Course Title: Newborn Risk Screening
advertisement

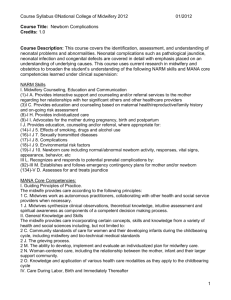
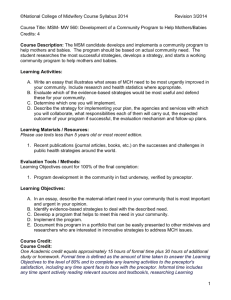
Course Syllabus ©National College of Midwifery 2012 01/2012 Course Title: Newborn Risk Screening Credits: 0.5 Course Description: This course provides an understanding of how to use information from the mother’s heath and reproductive history to assess the level of risk to the newborn. Fetal anomalies and problems at birth are examined to determine the impact they may have on the newborn. This course uses current research in midwifery and obstetrics to broaden the student’s understanding of the following NARM skills and MANA core competencies learned under clinical supervision: NARM Skills I. Midwifery Counseling, Education and Communication (1)-I A. Provides interactive support and counseling and/or referral services to the mother regarding her relationships with her significant others and other healthcare providers (3)I C. Provides education and counseling based on maternal health/reproductive/family history and on-going risk assessment (7)-I G. Applies the principles of informed consent (8)-I H. Provides individualized care (9)-I I. Advocates for the mother during pregnancy, birth and postpartum I J. Provides education, counseling and/or referral, where appropriate for: (13)-I J 4. Diet, nutrition and supplements (14)-I J 5. Effects of smoking, drugs and alcohol use (16)-I J 7. Sexually transmitted diseases (17)-I J 8. Complications (18)-I J 9. Environmental risk factors (19)-I J 10. Newborn care including normal/abnormal newborn activity, responses, vital signs, appearance, behavior, etc IV F. Assesses the condition of, and provides care for the newborn immediately after the birth by: (108)-IV F 2. Determining APGAR score VII. Well-Baby Care (149)-VII A. Provides well-baby care 2-6 weeks (150)-VII B. Assesses the general health and appearance of baby MANA Core Competencies: I. Guiding Principles of Practice. The midwife provides care according to the following principles: 1 H. Midwives recognize the empowerment inherent in the childbearing experience and strive to support women to make informed decisions and take responsibility for their own well-being. 1 J. Midwives synthesize clinical observations, theoretical knowledge, intuitive assessment and spiritual awareness as components of a competent decision making process. II. General Knowledge and Skills The midwife provides care incorporating certain concepts, skills and knowledge from a variety of health and social sciences including, but not limited to: 2 C. Community standards of care for women and their developing infants during the childbearing cycle, including midwifery and bio-technical medical standards and the rationale for and limitations of such standards 1 Course Syllabus ©National College of Midwifery 2012 01/2012 2 M. The ability to develop, implement and evaluate an individualized plan for midwifery care. 2 N. Woman-centered care, including the relationship between the mother, infant and their larger support community. 2 O. Knowledge and application of various health care modalities as they apply to the childbearing cycle IV. Care During Labor, Birth and Immediately Thereafter The midwife provides health care, support, and information to women throughout labor, birth and the hours immediately thereafter. She determines the need for consultation or referral as appropriate. The midwife uses a foundation of knowledge and/or skill which includes the following: 4 B. Parameters and methods for evaluating maternal and fetal well-being during labor, birth and immediately thereafter, including relevant historical data. 4 L. Understanding of and appropriate support for the newborn's transition during the first minutes and hours following birth. VI. Newborn Care The entry-level midwife provides health care to the newborn during the postpartum period and support and information to parents regarding newborn care. She determines the need for consultation or referral as appropriate. The midwife uses a foundation of knowledge and/or skill which includes the following: 6 A. Anatomy, physiology and support of the newborn’s adjustment during the first days and weeks of life 6 B. Parameters and methods for evaluating newborn wellness including relevant historical data and gestational age. 6 C. Nutritional needs of the newborn. 6 D. Community standards and state laws regarding indications for, administration of, and the risks and benefits of prophylactic bio-technical treatments and screening tests commonly used during the neonatal period. 6 E. Causes of, assessment of, appropriate treatment and emergency measures for neonatal problems and abnormalities. Learning Activities: A. Student reads appropriate sections from the Learning Materials/Resources. B. Student answers the questions listed in the Learning Objectives by researching the Learning Materials/Resources for the course and correctly cites the sources and page numbers for each of their answers. C. Student presents answers the questions listed in the Learning Objectives for review by preceptor. D. Student participates in preceptor elaboration/discussion of Learning Objectives. E. In the case that the required texts are more than 5 years old, the student must research, prepare & present a summary of current best midwifery care/practices appropriate to a topic covered in this course from a current journal article/study, less than 5 years old. 2 Course Syllabus ©National College of Midwifery 2012 01/2012 F. Recommended Role-playing and/or Clinical Interactions Note: The clinical requirement of NARM /Clinical Skills is completed at any time throughout the ASM apprenticeship during actual clinical practice and is NOT a requirement to complete this academic course. Activities specific to NARM skills learned in this section: 1. Attend a case review or peer review with a group of midwives. Discuss potential risks to the neonate based on the client’s history being discussed. 2. Observe a neonatal nurse practitioner or neonatologist on rounds at a neonatal intensive care unit. Listen for reviews of the mother’s history and how it may relate to the care of the newborn patient. 3. Create a handout for pregnant clients on the dangers of smoking in pregnancy. 4. Create a handout for clients on herpes simplex virus and its attendant risks for pregnant women and their newborns. 5. Create a handout on diabetes during pregnancy. Role play educating the client about risks to the newborn for diabetes in pregnancy. 6. Create a handout on genetic screening in pregnancy. Role play educating the client about risks of chromosomal abnormalities in pregnancy depending on her age, and risks and benefits of testing for her informed consent. 7. Create a handout on circumcision. Role play educating the client on her options for circumcision. Include potential risks and benefits for informed consent. 8. Role play educating the client about cytomegalovirus in pregnancy, including testing offered and information about the risks of CMV to the fetus. Learning Materials / Resources: Please use textbooks less than 5 years old or most recent edition. 1. Thureen, et al. Assessment and Care of the well newborn. 2nd ed. Elsevier Saunders. 2005. 2. Fraser, DM, et al. Myles Textbook for Midwives. 15th ed. Churchill Livingstone Press. 2009. 3. Varney, Helen. Varney’s Midwifery. Fourth Edition. Jones and Bartlett Publishers. 2004 3 Course Syllabus ©National College of Midwifery 2012 01/2012 rd 4. F. Cunningham, et al. William’s Obstetrics. 23 Edition. McGraw-Hill Professional. 2009. 5. Frye, Anne. Holistic Midwifery: A Comprehensive Textbook for Midwives in Homebirth Practice, Vol. 2: Care of the Mother and Baby from the Onset of Labor Through the First Hours After Birth. Labrys Press. 2004. th 6. Weaver, Pam and Evans, Sharon K. Practical Skills Guide for Midwifery, 4 Edition. Morningstar Publishing Co. Wasilla. 2007. 7. MEAC Abbreviated NARM Skills Form. 8. MANA Core Competencies for Midwives 9. Midwives Model of Care®. 10. Students must find 1 article/study less than 5 years old. Recommended internet links as needed for latest developments in midwifery care: The Cochrane Collaboration EBSCO National Library of Medicine PubMed Medline SCIRUS Medscape World Health Organization Evaluation Tools / Methods: Minimum passing grade for each course is a cumulative 80% / B-. Students and preceptors are encouraged to work together until the student masters the information. Final grade for the course is based on preceptor evaluation of the following: A. Learning Objectives count for 80-90% of the final grade. The preceptor evaluates each answer based on three elements: 1. Answers should reflect a thorough review of current literature regarding best current practices in midwifery care. 2. Each answer should be formed in the student’s own words or paraphrased from the text. The answer should be minimal, not a re-write of the entire text, but enough to show appropriate comprehension of the learning objective. 3. Student identification of sources and page numbers for each of the Learning Objectives. (Preceptor should do a random check to determine that sources cited are correctly identified.) 4 Course Syllabus ©National College of Midwifery 2012 01/2012 B. Summary of current journal article / study counts for 10% of the final grade in the case that other scholarly resources used are more than five years old. C. Exam counts for 10% of the final grade. Course credit: One Academic credit equals approximately 15 hours of formal time plus 30 hours of additional study or homework. Formal time is defined as the amount of time taken to answer the Learning Objectives to the level of 80% and to complete any learning activities to the preceptor's satisfaction, including any time spent face to face with the preceptor. Informal time includes any time spent actively reading relevant sources and textbook/s, researching Learning Objectives, and studying for examinations. Learning Objectives: A. The student must research, prepare & present a summary of an aspect of current best midwifery care/practices appropriate a topic from this course from a current journal article/study. B. Student answers the questions below and cites the sources and page numbers. 1. Explain why perinatal deaths are more often associated with a combination of adverse maternal history and/or conditions contributing to an adverse fetal environment rather than by any single adverse condition. 2. Explain why a previous pregnancy that ended in fetal mortality or morbidity contributes to increased risk to the present pregnancy. 3. Explain how maternal age may affect fetal risk status. 4. Discuss how pregnancy induced hypertension can increase risk for the neonate. 5. Explain how severe maternal anemia compromises the fetal environment. 6. Explain how grand multiparity contributes to neonatal risk. 7. Explain how maternal exposure to teratogenic medications during pregnancy increases neonatal risk. 8. Explain how maternal thyroid disorder can increase risk for the neonate. 9. Explain how maternal history of depression can increase risk for the neonate. 10. Explain how the birth environment contributes to fetal and neonatal risk management. 11. Describe the use of the Apgar score in neonatal risk assessment. 12. Discuss how the Apgar score is assessed and at what time intervals. 5 Course Syllabus ©National College of Midwifery 2012 01/2012 13. Discuss how bleeding during labor can increase risk for the neonate. 14. Discuss how instrument assisted delivery can increase risk for the neonate. 15. Discuss which factors may lead to an increased incidence of breastfeeding problems for the neonate. 16. Discuss how the timing of the initiation of breastfeeding can affect a neonate’s feeding patterns. 17. Discuss how maternal infection increases risk of infection for the neonate. 18. Discuss what factors during the birth increase the chances that neonatal resuscitation will be necessary. 19. Discuss risks faced by a newborn that has required and undergone extensive resuscitation at birth. 20. Discuss how a newborn’s inability to thermoregulate increases risk after birth. 21. Discuss the neonatal risks for infants born to mothers with polyhydramnios. 22. Discuss the neonatal risks for infants born to mothers with placental bleeding in 3rd trimester. 23. Discuss the neonatal risks for infants born to diabetic mothers. 24. Describe the neonatal risks for infants born to mothers with Hepatitis B. 25. Describe the neonatal risks for infants born to mothers with herpes simplex virus. 26. Describe the neonatal risks for infants born to mothers with human immunodeficiency virus (HIV). 27. Describe the neonatal risks for infants born to mothers with cytomegalovirus (CMV). 28. Describe the neonatal risks for infants born to mothers who were exposed to rubella during pregnancy 29. Describe the neonatal risks for infants who mothers’ smoked during pregnancy. 30. Describe the neonatal risks for infants whose mothers’ received live virus vaccines during pregnancy. 31. Describe the risks associated with circumcision of the newborn. 6