BENIGN TUMORS
advertisement

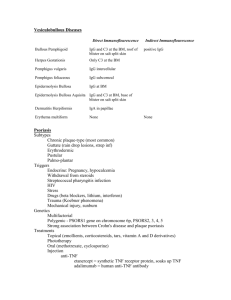
BENIGN TUMORS I. EPIDERMAL A. Keratosis 1. Actinic--sun induced, premalignant ill-defined pink keratotic plaques in sun exposed distribution. 2. Seborrheic--flesh colored to brown waxy verrucous plaques. Well defined lesions, global distribution. No malignant potential. Sign of Leser-Trelat. B. Keratoacanthoma--sun induced. "Self-healing" squamous cell carcinoma. Extremely rapidly growing indurated keratotic pink nodule with central crater and keratin core. C. Skin Tag--acrochordon, fibroepithelial polyp. Flexural folds. ?Associated with GI polyps. D. Clavus--"corn". Thick localized callus with keratin plug. E. Verrucae--warts. Human papilloma virus, 60 known subtypes. 1. Flat 2. Plantar 3. Vulgaris 4. Filiform 5. Venereal--condyloma acuminata F. Cutaneous Horn--indurated pink papule with keratin horn. Wart, actinic keratosis, r/o squamous cell carcinoma G. Nevus Sebaceus of Jadassohn II. DERMAL A. Dermatofibroma--firm, pink-brown plaque or nodule. + "dimple" sign. Lower leg distribution, female greater than male. B. Hemangioma 1. Capillary 2. Cavernous 3. Cherry angioma C. Pyogenic Granuloma--rapidly growing hemangioma with "collarette", Friable, purulent surface. D. Lipoma--moveable firm rubbery subcutaneous nodule(s) with distinct capsule. Isolated or numerous. Often familial. E. Epidermal Inclusion Cyst--"sebaceous" cyst, "wen". III. PIGMENTED A. Nevus 1. Dermal 2. Junctional 3. Compound 4. Congenital 5. Blue 6. Dysplastic--over 5 mm. Macular. Irregular notched borders. Variegated pigment from pink to brown, eccentrically. 7. Halo B. Lentigo--tan maculae, "liver" spots. 1. simplex 2. actinic C. Ephelid--freckle Rovner MALIGNANT TUMORS Basal Cell Carcinoma--sun induced. Minimal metastatic potential I. A. Nodular--pearly, telangiectatic borders. "Rodent" ulcer. B. Superficial--eroded, scaling pink plaques. II. Squamous Cell Carcinoma A. Sun-induced--little metastatic potential. Often arise from existing actinic keratosis. Indurated pink scaling plaques. B. Mucosal--dangerous with high metastatic potential. C. in situ--Bowen's Disease. Well defined psoriasiform plaque in sun exposed area(s). III. Melanoma A. Types 1. Superficial Spreading 2. Nodular 3. Lentigo maligna (Hutchinson's freckle) (i) Lentigo maligna melanoma 4. Acro-lentiginous B. Prognosis 1. Type 2. Location ("BANS" areas) 3. Depth a Clark's level b Breslow scale: Depth %Survival (5 yr) 0--.75 mm 98-100% .75--1.5 mm 90--95% 1.5--3.0 mm 50--75% over 3.0 mm less than 50% C. Treatment 1. wide local excision 2. ?lymph node dissection - [sentinel lymph node] 3. chemotherapy 4. immune modulation Rovner INFLAMMATORY DISORDERS I. ECZEMA--Dermatitis Acute--"juicy" red ill defined plaques with or without vesiculation; pruritus Chronic-lichenification--scaling thickened pink plaques with increased skin markings; pruritus A. Contact--unusual configuration and distribution limited to areas of contact 1. Allergic-a specific sensitivity, not dose dependent b eg: poison ivy, Nickel, fragrances, c preservatives, Neomycin 2. Irritant--non specific a dose dependent b eg: soaps, lye B. Seborrheic--"dandruff" 1. scalp, central face, chest ("oily" areas) 2. ill defined, greasy, yellow scaling pink plaques 3. Pityrosporum ovale C. Dyshidrotic--"Pompholyx" 1. palms, soles 2. "tapioca" vesicles D. Stasis--shins - edema, with diffuse erythema, scaling and purpura E. Xerotic--"dry" skin F. Atopic--asthma 1. flexural fold involvement 2. food allergies (milk, eggs, nuts, wheat, citrus)--RAST testing 3. familial 4. cataracts G. Treatment: identification and avoidance of offending agent(s)--patch test 1. steroids-topical and systemic 2. antihistamines 3. moisturizers 4. antibiotics (Staph aureus) II. PSORIASIS 3% of American population Etiology unknown--increased cell turnover Polygenic inheritance A. Vulgaris 1. well defined pink plaques with "micaceous" scales 2. distribution a elbows, knees b gluteal cleft c scalp d nails--pitting, oil staining e sites of trauma--"Koebner phenomenon" B. Pustular 1. sterile pustules, lakes of pus with diffuse erythematous background 2. palms and soles most frequent sites 3. eruptive (von Zumbusch)--generalized involvement, often steroid induced C. Guttate 1. Wide spread, small "raindrop spattered" plaques 2. post Strep, viral infections D. Psoriatic arthritis--occurs in 3-5% of psoriasis patients 1. mono-articular--most common 2. mutilans (distal interphalangeal, "pencil in cup")--pathognomonic E. Treatment: 1. topical steroids 2. tar 3. UVB 4. PUVA 5. Methotrexate 6. Retinoids 7. vitamin D 8. cyclosporine III. LICHEN PLANUS A. Flat topped violaceous polygonal plaques with white lacy striae (Wickham's) B. ankles, wrists C. oral (buccal mucosa) D. nails (pterygium) E. extreme pruritus Rovner REACTIVE ERYTHEMAS Urticaria, Angioedema Type I hypersensitivity I. Red wheals, plaques with central translucency; pruritic! Lesions recur in crops and waves, each lasting under 24 hours Acute--under 6 weeks Chronic--over 6 weeks A. Types: 1. Angio[neurotic]edema--swelling of lips, genitalia, eyelids 2. Contact--rare; DMSO, cinnamates 3. Papular--insect bite reaction 4. Dermographism 5. Hereditary Angioedema--complement mediated B. Etiology 1. Drugs--antibiotics (PCN, sulfa) salicylates 2. Foods--shellfish, tartrazine dyes 3. Physical Factors--heat, cold, pressure 4. Stress C. Treatment--antihistamines 1. Steroids 2. epinephrine II. Erythema Multiforme Symmetric target "Iris" lesions, often involving palms, soles Resolving within days to weeks A. Etiology 1. Infectious--Herpes virus, mycoplasma, deep fungi 2. Drugs-- -phenobarbital, PCN, sulfa B. Treatment--self limited 1. ? steroids 2. antihistamines 3. treat underlying condition C. Variants 1. Steven's Johnson Syndrome a Erythema multiforme with bullous, erosive lesions b Mucosal involvement c Severe, potentially life threatening 2. Toxic Epidermal Necrolysis a Widespread denudation, sloughing of inflamed skin b Mortality--over 50%! III. Erythema Nodosum (panniculitis) A. painful subcutaneous nodules on anterior shins, bilaterally B. bruising with pink/yellow/purple shiny plaques or nodules C. NO ulceration D. Etiology: Infectious (viral, Strep, deep fungi) E. Drugs (BCP's, PCN) F. Inflammatory Bowel Disease G. Sarcoid H. Treatment--self limited, lasting up to several weeks 1. NSAID's 2. steroids IV. Drug Reactions--Type IV hypersensitivity (except urticaria) A. Morbilliform--symmetric, pruritic coalescent pink papules and plaques 1. typically begins within 1 week of new drug 2. Bactrim, PCN B. Urticaria C. "Fixed"--phenolphthalein (Ex-Lax); Tetracyclines D. Phototoxic--Tetracyclines, Thorazine, NSAID's E. Alopecia--heparin, coumadin F. Bullous--griseofulvin, nalidixic acid G. Lupus Erythematosus--hydralazine, procainamide, INH H. Psoriasis--lithium Rovner INFECTIOUS DISEASES OF THE SKIN Viral I. A. Herpes simplex (types I and II) 1. Primary 2. Recurrent B. Zoster--reactivated Varicella C. Molluscum Contagiosum D. Human Papilloma Virus 1. Warts 2. Condyloma acuminata 3. Cervical dysplasia 4. Laryngeal polyps E. Exanthems 1. nonspecific--similar to morbilliform drug reaction 2. specific II. a Fifth Disease--Parvovirus b Sixth Disease (Roseola)--HSV VI c Hand, foot and mouth disease--Coxsackie virus d ?Pityriasis Rosea - ?HSV VII Bacterial A. Impetigo 1. Staph aureus, NOT Strep 2. Honey colored crusts, erosions with a red base 3. May be bullous 4. Treatment: a Systemic antibiotics b Topical antibiotics ineffective except Bactroban! B. Cellulitis 1. Staph, Strep, H. influenza (children) 2. Tender, bright red dermal plaques with indistinct borders 3. Constitutional symptoms--fever, arthralgias, malaise C. Erysipelas 1. Strep usually causative 2. Extremely well demarcated red indurated plaques 3. Recurrence is frequent D. Mycobacteria 1. Leprosy--M. leprae Tuberculoid TT Borderline BT BB 2. Atypical Mycobacterium-a M. marinum b Fish tank (swimming pool) granuloma E. Pseudomonas--hot tub folliculitis Lepromatous BL LL F. Disseminated 1. Gonococcemia a rare, painful hemorrhagic pustules b palms and soles c septic arthritis 2. Meningococcemia a gun metal grey hemorrhagic pustules b EXTREMELY DANGEROUS 3. Rickettsia--Rocky Mountain Spotted Fever a wood tick vector b acral hemorrhagic papules III. Fungal A. Superficial 1. Dermatophytes a "ringworm, athlete's foot, jock itch" b annular scaling pink plaques with central clearing c Skin--Tinea corporis, cruris, pedis, etc. d Hair--Tinea capitis e Nail--Tinea unguium f 3 genera i Trichophyton spp ii Epidermophyton iii Microsporum spp g Diagnosis--KOH slide h Treatment i topical--imidazoles ii systemic--griseofulvin, ketoconazole 2. Candida--C. albicans a bright red plaques with satellite pustules b skin: moist intertriginous areas (groin, glans, angles of mouth) c oral: thrush d Treatment: nystatin, imidazoles (NOT griseofulvin) 3. Pityrosporum a P orbiculare, ovale b normal commensal in oily areas c Tinea Versicolor (Malassezia furfur) d Folliculitis B. Deep 1. Begin as self limited acute respiratory infection with fever, cough with eventual spread to skin (in rare instances) 2. Histoplasmosis a oral lesions b Ohio River basin c Erythema multiform, Erythema nodosum 3. Blastomycosis a Eastern USA b vegetative, verrucous plaques 4. Coccidioidomycosis a Pacific Southwest b EM, EN 5. Paracoccidioidomycosis--Amazon basin 6. Sporotrichosis--verrucous papules, nodules, plaques, peat moss, rose thorns IV. Infestations A. Scabies--Sarcoptus scabii B. Pediculosis 1. capitus--head lice 2. corporis--body lice (organisms found in seams of clothes only, not on body) 3. pubis a pubic lice "crabs" b also may affect eyelashes Parasites V. A. Cutanea larva migrans (creeping eruption) B. Schistosomiasis--(duck itch, swimmer's itch) VI. Spirochetes A. Syphilis--Treponema pallidum 1. a. Primary--chancre: negative painless, indurated ulcer at inoculation site, RPR 2. Secondary--Pityriasis rosea like rash 1 to 6 months after 10 infection a brown macules on palms and soles b mucous patches c Condyloma lata d RPR positive; spirochetes recoverable from all lesions e latent--RPR remains positive; no lesions 3. Tertiary--5 to 30 years after latency a gumma b arthritides c cardiac, neurologic involvement B. Lyme Disease 1. Borrelia burgdorferii 2. deer tick vector 3. triphasic course: a 10--Erythema chronicum migrans b 20--Fever, arthritis c 30--Late sequelae (cardiac, neurologic) Rovner GENODERMATOSES Ichthyoses I. 1. Genetically determined conditions with thick scaling plates 2. Two mechanisms: a Increased cohesiveness (I. vulgaris, X-Linked Ich). b Increased cellular production (lamellar Ich., epidermolytic hyperkeratosis) 3. Infants often present with membrane ("colloidian baby") 4. Symptoms: 5. II. a pruritus b cosmesis c bacterial 20 infections d odor e ectropion f fluid, electrolyte imbalance Treatment: a antibiotics b moisturization (LacHydrin) Neurofibromatosis (von Recklinghausen's) A. Autosomal dominant B. cafe-au-lait macules (at least 6 greater than 1 cm.) C. neurofibromas 1. typical 2. plexiform-may eventuate in neurosarcoma D. pheochromocytoma E. acoustic neuroma F. **Crowe's sign--axillary freckling G. **Lisch nodules III. Tuberous Sclerosis A. Autosomal dominant B. Ash leaf macules C. Adenoma sebaceum (angiofibromas) D. **Shagreen patch E. mental retardation IV. Peutz Jaegher's A. Autosomal dominant B. Multiple lentigines C. Small intestinal polyps (pre adenocarcinomatous) Gardiner's V. A. Autosomal dominant B. multiple cysts C. colonic polyps (premalignant) VI. Osler-Weber-Rendu A. Autosomal dominant B. Familial hemorrhagic telangiectasia C. Telangiectases on lips, oral mucosa, skin D. Bleeding from CNS, GI tract Rovner BULLOUS DISORDERS Epidermolysis Bullosa--noninflammatory inheritable blistering disorders,skin I. fragility A. E.B. Simplex B. E.B. Letalis (junctional) C. E.E. Dystrophica D. Treatment: trauma avoidance 1. cool environs 2. antibiotics, local wound care 3. steroids 4. Dilantin II. Pemphigus A. Superficial 1. P. foliaceous 2. P. erythematosus B. Deep 1. P. vulgaris 2. P. vegetans C. flaccid bullae on uninflamed base D. + Nikolsky sign E. Pathogenesis: autoantibodies to intercellular cement F. Histopathology 1. acantholysis 2. intrerepidermal bullae 3. + immunofluorescence intracellularly in epidermis G. Treatment: 1. Steroids! 2. immunosuppressants III. Bullous Pemphigoid A. Tense bullae on inflamed base B. Nikolsky sign C. Pathogenesis: autoantibodies to basement membrane zone protein D. Histopathology 1. no acantholysis 2. intact epidermis overlying bulla with eo's, PMN's 3. + immunofluorescence at DE junction E. Treatment: IV. Steroids, immunosuppressants Dermatitis Herpetiformis 1. Intensely pruritic papulovesicles over elbows, knees, buttocks 2. gluten enteropathy (asymptomatic) 3. Pathogenesis: IgA antibodies in dermal papillae 4. Histopathology: Necrosis of dermal papillae with PMN's 5. Treatment: Dapsone, gluten free diet, antihistamines V. Porphyria Cutanea Tarda A. Blisters on dorsal hands with sun exposure B. Zygomatic hypertrichosis C. Marked skin fragility D. Pathogenesis: 1. defect in uroporphyrinogen decarboxylase 2. increased porphyrins excreted in urine (positive fluorescence) E. Aggravated by BCP's, EtOH F. Treatment: 1. phlebotomy 2. antimalarials 3. EtOH avoidance 4. sunscreens Rovner COLLAGEN VASCULAR DISORDERS I. Lupus erythematosis A. Discoid LE (DLE) 1. pink, violaceous well defined plaques in sun exposed distribution 2. scarring, including alopecia 3. follicular plugging, atrophy 4. ANA-negative 5. no systemic manifestations 6. Treatment: a steroids (systemic, topical) b antimalarials c sunscreens B. Systemic LE (SLE) 1. autoimmune antibody/antigen complex deposition with Type III inflammation 2. drug induced a hydralazine b procainamide c isoniazid INH 3. 4 or more ARA criteria for diagnosis: a malar ("butterfly") rash with sun exposure b discoid lesions c photosensitivity d oral ulcers e arthritis f serositis (pleuritis, pericarditis) g renal disease h neurologic sx's (seizures, neuropathy, psychosis) i hematologic (anemia, pancytopenia) j immunologic (anti-DNA ab's; LE prep; false + RPR) ANA 4. Treatment: a steroids b immunosuppressants c antimalarials d sunscreens C. Subacute LE (SCLE) 1. ANA negative lupus 2. +SSA, SSB antibodies (anti Ro, anti La) 3. less cardiac, renal involvement compared to SLE 4. small, annular red plaques in sun exposed areas 5. Neonatal lupus: a (infants born to mothers with SCLE) b 30 heart block c discoid lesions d anemia, "HELP" syndrome (Hepatic Enzymes Low Platelets) e II. usually resolves within 6 months, but heart block permanent Dermatomyositis A. Inflammatory disorder of proximal muscles, skin B. Associated with internal malignancy 25 to 50% in patients over 55 C. Skin: 1. "heliotrope" rash 2. Gottron's papules 3. periungual telangiectases D. Muscle: limb/girdle weakness with abnormal EMG findings E. Laboratory: 1. elevated CPK, Aldolase 2. + ANA 3. ESR elevation F. Treatment 1. treat underlying malignancy 2. steroids III. Scleroderma A. Morphea (localized) 1. atrophic plaques without systemic involvement B. CREST Syndrome 1. Calcinosis cutis 2. Raynaud's disease 3. Esophageal strictures 4. Sclerodactyly 5. Telangiectases C. PSS (Progressive Systemic Sclerosis) 1. proximal sclerosis 2. pulmonary fibrosis 3. renal disease 4. cardiac (restrictive cardiomyopathy) D. Treatment: 1. steroids 2. d-penicillamine Rovner VASCULITIS Definition: Inflammation with necrosis of blood vessels resulting in variable clinical presentations depending upon: 1. size of vessel 2. type of vessel 3. histological infiltrate Pathophysiology: Antigen-Antibody Complex Formation Immune Complex Deposition Complement Derived Chemotaxis PMN Lysosomal Enzyme Release Vessel Wall Injury, Necrosis VASCULITIS I. Vasculitis - Types A. Hypersensitivity Group (Leukocytoclastic) 1. Vessel type: small, usually post capillary venules 2. Symptoms: Skin-Palpable Purpura a vesicles, bullae, ulceration b urticaria (collagen vascular disease) 3. Systemic: a Joints--arthritis (50%) b Renal--hematuria c Other--GI tract 4. Etiology: a Infectious (Strep, viral, Rickettsial) b Drug Reaction c Collagen vascular disease d Cryoglobulinemia e Internal Malignancy f Henoch-Schonlein Purpura g i Palpable purpura (dependent areas-legs and buttocks) ii Abdominal pain iii Arthritis iv Hematuria v Increased IgA Idiopathic 5. Laboratory work-up a CBC, Platelets b Urinalysis, BUN, Creatinine c Chest x-ray d ANA e Cryoglobulins f Serum Protein Electropheresis g ESR (nonspecific) 6. Differential Diagnosis: a Thrombocytopenia b Sepsis 7. Treatment a removal of offending agent b steroids c dapsone B. Polyarteritis Group (Periarteritis) 1. Polyarteritis Nodosa a Vasculitis of small-medium sized arteries with segmental (skip) involvement. b Symptoms: i Constitutional ii Renal--hypertension, glomerulonephritis iii Neuromuscular--arthritis, myalgia, sensorimotor neuropathy (mononeuritis multiplex) iv Gastrointestinal--functional v Cutaneous--Livedo reticularis, Nodules (painful shiny red nodules in crops usually on lower extremities), Ulcerations vi Other--cardiac, CNS c Laboratory Work-Up: Nonspecific d Treatment: i Steroids (50% 5 yr. survival) ii Cyclophosphamide (80% 5 yr. survival) iii None (10% 50 year survival) 2. Churg-Strauss a Allergic granulomatous angiitis b Asthma, Eosinophilia c Pulmonary vessel involvement--100% d Splenic involvement--70% C. Granulomatous 1. Wegener's Granulomatosis a Granulomatous vasculitis of upper and lower respiratory tract, glomerulonephritis, and other small arteries b c d Symptoms: i Respiratory Tract--100% ii sinusitis, rhinitis, septal destruction, cough, dyspnea iii Renal--80% glomerulonephritis iv Cutaneous--40-50% nodules, ulcers v Other--joints, CNS, cardiac Laboratory work-up i ESR markedly elevated ii Chest x-ray (cavitary lesions, nodules) Treatment: i 90% 2 yr. mortality without treatment ii cyclophosphamide and steroids 2. Giant Cell Arteritis II. a Temporal Arteritis (Polymyalgia Rheumatica) b Giant cell infiltrate of large arteries (temporal, carotid) c Severe, disabling musculoskeletal pain, d Blindness without immediate steroids in high doses e ESR extremely elevated (over 100) SYSTEMIC DISEASE A. Pruritus 1. Thyroid (hyper- or hypo) TSH, T4 2. Renal disease BUN, Creatinine 3. Hepatic disease LFT's 4. Malignancy (Hodgkins Disease) Chest x-ray 5. Polycythemia vera CBC, platelets 6. Diabetes glucose B. Endocrine 1. Adrenal a b Addison's Disease i Hypoadrenalism ii generalized bronzing iii dark pigmentation on gums Cushing's i Hyperadrenalism ii moon facies iii buffalo hump iv hirsutism v acanthosis nigracans 2. Thyroid a hyperthyroidism--pretibial myxedema, thyroid acropachy b hypothyroidism--myxedema, alopecia, xerosis, macroglossia 3. Diabetes Mellitis a Necrobiosis Lipoidica Diabeticorum b Diabetic Dermopathy C. Malignancy 1. Pruritus 2. Dermatomyositis 3. Acanthosis Nigracans 4. Acquired Ichthyosis 5. malignant down - lanugo hairs D. AIDS 1. Oral hairy leukoplakia--EB virus 2. Kaposi's Sarcoma 3. Sudden, severe Seborrheic Dermatitis 4. Molluscum contagiosum-- refractory 5. Unusual or opportunistic infections 6. Bacillary angiomatosis 7. Chronic cutaneous herpes virus infections 8. Lipodystrophy Rovner DISEASES OF SKIN APPENDAGES I. Pilo-sebaceous unit A. Acne: inflammatory papules, cysts, or nodules due to follicular plugging and anaerobic breakdown of trapped sebum due to Propionbacterium acnes. 1. Types: a A. vulgaris b A. cosmetica c A. fulminans d A. conglobata e Chloracne--dioxin induced (Agent Orange) 2. Treatment: a avoidance of comedogenic materials b Retin-A (tretinoic acid) c Benzoyl peroxide d Antibiotics: i tetracyclines ii erythromycins (topical or systemic) iii amoxicillin, Bactrim iv clindamycin (Cleocin-T), usually topical e Accutane (isotretinoic acid) f Diet and acne cleansers have NO therapeutic effect II. Sweat ducts A. Eccrine--Miliaria 1. Miliaria rubra--"prickly heat" perifollicular papules 2. Miliaria crystallina--crystal clear superficial vesicles, febrile 3. Miliaria profunda--hyperthermia, no skin signs B. Apocrine 1. Hidradenitis suppurativa--cysts, nodules, sinus tracts and scarring in axillary, inguinal areas III. Alopecia A. Scarring--DLE, lichen planus, male pattern B. Non scarring 1. Alopecia areata--stress induced; pernicious anemia, thyroid disease 2. Telogen effluvium--post partum, stress, crash diets, febrile illness, drugs 3. Anagen effluvium--chemotherapy, trichotillomania IV. Nails A. Tinea unguium B. Psoriasis C. 1/2 and 1/2 nails--renal disease D. White nails (Terry's nails)--liver disease E. Nail Tic Deformity V. Pigmentation A. Melasma, chloasma--reticular hyperpigmentation in sun exposed areas of face, more common in females, estrogen induced B. Vitiligo 1. Autoimmune--may be associated with thyroid anti-microsomal antibodies and pernicious anemia; symmetric depigmentation, accentuated by Wood's light exam; etiology unknown, may run in families Treatment: psoralens, UVB or UVA, topical steroids 2. Contact: phenols (photographic developers) Surgery of the Skin CRYOTHERAPY: minus 40˚ Centigrade for 30 seconds with LN2 wart, keratoses not suitable for tissue requiring histopathologic exam ELECTROCAUTERY: Electrodesiccation Electrofulguration Electrocauterization Hemostasis Superficial lesions, except warts; telangiectases CURETTAGE; wart, keratoses Basal Cell Carcinoma--E&C Electrodesiccation and curettage SCALPEL SURGERY; "cold steel" surgery Elliptical excision --3 times the width of lesion Anesthesia-- 1% xylocaine w/ or w/o epinephrine Benadryl injectable Saline Closure primary--subcuticular sutures for hemostasis and tension placement Secondary--packing Granulation Flaps and grafts--large wounds, cosmesis, function LASER SURGERY; argon--vascular tumors CO2--warts, condyloma Neodymium: YAG Tunable dyes--vascular, pigmented, and other solid tumors MOH'S (CHEMO) SURGERY: SKIN BIOPSY: punch shave recurrent malignant tumors Affords potential best cosmetic result Rovner TOPICAL DERMATOLOGIC THERAPY IV. VEHICLES (BASES) A. POWDERS 1. reduce friction; absorb moisture 2. eg. talc, cornstarch, Zeasorb B. SHAKE LOTIONS/EMULSIONS 1. suspension of non-soluble in liquid/oil 2. drying, soothing 3. eg. Calamine C. SOLUTIONS 1. active medication dissolved in aqueous or alcohol solution 2. useful in hair bearing areas D. GELS 1. similar to a solution, but with an added polymer to provide substance - less "runny" than solutions E. CREAMS 1. oil-in-water (light) or water-in-oil (heavy) 2. require preservatives, emulsifiers, stabilizers 3. cosmetically acceptable F. OINTMENTS 1. nonaqueous base, usually petrolatum 2. greasy, cosmetically not desirable, especially in hair bearing areas 3. usually best delivery system in terms of effectiveness G. PASTES 1. nonvanishing, thick wax based, remain on skin 2. cosmetically unacceptable, messy SOAKS, BATHS V. A. soothing anti-inflammatory, antipruritic, may be anti- infective or used to dry oozing areas or loosen debris in wounds B. Examples: 1. colloidal oatmeal (Aveeno) - soothing 2. Aluminum Subacetate (Dome Boro's) - drying. antibacterial 3. Daikon's Solution - saline with sodium hypochlorite - good debriding agent 4. Tar - anti-inflammatory, useful for eczema, psoriasis 5. Oil - soothing, hydrating VI. ANTI- INFLAMMATORY A. TOPICAL STEROIDS 1. Potency (as determined by vasocontrictor assay): a Classification: Class I - super potent - Class VII - least potent b Concentration c Vehicle d Substitution (fluorination, esterification) 2. Usage a Type of skin b Area to be covered - 30 gms per total body application c Location to be treated - facial and intertrigenous areas require special attention d Cost - generic vs. Brand-name B. TAR PREPARATIONS 1. May be compounded with steroids 2. Messy, staining, potentially irritating a LCD (Liquor Carbonis Detergens) b Anthralin - synthetic c Pine Tar Extracts C. SPECIAL CASES 1. Viaform a Useful in intertrigenous areas 2. Topical Antihistamines and Anesthetics a Any preparation ending with "-dryl" or "-caine" (eg. Benedryl, Caladryl, Benzocaine) is potentially sensitizing. Zonalon (topical doxepin) may be effective 3. Capsaicin a Depletes substance P VII. TOPICAL ANTIBIOTICS A. ANTI-INFECTIVES 1. Bacitracin, Polymixin B, Neomycin - wound healing, - prophylaxis only Polysporin , Neosporin NB: Products with neomycin (eg. "triple" antibiotic) should be avoided due to high incidence of hypersensitivity! 2. Mupiricin (Bactroban) - effective for impetigo 3. Cleocin, Erythromycin - folliculitis 4. Sulfonamides (Azulfidine) - burns 5. Cleansing Agents a Soaps - Deodrant (Triclosan) b Scrubs i chlorhexidene (Hibiclens) ii povidone/iodine (Betadine) iii hexachlorophene (PhisoHex) c Alcohol d Hydrogen Peroxide B. ACNE 1. Erythromycin 2. Clindamycin 3. Tetracycline 4. Meclocycline 5. Sulfonamides 6. Metronidazole (Flagyl) - rosacea VIII. TOPICAL ANTI FUNGALS A. Candida, yeast 1. nystatin (Mycostat) B. Fungi 1. Powders a useful in prevention i tolnaftate ii micostatin iii undecylenic acid 2. Shampoos a Zinc - (Head & Shoulders) b Tar - (T-Gel) c Selenium Sulfide - Selsun Blue d Nizoral 3. Creams/Lotions a Imidazoles i clotrimazole (Lotrimin) ii Ketoconazole, econazole, miconazole b Cyclopirox (Loprox) c Allyl Amines (Lamisil) Rovner SYSTEMIC DERMATOLOGIC THERAPY IX. ANTIBIOTICS - Widespread, deep or potentially life threatening infection, (eg. folliculitis, cellulitis, ecthyma) A. Anti-Staphylococcal 1. Erythromycin 2. Beta-lactamase resistant Penicillins (Dicloxacillin, Augmentin) 3. Cephalosporins (Keflex, Duricef) 4. Penicillin and Tefracycline are NOT appropriate. B. Anti-Streptococcal 1. Erythromycin 2. Penicillins C. Acne 1. Tetracyclines, Minocycline, Doxycyclene 2. Erythromycins 3. Amoxicillin 4. Trimethoprim/sulfa (Bactrim) 5. Clindamycin 6. Cephalosporins (Duricef) X. ANTI-FUNGALS - Widespread or deep infections; nail infections A. Griseofulvin 1. eg. Gris Peg, Fulvicin 2. Dermatophyte infections only - no yeasts! 3. Potentially hepatotoxic, phototoxic B. Imidazoles 1. eg. Ketoconazole (Nizoral), Itraconazole (Sporanox) 2. Drug interactions 3. Potential hepatotoxicity C. Allyl Amines - (Lamisil) XI. ANTI-HISTAMINES A. Sedating 1. Hydroxyzine (Atarax) 2. Diphenhidramine (Benadryl) 3. Cyproheptadine (Periaction) B. Non-sedating 1. Terfenadine (Seldane) Interaction with Macrolides 2. Astemizole (Hismanal) and imidazoles 3. Loratadine (Claritin) C. Mildly sedating 1. Cetirizine (Zyrtec) XII. STEROIDS - used to control acute flare of eczema, pemphigus,urticaria, and other inflammatory dermatoses except psoriasis A. Prednisone - usual dose is 0.5 to 1 mg/kg tapering over 3 to 4 weeks B. Other - equivalence: Decadron Triamicinolone, Prednisone Hydrocortisone Methyl Prednisdone Prednisolone 0.75mg 4mg 5mg 20mg May be given PO, IM, IV, or intralesionally XIII. RETINOIDS - teratogenic A. Accutane (isotretinoin) B. Tegison (etretinate) C. Arotonoids Rovner PEDIATRIC DERMATOLOGY I. CLASSIC EXANTHEMS A. First Disease (MEASLES, Rubeola) 1. Etiology: myxovirus 2. Clinical: age of onset after 6-12 months, 10-11 days' incubation, then fever, coryza, rash 3. Enanthem: Koplik's spots - 1-2 days prior to onset of rash 4. Exanthem: morbilliform a eruption 14 days after inoculation b Posterior scalp-- neck-- face-- trunk, upper extremities c 2-3 days' duration 5. Sequelae: neurologic in up to 50% 6. Prevention: a live attenuated vaccine (MMR) after 12 months b earlier killed vaccines led to atypical measles B. Second Disease (SCARLET FEVER) 1. Etiology: erythrotoxin from Group A Beta-hemolytic Strep, usually from pharygeal infection ("Strep" Throat) 2. Clinical: Sudden, severe after 2-4 days' incubation with fever, sore throat, headache 3. Exanthem: a oropharyngeal erythema b "Strawberry" tongue 4. Sequelae: a rheumatic fever 2-3 weeks post infection b glomerulonephritis 5. Treatment: Penicillin C. Third Disease (RUBELLA, German Measles) 1. Etiology: paramyxovirus 2. Clinical: a 12-25 days' incubation b 4-5 day prodrome (fever, malaise) with adenopathy (post cervical) 3. Exanthem: a 2-3 day course b small pink papules on face with peripheral spread to trunk and arms over 1 day c clearing in upper extremity, with involvement of lower extremity 4. Enanthem: a Forchheimer's spots - petechiae on soft palate b coincident with exanthem 5. Sequelae: a Usually none b Neonatal Rubella Syndrome 6. Prevention: live attenuated virus (MMR) D. Fourth Disease (Duke's Disease) 1. Historical significance only 2. ? ECHO virus exanthem 3. ? Scarlatiniform eruption E. Fifth Disease (Erythema Infectiosum) 1. Etiology: Human Parvovirus 2. Clinical: a children 5-15 years b mild constitutional symptoms c 1-2 week duration, waxing and waning 3. Exanthem: a "slapped" cheek appearance b reticulated erythema over upper back, shoulders, buttocks 4. Enanthem: none 5. Sequelae: none, but adults may have lingering malaise, arthragias, fever F. Sixth Disease (Exanthem Subitum, Roseola) 1. Etiology: Herpes Virus VI 2. Clinical: a young children (6 months to 2 years) b 10-12 days' incubation c High fever spike, 2-3 days' duration 3. Exanthem: a abruptly follows defervescence b short lived (1 day's duration) c faint pink macules from neck to trunk d facial sparing 4. Enanthem: none 5. Sequelae: febrile seizures, (non specific) 6. Prevention: none II. VARICELLA (CHICKEN POX) A. Etiology: Varicella Zoster Virus B. Clinical: 1. 10-20 days' incubation 2. 1 day prodrome of fever, malaise C. Exanthem: 1. successive crops 2. congested papules becoming vesicular ("dew drop on a rose petal"), then crusted 3. central distribution (face, scalp, trunk) palms, soles spared 4. 1 week's duration (maybe up to 3 weeks) D. Enanthem: flaccid vesicles progress to white ulceration on hard palate, tonsillar pillars E. Sequelae: 1. uncommon in immunocompetent 2. Zoster (Shingles) F. Treatment: Acyclovir, Valcyclovir, Famcyclovir G. Prevention: Vaccine III. KAWASAKI'S DISEASE (mucocutaneous lymph node syndrome) A. Etiology: uncertain B. Clinical: infants, young children C. Criteria: 1. 5 or more days of fever 2. conjunctivitis 3. Strawberry tongue, oropharyngeal erythema 4. erythema and subsequent peeling of hands, feet 5. scarlatiniform rash 6. acute cervical adenopathy 7. elevated platelets D. Sequelae: coronary arteritis, aneurysms E. Treatment: 1. ? Antibiotics 2. ? Steroids IV. COMMON CHILDHOOD PROBLEMS - (treatment considerations) A. Atopic Dermatitis B. Warts C. Molluscum Contagiosum D. Poison Ivy E. Ringworm F. Drug eruptions G. Viral Exanthems H. Acne I. Impetigo NEONATAL DERMATOLOGY "TORCH" SYNDROME - "blueberry muffin baby" I. A. Toxoplasmosis B. Other C. Rubella D. Cytomegalovirus E. Herpes Simplex II. COMMON NEONATAL ERUPTIONS A. Erythema Toxicum [Neonatorum] B. Neonatal Acne C. Milia