GASTROENTEROLOGY
advertisement

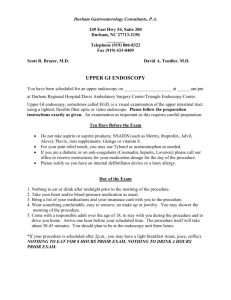
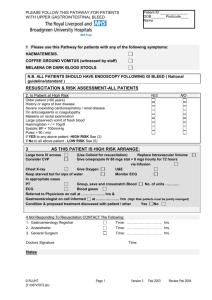
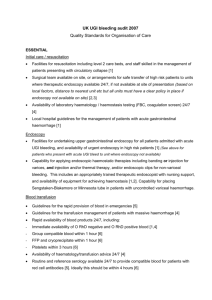
Liver failure Upper GI haemorrhage LIVER FAILURE Aetiology Assessement A Deterioration of chronic liver impairment Alcohol GIT haemorrhage Infection – bacterial peritonitis, viral hepatitis Drugs – diuretics, hypnotics, sedatives, narcotics Metabolic – hypokalaemia, hypoglycaemia Other – constipation, surgery B Acute causes Drugs – paracetamol, idiosyncratic (phenytoin amiodarone, isoniazid, valproate, sulphonamides) Viral hapatitis – A, B, C, D, E Toxins – amanita phalloides, carbon tetrachloride Vascular events – ischaemia, veno-occlusive disease, heatstroke, malignancy Other – Wilson’s (<50); acute fatty liver of pregnancy (3 rd trimester) Reye’s syndrome. A Aims to determine the precipitant as well as assess the current state B ABC’s i.e. CVS and respiratory C Neurological Asterixis – characteristic but not specific Hyper reflexia Grade of hepatic encephalopathy Grade 1: Mildly drowsy, impaired concentration and psychomotor function Grade 2: Confused but able to answer questions Grade 3: Very drowsy – reponds to simple commands Grade 4: Unrousable 4a Responsive to pain 4b Unresponsive D GIT D Renal E Urinary catheter to monitor fluid status Oliguric renal failure develops in 50% General Investigations Jaundice PR blood loss Bacterial peritonitis Look for infection LFT’s – elevated. May return to near normal in end stage Urea, Cr, Na+, K+, PO4, Mg – hyponatraemia, hypokalaemia Glucose – hypoglycaemia Coagulation – prolonged PT (>4 seconds) FBC – infection, low platelets ABG – lactic acidosis is bad prognostic indicator Paracetamol level Blood culture Urine culture Ascites for MCS if present CXR + viral hepatitis screen ) + plasma caeruloplasmin ) + toxicology ) Management in acute failure ABC’s Maintain glucose >3.5mmol/L 10% dextrose 1L 12 hourly and monitor glucose 1 – 4 hourly and if decreased consciousness Fluid and electrolyte balance Maintain K+ >3.5mmolL with supplements Avoid saline, use 5%, 10% dextrose or colloids Treat ascites with spironolactone, frusemide and albumin Low salt diet Correct coagulation Vitamin K 10mg IV daily Folic acid 10mg orally daily Platelets if <20 – 50,000 Decrease nitrogen load Stop dietary protein Lactulose 30ml 3 hourly until diarrhoea then 30ml BD Mag sulphate enema if GI bleeding Decrease risk of stress ulceration Ranitadine 150mg BD orally or 50mg 8 hourly or sucralfate 1g QID orally Treat infection Treat cause – NAC if paracetamol Avoid elevating ICP Head up 100 Consider ICP monitoring Disposition Gastroenterology Consult with DCCM + liver transplant unit UPPER GI HAEMORRHAGE RESUSCITATION / A, B, Cs Oxygen 16g IV cannulae x 2 FBC, INR,U&E, Cr, LFTs, Group & Hold / Crossmatch Crystalloid, colloid, blood and clotting factors PRN ASSESSMENT Assess as High risk – any one of the following risk factors Age > 60 Systolic BP < 100 Hb < 90 g / l Varices or cirrhosis Co-existing disease (CVS, renal, hepatic) Confusion High risk findings at endoscopy may religate the patient to high risk from low risk stigmata of recent haemorrhage, Dieulafoy’s lesion, varices, carcinoma Or as low risk in the absence of these ECG CXR FURTHER MANAGEMENT Dependant on risk assessment High Risk Continue resuscitation and monitoring Omeprazole 20mg orally Octreotide 50 micrograms then 50 micrograms per hour if varices Endoscopy – discuss with gastroenterology registrar. Perform in resuscitation room if unstable. Alternatives are DCCM or theatre. Only haemodynamically stable patients are to be transferred to the Endoscopy Unit. Surgery – surgical registrar should see the patient. Surgery is considered if Exsanguinating bleed Excessive transfusion requirement > 55 or co-morbidity ; > 4 units / 24 hours <55; 6 – 8 units / 24 hours Re-bleed (or 2 re-bleeds and low risk) Carcinoma Low Risk Admit to medical unit Can eat and drink until 6 hours prior to endoscopy Endoscopy on next routine list Surgical registrar is to be made aware of the patient