Fighting Through Pain: Treating Migraines
advertisement

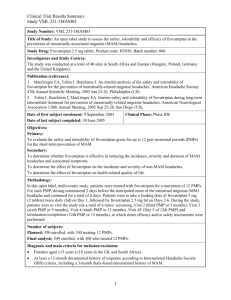
Handout for “Fighting Through The Pain” Please note: Slides for this presentation are protected under copywrite laws and are not to be reproduced or distributed. Only selected slides are available. Fighting Through Pain: Treating Migraines Anne H. Calhoun, MD Clinical Associate Professor, Department of Neurology University of North Carolina Identifying Migraine Prevalence, Pitfalls, and Diagnostic Criteria IF YOU CANNOT HEAR THE PRESENTATION THROUGH YOUR COMPUTER, Listen by telephone by dialing (605) 772-3434, organizer access code 608-643-499 Objectives Identifying Migraine Prevalence, Pitfalls, and Diagnostic Criteria Identifying Migraine: Prevalence Age and Gender Prevalence of Migraine in Adults Migraine Prevalence (%) 30 Females Males 25 20 15 10 5 0 0 20 30 40 50 60 70 80 100 Age (y) Age and Gender Prevalence of Migraine in Adults Lipton et al. Headache. 2001;41:646-657. Identifying Migraine: Prevalence Referred Pain / Autonomic Sxs IHS Criteria: Migraine without Aura ≥5 attacks lasting 4-72 hours Any two: – Moderate-to-severe intensity – Pulsatile – Unilateral – Exacerbated by activity Either: – Nausea – Photophobia & phonophobia Not attributed to other disorder IHS Criteria: Migraine without Aura International Headache Society. Cephalalgia. 2004;24(suppl 1):24-36;139-151. IHS Criteria: Migraine with Aura When to Refer Identifying the patient whose headaches need further evaluation Pharmacists & Headache Care Pharmacists are asked to recommend treatment for headache 53,000 times a day “Excuse Me, Can You Recommend Something for My Headache?” 1. How often do your headaches prevent normal function? 2. How many days per month are you completely headache-free? Q#1: How Often Do Headaches Prevent Normal Function? Q#1: How Often Do Headaches Prevent Normal Function? >50% disabling &/or >20% with vomiting: Refer to physician “Disabling” means: • Cannot perform daily tasks • Missed work/school/family activities • ≥50% reduction in ability to perform chores • Vomiting • Sleep required for improvement >50% disabling &/or >20% with vomiting: Refer to physician <15 days/month? ◦Patient has a chronic daily headache subtype ◦There is a high probability of medication overuse headache (Do not recommend more analgesics) Refer to physician Treat at least 3 attacks ◦With inadequate relief in ≥2 out of 3 attacks, try a distinctly different OTC product Acute Therapy for Migraine Non-specific and Migraine Specific Medications Acute Migraine Medications: The Available Options Nonspecific treatments ◦NSAIDs ◦Combination analgesics ◦Opioids ◦Neuroleptics/antiemetics ◦Isometheptene Specific treatments ◦Triptans ◦Ergotamine/dihydroergotamine (DHE) Acute Migraine Management: Evidence-Based Guidelines NSAIDs as first-line therapy Triptans (or DHE) indicated for those who fail to tolerate or respond to NSAIDs No evidence to support the use of IV corticosteroids or intranasal lidocaine Little evidence to support the use of isometheptene combinations in migraine Opioids should be “reserved for use when other medications cannot be used” The Triptans—Specifically Indicated for Migraine Triptans Are Highly Selective Triptan Effects are Minimal Triptan Binding Shows Craniovascular Selectivity 5-HT1B receptors are denser in meningeal arteries than in coronary arteries Triptans stimulate meningeal 5-HT1B receptors more potently than those in the heart Triptans are unlikely to cause serious cardiovascular (CV) events in healthy patients Available Triptan Formulations Almotriptan ◦Oral 6.25, 12.5 mg Eletriptan ◦Oral 20, 40 mg Frovatriptan ◦Oral 2.5 mg Naratriptan ◦Oral 1, 2.5 mg Achieving optimal results What your clients can do to improve outcome with their medications 4 Reasons for Sub-optimal Response to a Triptan 1. Chronic Daily Headache Analgesic Overuse Can Complicate Patient Profile 2. Hormonally Mediated Migraine Hormonal Treatment of MRM Naratriptan Mini Prophylaxis Randomized, double-blind, parallel-group, placebo-controlled, 3-arm study ◦Naratriptan 1 mg bid for 5 days ◦Naratriptan 2.5 mg bid for 5 days ◦Placebo bid for 5 days Naratriptan 2.5 mg bid was not effective Naratriptan 1 mg bid reduced the median number of MRM attacks in 4 months from 4 to 2 (p=0.01) Frovatriptan Mini Prophylaxis Randomized, double-blind, placebo-controlled, three-way crossover study ◦Frovatriptan 2.5 mg QD for 6 days ◦Frovatriptan 2.5 mg BID for 6 days ◦Placebo for 6 days Incidence of MRM during the 6-day PMP was ◦67% for placebo ◦52% for frovatriptan 2.5 mg QD ◦41% for frovatriptan 2.5 mg BID Both frovatriptan regimens reduced ◦Severity of MRM ◦Duration of MRM ◦Use of rescue medication Impact of MRM 3. Patient Delayed Treatment Central Sensitization Central Sensitization Central Sensitization 4. Headache Awakened Patient • Sleep complaints were common in a sample of 1283 migraineurs • >50% reported insomnia • 71% were regularly awakened by headaches • 50% reported that sleep disturbances triggered migraine • 38% were “short sleepers” (≤6 hrs per night) • Compared to those who slept longer, short sleepers experienced: • More frequent and more severe headaches • More headaches on awakening 4. Headache Awakened Patient Kelman L, Rains JC. Headache and sleep: examination of sleep patterns and complaints in a large clinical sample of migraineurs. Headache. Jul 2005;45(7):904-910. 4. Headache Awakened Patient Study Design In Summary . . . Questions & Answers