized ovum takes place anywhere other than the upper 2/3 of the uterus. When this occurs, it is most commonly in the oviduct. 48. The fundus is the part of the uterus, where implantation typically occurs, it is located at the very top of the uterus. The cervix is the narrow portion of the bottom of the uterus. The cervical os is the opening from the cervix into the vagina. 49. Cells lining the cervix produce cervical mucus which changes depending on which hormones are present. When estrogen is high (around the time of ovulation), the cervical mucus becomes thin/wet/slippery/stringy, while when it is low or there is high levels of progesterone, the cervical mucus is dry/sticky. 50. Menstrual fluid consists of blood, glandular secretions from endometrial cells, the dead unfertilized ovum and fragments from the disintegrating endometrial cells. 51. During the Proliferative Phase, which runs from the end of menses to ovulation, endometrial cells INCREASE in size and number; while during the Secretory Phase, which runs from ovulation until Day 1 of the next cycle, the endometrial cells fill with fats and glycogen. 52. There are FEW nerve endings in the vagina. The cervix has FEW nerve endings. 53. Fornices are located at the top of the vagina near the cervix. They serve as shock absorbers and pooling places for semen and sperm. 54. The vulva is the visible external genitalia of a female. The mons veneris/mons pubis is at the front. Here skin, fat and connective tissue overlie the pubic bone. The perineum is at the back located between the vaginal opening and the anus and has many nerve endings. The labia majora are at the lateral (side) borders and have many sweat and sebaceous glands on their inner surfaces that make the area waterproof and protect from urine crystallization and blood clots. It has characteristics similar to the scrotal sac. 55. Endometriosis occurs when endometrial cells grow outside the fundus and undergo the same changes as the cells that should be found in the uterus. 56. The Bulbs of Vestibule are spongy, specialized erectile tissue inside the labia majora. The Glands of Bartholin have ducts/tubes that open right inside the vagina. They were originally thought to be the major source of vaginal lubrication during sexual excitement, which was later DISPROVED by Masters and Johnson. It is now believed that they play a small role on vaginal lubrication during sexual excitement 57. The labia minora meets at the front to form the prepuce (or hood) of the clitoris. The labia minora DO NOT HAVE specialized erectile tissue but have venous spaces that engorge with blood during sexual excitement. 58. The area of the vulva located under the labia minora is called the Vestibule. It includes the following structures: clitoris, urethral opening, vaginal opening, hymen, and Glands of Bartholin. 59. The clitoris is MORE sensitive to touch than the penis because of its HIGH concentration of nerves. 60. The urethral opening is where urine leaves the body. A female urethra is SHORTER than the male urethra, making them MORE susceptible to bladder/urinary tract infections. However, bladder infections in women are LESS serious than in men. 61. The hymen is the membranous covering over the vaginal opening. It differs in structure from woman to woman. 62. The clitoris extends into the body and has crura or legs that pass on either side of the urethra and vagina. During sexual excitement it PULLS BACK. It contains erectile tissue called the corpora cavernosa. 63. Prior to puberty breasts in females and males are THE SAME; they respond to hormones in THE SAME ways. 64. The suspensory ligaments connect the breast to the pectoral muscle. Differences in the amount of adipose tissue (fat) and connective tissue determine differences in breast size. The area near the nipple that is pigmented is called the areola. The areolae have Montgomery glands which are important during breast feeding as they lubricate the nipple and secrete an anti-bacterial that reduces the risk of infection. 65. The Mammary glands are the milk producing and transport structures in the breast. The sinuses are the wider areas of the ducts right near the nipple. Milk is produced in the alveoli. The lobes and lobules are ducts that transport the milk to the nipple for release from the breast. 66. With every monthly cycle the amount of mammary gland tissue INCREASES. The vast majority of alveoli are located at the sides of the breasts close to the underarm area.