Circulation Qs
advertisement
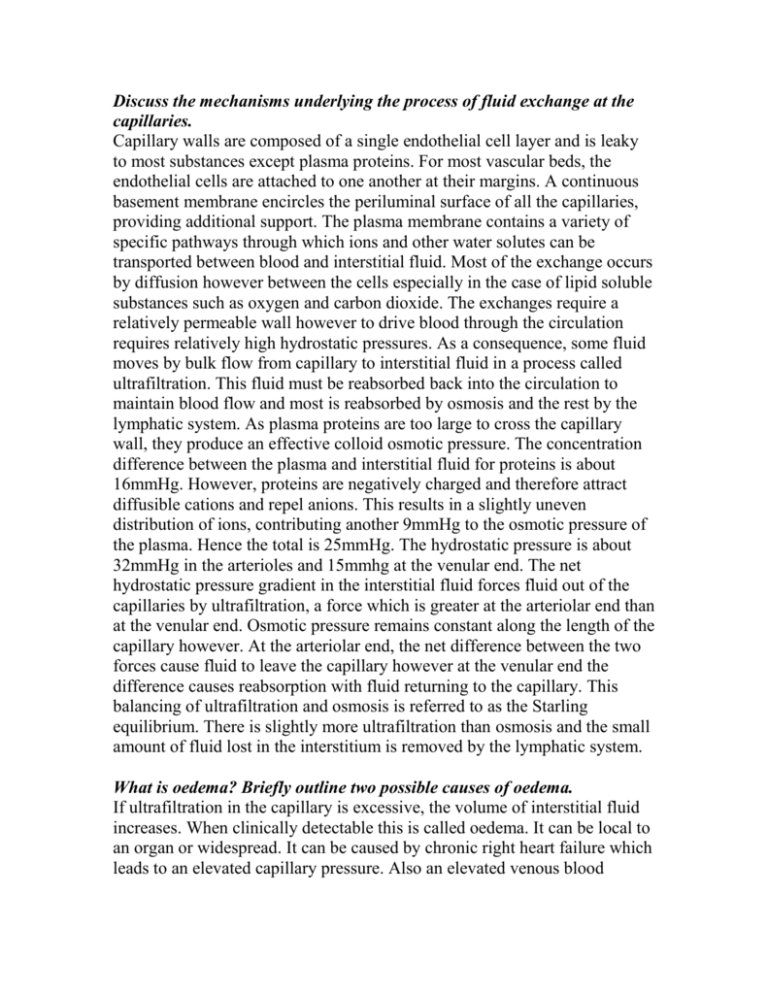
Discuss the mechanisms underlying the process of fluid exchange at the capillaries. Capillary walls are composed of a single endothelial cell layer and is leaky to most substances except plasma proteins. For most vascular beds, the endothelial cells are attached to one another at their margins. A continuous basement membrane encircles the periluminal surface of all the capillaries, providing additional support. The plasma membrane contains a variety of specific pathways through which ions and other water solutes can be transported between blood and interstitial fluid. Most of the exchange occurs by diffusion however between the cells especially in the case of lipid soluble substances such as oxygen and carbon dioxide. The exchanges require a relatively permeable wall however to drive blood through the circulation requires relatively high hydrostatic pressures. As a consequence, some fluid moves by bulk flow from capillary to interstitial fluid in a process called ultrafiltration. This fluid must be reabsorbed back into the circulation to maintain blood flow and most is reabsorbed by osmosis and the rest by the lymphatic system. As plasma proteins are too large to cross the capillary wall, they produce an effective colloid osmotic pressure. The concentration difference between the plasma and interstitial fluid for proteins is about 16mmHg. However, proteins are negatively charged and therefore attract diffusible cations and repel anions. This results in a slightly uneven distribution of ions, contributing another 9mmHg to the osmotic pressure of the plasma. Hence the total is 25mmHg. The hydrostatic pressure is about 32mmHg in the arterioles and 15mmhg at the venular end. The net hydrostatic pressure gradient in the interstitial fluid forces fluid out of the capillaries by ultrafiltration, a force which is greater at the arteriolar end than at the venular end. Osmotic pressure remains constant along the length of the capillary however. At the arteriolar end, the net difference between the two forces cause fluid to leave the capillary however at the venular end the difference causes reabsorption with fluid returning to the capillary. This balancing of ultrafiltration and osmosis is referred to as the Starling equilibrium. There is slightly more ultrafiltration than osmosis and the small amount of fluid lost in the interstitium is removed by the lymphatic system. What is oedema? Briefly outline two possible causes of oedema. If ultrafiltration in the capillary is excessive, the volume of interstitial fluid increases. When clinically detectable this is called oedema. It can be local to an organ or widespread. It can be caused by chronic right heart failure which leads to an elevated capillary pressure. Also an elevated venous blood pressure as occurs in the lower limbs when in the standing position can be enough to cause oedema in some people. What major changes occur in blood flow distribution during strenuous exercise? How are these changes produced? At the onset of exercise, signals are transmitted not only from the brain to the muscles to cause muscle contraction but also into the vasomotor center to initiate mass sympathetic discharge throughout the body. Simultaneously, the parasympathetic signals to the heart are attenuated. Therefore, three major circulatory effects result. First, the heart is stimulated to greatly increased heart rate and increased pumping strength as a result of the sympathetic drive to the heart plus release of the heart from normal parasympathetic inhibition. Second, most of the arterioles of the peripheral circulation are strongly contracted, except for the arterioles in the active muscles, which are strongly vasodilated by the local vasodilator effects in the muscles by acetylcholine secreting sympathetic fibers. Thus, the heart is stimulated to supply the increased blood flow required by the muscles, while at the same time blood flow through most nonmuscular areas of the body is temporarily reduced, thereby temporarily "lending" their blood supply to the muscles. This accounts for as much as 2 L/min of extra blood flow to the muscles, which is exceedingly important when one thinks of a person running for his life-even a fractional increase in running speed may make the difference between life and death. Two of the peripheral circulatory systems, the coronary and cerebral systems, are spared this vasoconstrictor effect because both these circulatory areas have poor vasoconstrictor innervation-fortunately so because both the heart and the brain are as essential to exercise as are the skeletal muscles. Third, the muscle walls of the veins and other capacitative areas of the circulation are contracted powerfully, which greatly increases the mean systemic filling pressure. This is one of the most important factors in promoting increase in venous return of blood to the heart and, therefore, in increasing the cardiac output. Describe the mechanisms underlying intrinsic control of blood flow in the vasculature. Many organs demonstrate the phenomenon of autoregulation. This means that despite large changes in perfusion pressure the blood flow remains remarkably constant. This is determined to be a result of the response of the arteriolar smooth muscle to stretch and local metabolites. According to the law of Laplace, the smooth muscle of arterioles contracts when its wall tension is passively increased and relax when the pressure decreases. Increased wall tension opens calcium channels in the muscle and this increases the muscle tone. The reduction in radius matches the increase in perfusion pressure so that there is no change in blood flow. This is called myogenic autoregulation and does not occur in the skin. During increased metabolism there is a local decrease in the partial pressure of oxygen, an increase in the partial pressure of carbon dioxide and an increase in the H+ concentration in the interstitial fluid. These changes cause the smooth muscle to relax to a degree that is appropriate to the increased metabolism and ensure an increase in flow with little to no change in perfusion pressure. This called metabolic regulation or active hyperemia. Increases in temperature and in the concentrations of ATP, ADP, AMP, adenosine, inorganic phosphate, lactate and pyruvate as well as potassium concentration and interstitial osmolarity can also cause vasodilation. Nervous control is capable of over-riding metabolic regulation. Discuss the regulation of cerebral blood flow. Blood flow into the brain is fairly constant and does not change greatly with a changing pressure gradient. The brain receives 13% of the cardiac output, has a high O2 consumption and a large arteriovenous difference. However the distribution of the blood can be altered to allow for different activities in the brain e.g. thinking vs vision. Nervous control is not one of the key regulators of cerebral blood flow. There is sparse sympathetic innervation in the brain which has vasoconstrictor potential but has little effect when activated. The same is true for activating the vasodilator nerves which emerge from the Facial N (CNVII). The action of hormones is also determined to have little effect. The effects of oxygen partial pressure have been found to be more important. Below 50mmHg pO2 the cerebral arterioles become sensitive to the vasodilating effects of hypoxia. The main regulators of cerebral blood flow have been determined to be carbon dioxide and hydrogen ions. Carbon dioxide combines with water to form carbonic acid which can dissociate to hydrogen ions and bicarbonate. It has been discovered that a rise in the partial pressure of carbon dioxide leads to increased cerebral blood flow. This increase in pCO2 may cause the concentration of hydrogen ions to increase as the two are linked by the above reactions. Similarly, a decrease in pCO2 can cause a fall in cerebral blood flow probably due to a fall in hydrogen ion concentration. A reduced oxygen supply is accompanied by an increase in pCO2 and acidity, making the determining factor to be hypercapnia not hypoxia. Describe the changes that occur in the coronary circulation during exercise. The left and right coronary arteries emerge from the aortic sinuses. They each supply the myocardium of the atria and ventricles and also provide a blood supply to the SA and AV nodes. They flow into capillaries in the myocardium, drained by coronary veins which return blood into the right atrium via the coronary sinus. The heart receives 5% of the cardiac output and has a very high oxygen consumption. The relationship between coronary blood flow and the work of the heart is a linear one. That means that if one increases so does the other. The increase in coronary blood flow can be seen to be the result of two opposing forces. During the heart cycle, blood flow through the coronary circulation is seen to decrease during systole. The vessels are compressed during contraction and flow is particularly reduced in the left coronary artery. In diastole there is no compression and blood flow returns. In exercise, the heart rate is increased, tachycardia, and the cardiac contractility is also increased. Tachycardia reduces the diastolic filling time considerably and so less blood is able to reach the heart. The increased contractility means greater compression and thus less blood flow during systole. During increased cardiac activity, there is little further decrease in the venous oxygen content and the increased demand is satisfied by increased coronary blood flow. Hypoxia and adenosine are the main vasodilators of the coronary arteries and these are in high concentration during exercise. Thus although greater compression and shorter diastole in exercise act to reduce coronary blood flow, the metabolic regulation that occurs causes blood flow to increase during the diastolic period to supply the greater oxygen and thus blood demand. The last remaining effect which increases blood flow during exercise is increased potassium concentration in the extracellular fluid. Each time the muscle cell is excited by an action potential, the repolarization sees more potassium ions released into the ECF. These ions act as vasodilators and so increase the blood flow in the nearby coronary arteries. They have their greatest effect when the work of the heart is increased as in the case of exercise. Describe what happens to fluid movement across capillary walls when: (a) arterioles constrict; (b) plasma protein concentration is decreased.