Overview of Good Practice and Good Practice Recommendations
advertisement

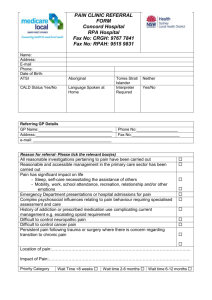
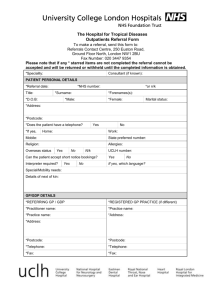
Safer Care North East: Falls Group Recommendations for Good Practice and Mapping of Existing Services Against Recommendations: Falls Services North East Strategic Health Authority Introduction Safer Care North East is an enabling strategy which aligns to and complements the North East Our Vision, Our Future Strategy and the North East Transformation System (NETS). It provides a focus on specific clinical safety issues, one of which is Falls. The membership of the Safer Care North East Falls Group consists of key individuals from the Falls and Osteoporosis Services across the North East Strategic Health Authority and representatives from the North East Ambulance Service, Pharmacy Services and the Voluntary Sector. Meetings in early 2009 established a consensus view to agree Recommendations for Good Practice for a Whole Systems Falls Service under the headings: 1. Organisational Issues. 2. Services Delivered. 3. In-patient / Hospital Falls. 4. Care Homes. 5. Training. 6. Information. 7. Quality Metrics. The Falls Services then rated themselves against individual recommendations and provided narrative comment to further describe their service. Good Practice Recommendations The Good Practice Recommendations agreed by the Safer Care North East Falls Group are as follows: 1. Organisational issues i. Falls Strategy which all organisations (health -hospital and PCT, social care, voluntary sector and others) have ownership of and are working to achieve. ii. Individual or group who have responsibility for Falls Strategy / other Falls initiatives and the enthusiasm, time and mandate to implement them. iii. Formal communication mechanism between all organisations involved in Falls / Falls Prevention / Falls Service Delivery. iv. Good links with Commissioners and Public Health Physicians. 1 v. Referral mechanism into Falls Services that gives access to range of health and social care professionals, the voluntary sector and older people themselves. vi. Standardisation of documentation. vii. Good links with community initiatives as ‘step-down’ from Falls Service. viii. Good links with local Telecare services. ix. Good links with community pharmacy services. x. Older people themselves have a key role in planning, implementing and delivering Falls Services. xi. Robust referral pathway from the Ambulance Service. xii. Robust referral pathway from the Accident and Emergency Department. xiii. Robust referral pathways from Orthopaedics (including Fracture Clinic) and other services e.g. Medical Admissions Unit, Neurology where fallers present. xiv.Osteoporosis link nurse (or similar) working closely with Fracture Clinic / Orthopaedics and the Falls Services. 2. Services Delivered i. Multifactorial assessment and intervention following NICE guidelines. ii. Specialist Falls and Syncope Service. iii. Falls Services screen for and treat osteoporosis. iv. Falls Services delivered in the community, close to / in older people’s own homes. v. Community based targeted strength and balance exercise programme following evidence based protocols. 3. In-patient / Hospital Falls i. Commitment to falls prevention at board / senior management level. ii. Commitment of front line manager to implement risk reporting and falls assessment and intervention protocols. iii. Accurate and complete falls reporting (e.g. via Datix). iv. Contribute to the National Hip Fracture Database. v. Falls assessment documentation coupled with interventions to prevent falls / refer for further assessment. vi. Staff training in falls risk reporting / assessment of falls risks / falls prevention interventions / referral pathways. 4. Care Homes i. Training package for care homes on falls prevention and on when and how to refer to falls services. ii. Good links with care homes to encourage uptake of training and referral to falls services. 5. Training i. Training for health and social care professionals and others in management of falls. and on when and how to refer to falls services. ii. Training package around inpatient falls – see above. 2 iii. Training package for care homes – see above. iv. Training package for sheltered housing schemes and day care on falls prevention and on when and how to refer to falls services. 6. Information i. Provision of falls prevention information for older people and their carers. 7. Quality metrics i. Data collection that allows development of clinically relevant quality metrics. Mapping of Existing Falls Services Against Good Practice Recommendations Services / areas rated themselves broadly against their own recommendations using the following scale: - outstanding good practice; - established good practice; - some areas of good practice; & - something similar / work in progress; Gap - not available. The outcomes are summarised in the table below according to trusts / geographical areas in order to reflect patient experience of the Falls Service. Areas of service delivery are summarised as: County Durham and Darlington (CDD); Newcastle (NCL); North Tees and Hartlepool (NT&H); Northumberland (N’bria); Gateshead (Ghead); South Tees (Sth Tees); Sunderland (S’drl’d); North Tyneside (Nth T’side); South Tyneside (Sth T’side). For most areas (indicated by *) more than one trust contributed to services delivered and information supplied. For some areas, particularly County Durham and Darlington, it was difficult to provide an overview of patient experience as there was a wide variation in service provision. In Northumberland some parts of the service previously provided by the FISHNETS project were not fully funded and are indicated as such in the table. The Newcastle Falls and Syncope Service takes referrals from across the region. The information represents the knowledge of service provision in their area by the members of the group. There is no information for South Tyneside as despite several attempts to contact key people from the Falls Service there is no representation from this area. Representation from North Tyneside has been limited and the information for this area may be a reflection of this. 3 Mapping of Existing Falls Services Against Good Practice Recommendations Good Practice 1. Organisational issues Falls Strategy which all organisations (health -hospital and PCT, social care, voluntary sector and others) have ownership of and are working to achieve Individual or group who have responsibility for Falls Strategy / other Falls initiatives and the enthusiasm, time and mandate to implement them Formal communication mechanism between all organisations involved in Falls / Falls Prevention / Falls Service Delivery Good links with Commissioners and Public Health Physicians Referral mechanism into Falls Services that gives access to range of health and social care professionals, the voluntary sector and older people themselves Standardisation of documentation Good links with community initiatives as ‘step-down’ from Falls Service Good links with local Telecare services Good links with community pharmacy services Older people themselves have a key role in planning, implementing and delivering Falls Services Robust referral pathway from the Ambulance Service Robust referral pathway from the Accident & Emergency Department Robust referral pathways from Orthopaedics (including Fracture Clinic) and other services e.g. Medical Admissions Unit, Neurology where fallers present Osteoporosis link nurse (or similar) working closely with Fracture Clinic / Orthopaedics and the Falls Services 2. Services Delivered Multifactorial assessment and intervention following NICE guidelines Specialist Falls and Syncope Service Falls Services screen for and treat osteoporosis Falls Services delivered in the community, close to / in older people’s own homes Community based targeted strength and balance exercise programme following evidence based protocols CDD* NCL* NT&H* N’bria* Ghead Sth Tees* S’drl’d* Nth T’side & f f f f & Gap Gap Gap Gap & Gap Gap f & & & Gap & & & & Gap + & f & Gap & Sth T’side 4 Good Practice 3. In-patient / Hospital Falls Commitment to falls prevention at board / senior management level Commitment of front line manager to implement risk reporting and falls assessment and intervention protocols Accurate and complete falls reporting (e.g. via Datix) Contribute to the National Hip Fracture Database Falls assessment documentation coupled with interventions to prevent falls / refer for further assessment Staff training in falls risk reporting / assessment of falls risks / falls prevention interventions / referral pathways 4. Care Homes Training package for care homes on falls prevention and on when and how to refer to falls services Good links with care homes to encourage uptake of training and referral to falls services 5. Training Training for health and social care professionals and others in management of falls and on when and how to refer to falls services Training package around inpatient falls – see above Training package for care homes – see above Training package for sheltered housing schemes and day care on falls prevention and on when and how to refer to falls services 6. Information Provision of falls prevention information for older people and their carers 7. Quality metrics Data collection that allows development of clinically relevant quality metrics CDD* NCL* NT&H* N’bria Ghead Sth Tees* S’drl’d Nth T’side & f & Gap & f Gap & f & & Gap Gap Sth T’side * More than one trust represented in comment (hospitals and PCT) KEY: - outstanding good practice; - established good practice; - some areas of good practice; & - something similar / work in progress; Gap – not available; f = input previously provided via FISHNETS in Northumberland – pilot funding ended – ongoing work not fully funded; + Newcastle Falls and Syncope Service takes referrals from across the region 5 Notes on Mapping of Existing Falls Services Against Good Practice Recommendations 1. Organisational issues Falls Strategy which all organisations (health -hospital and PCT, social care, voluntary sector and others) have ownership of and are working to achieve Individual or group who have responsibility for Falls Strategy / other Falls initiatives and the enthusiasm, time and mandate to implement them o S’drl’d: City wide and Hospital based Strategy Group. Strong leadership from both Falls Coordinator and Consultant Geriatrician. o Sth Tees: Close working between Clinical Lead/falls coordinator and hospital senior nurse. Consultant Geriatrician member of Falls Strategy and Osteoporosis Steering Groups. o NCL: Newcastle Falls Clinical Network: Acute Trust, PCT, NEAS, Social Services, Voluntary Sector, Osteoporosis Service. Also within organisation groups for falls e.g. PCT services working to common strategy. o NT&H: Individual multi-agency steering groups which span across Health and Social Care and patient representative. The aims of the groups are to develop the falls strategies and initiatives and service improvements for both localities. o CDD: CDD wide monthly meeting takes place, also locality based meetings which include voluntary social services and NEAS. Osteoporosis Steering group established across primary and secondary care. o Ghead: Close working between falls team and risk management. Reducing Harem from Falls Steering Group. Aim to implement recommendations from Patient Safety First document. Falls Prevention identified as a priority of SafeCare Council. o NthT’side: Via North Tyneside Falls Prevention Service DH Integrated Care Pilot; multi-organisational service involving NuTH acute trust, PCT, General Practice, Social Services, NEAS, Age Concern and Newcastle University. Monthly steering group meetings, regular updates for GPs. Formal communication mechanism between all organisations involved in Falls / Falls Prevention / Falls Service Delivery o S’drl’d: City wide and Hospital based Strategy Group with multi-agency representation. o Sth Tees -Middlesbrough, Redcar & Cleveland Community Services (MRCCS) Falls Team hold central falls register and multi-agency strategy group. o NCL: via Newcastle Falls Clinical Network. Also good informal links at PCT medical staff work into acute trust falls service. o N’bria: FISHNETS project. o NT&H: Hold individual falls databases of fallers referred into falls services in order to establish trends and gaps. The two falls coordinators work closely together to develop an integrated service. o Ghead: Falls Strategy Group. Also hold falls database of all people who are referred to the falls service 6 o CDD: Falls Prevention Service in place, working closely with community, health and social care and voluntary agencies. o NthT’side: Via North Tyneside Falls Prevention Service DH Integrated Care Pilot as above. Good links with Commissioners and Public Health Physicians o Sth Tees: good links with commissioner; elderly care pathways group involving commissioner. o NCL: links with new commissioner and public health being established. o NT&H: North Tees as above. o CDD: Service has been going through review with the commissioners, gaps have been identified and funding was agreed through the AOP, however this has currently been frozen. o Ghead: Links with Public Health being further established. o NthT’side: Excellent links with commissioners: lead commissioner for elder care and deputy director of commissioning for North of Tyne PCT both steering group members for North Tyneside Falls Prevention Service. Referral mechanism into Falls Services that gives access to range of health and social care professionals, the voluntary sector and older people themselves o S’drl’d: 2 referral and assessment tools: ‘Trigger Tool’ (NEAS) for quick referral and more detailed assessment for community matrons / district nurses to allow to manage falls as well as refer. o Sth Tees: 2 referral tools as above. Self – referral from A&E as well as stage one screen A&E, MAU, ambulance and GP referral. Stage 2 multi-factorial assessment/intervention tool carried out by community staff. o NCL: 2 referral tools as above. PCT (all services) and Acute Trust Day Hospital take referrals from all health profs / care homes / NEAS / care alarms / A&E. Acute trust falls service – GP and A&E. o N’bria: Well organised referral mechanism, including self-referral. o Ghead: Well organised system of open referrals inc. wardens, home helps, care alarms and nursing homes o NT&H: Use FRAT (Stage 1) and Multifactorial Falls Assessment Tool (Stage 2) recommended by NICE guideline as referral form. Falls services receiving referrals from Primary and Secondary Care and other community services etc. o CDD: Community based falls service with robust working links to Health & Social Care, Warden services, Care homes and voluntary agencies. o NthT’side: Falls Prevention Service refers to Age Concern-run strength and balance training classes; Social Services refer to the Service and vice versa. In process of trying to replicate NEAS success in other areas. Standardisation of documentation o All: Standard documentation for referrals from NEAS. o S’drl’d: Standard documentation across PCT / acute trust. o NCL: Across PCT organisations but different to acute trust. o Ghead: Standardised document and Falls Risk Assessment tool used across acute trust. Standardised Home Safety assessment used by OT teams across acute trust and PCT. 7 o N’bria: as part of FISHNETS. o Sth Tees: Standardised documentation across Acute, Community and Social Care. o NT&H: Both PCT areas use same referral forms and procedures. o CDD: Five areas all use SAP. Standardised local referral forms, slightly altered for professional/ non-professional referrals, i.e. we ask for more detail from professionals referring into the service. Good links with community initiatives as ‘step-down’ from Falls Service o NCL: Links with step-down exercise project just established. 36 week evidence based programme based on FAME protocol. o N’bria: Good links with community activities as part of FISHNETS. o S’drl’d: Health Trainer / Community Development Workers. o Sth Tees: Good links with postural stability classes in community run by sports development (does not cover all areas). o NT&H: Hartlepool: Falls prevention full day event in UHH hospital every 3 months to recall past fallers during that period for clinical assessment, but they also receive fun, interactive sessions from a wide range of agencies on falls prevention including information on local physical activity opportunities, podiatry, physio, healthy eating, fire service, NEAS etc. These sessions also provide feedback from past fallers which help to shape future service development. o CDD: Good links established eg Established links with PCT ‘Get Active Team’ who provide exercise classes, walking groups and swimming. Useful step-down for some of our clients. Also links with Age Concern befriending service and benefit advice. All clients receive a pack with useful information about falls prevention and contact details for useful agencies on discharge. PSI x2 weekly for 6 weeks courses are run by our physiotherapist as part of the patient’s step-down process. o NthT’side: Falls Prevention Service Age Concern-run strength and balance training classes run courses of 10 hour long weekly sessions with personal trainer using evidence based targeted exercises; participants then referred into existing Age Concern classes per ability. Good links with local Telecare services o NCL: established direct referral pathway from community care alarm service directly to falls services (PCT and Acute Trust). Referrals from falls services to community alarm service. o NT&H: established direct referral pathway from community care alarm service directly to falls services. o CDD: Good established links with Telecare Provider, all requests for fall detectors are referred to us and we frequently request telecare for complex fallers. Six week review appt is a joint telecare / falls team visit. o Ghead: Links with Telecare being further established. Good links with community pharmacy services o Sth Tees: some initial work done. o NT&H: exploring possibilities. o S’drl’d: exploring possibilities. Older people themselves have a key role in planning, implementing and delivering Falls Services o S’drl’d: Monitor patient outcomes / patient feedback questionnaire. 8 o Sth Tees: Patient satisfaction questionnaire including falls related outcomes, focus groups, discovery interviews. Clinical Lead attends LINK falls sub group. o NCL: Patient feedback Questionnaires, input from patient groups and voluntary sector to service planning. o N’bria: Fantastic involvement of older people in FISHNETS pilot – planning, budget, acting as volunteers to deliver services but this has not continued after project. o NT&H: Patient feedback – see above. Also working on patient satisfaction questionnaire – roll out May 2009. Hartlepool use local groups of older people ‘Encore’ who provide falls prevention information in song and sketch format. o CDD: Patient survey carried out in January, also linking to Age concern and local groups. o NthT’side: Falls Prevention Service patient feedback questionnaires and wider associated staff questionnaires on rolling basis; input from STARS syncope patient support organisation and Age Concern. Robust referral pathway from the Ambulance Service o All services have this except North Tyneside – being addressed. o CDD: Agreed documentation, some issues around communication within pathway this is being worked on, eg in Easington the process agreed and appears to be working satisfactorily. Robust referral pathway from the Accident and Emergency Department o Sth Tees – self referral using questionnaire version of Cryer Tool. o NCL: Acute trust plans for Falls Liaison Nurse in A&E ?implementation. Some links via Primary Care Response Team. Referral pathway to Falls Services in Acute Trust and PCT but under-used. o NT&H: Links established with A&E therapy teams at both site (UHH and UHHT). The team assesses patients in A&E, EAU and MAU and refer to falls services if necessary and with patients consent. Gap for orthopaedics. o N’bria: Falls nurse screens casualty cards daily (Mon – Fri). o S’drl’d: Falls coordinator has trained all staff in A&E to use the trigger tool and refer although number of referrals are often spasmodic and not representative of attendance in A&E. o Ghead: Good links with walk-in centre. Referrals to OT in Falls team for people who fall via OT OOH service for A & E. Links established with A & E staff increased referrals to the Falls team but numbers still not representative of numbers presenting. Monthly information received by Falls Service from information department re people over 55 years attending A & E as the result of a fall. o CDD: Fracture Liaison service established across County Durham and Darlington, also established good practice at Sunderland Royal as part of Joint initiative with Sunderland Falls Service. Other areas Hartlepool, Durham – pathways not established yet. Robust referral pathways from Orthopaedics (including Fracture Clinic) and other services e.g. Medical Admissions Unit, Neurology where fallers present o Sth Tees: Robust referral mechanism for inpatients to falls services (across trusts for registration only). Referral pathways from A&E and MAU (for over 65s). 9 o NCL: Referrals from Orthogeriatrics, Fracture Clinic, Orthopaedic Discharge Team and Medical Teams but can be patchy. o NT&H: see above. o CDD: Recently established Fracture Clinic link with Sunderland Royal, also receiving Appropriate low trauma fractures via Durham Fracture Liaison Service, these are primarily seen for Osteoporosis risk but falls risks are also addressed if required. Eas. Also some links via Community Matrons – work to do on linking with MAU. o Ghead: Referrals form Orthogeriatrics and general Orthopaedics. Robust referral pathway and joint working with Community Orthopaedic Rehab Team. Further work to be undertaken with MAU for fallers over 65 years. Osteoporosis link nurse (or similar) working closely with Facture Clinic / Orthopaedics and the Falls Services o NCL: Fracture Liaison Nurse based in Fracture Clinic – DEXA at time of Fracture Clinic attendance and refer to falls services as needed. Also Orthogeriatric Service review all IP Fracture on Orthopaedics and refer to falls services as needed. o CDD: Fracture liaison service – community based with links to fracture clinic. o N’bria: Fracture liaison nurse just appointed. o Ghead: Fracture Liaison Nurse covers all orthopaedic wards including Orthogeriatrics. She also runs Osteoporosis clinic with physician and directs referrals to the team. o Sth Tees – Osteoporosis Nurse now recruited within MRCCS Falls Team and to set up community based osteoporosis liaison service. o NthT’side: Falls Prevention Service – all attendees at the Service are FRAX-screened with treatment/DEXA referral according to need. 2. Services Delivered Multifactorial assessment and intervention following NICE guidelines o NCL: MDT teams based in day hospitals and community. o N’bria: Locality based Community Rehab Teams. o CDD: Specialist teams in North Durham, Darlington, and Easington but there are identified gaps in Sedgefield and the Dales. o Sth Tees: MDT assessment by specialist falls team. Multifactorial assessment/intervention tool for inpatients and community. o NT&H: Multifactorial assessment and intervention in patient’s homes, care homes and other community settings (e.g. day centres). o Ghead: MDT assessment by Specialist Falls team based in acute hospital. Multifactorial intervention in patients homes. o NthT’side: Falls Prevention Service – multifactorial, multidisciplinary community based service; unique proactive case finding from GP case notes and triaged according to need. Eventual aim for wider referral and eventual self referral/referral by carers. Specialist Falls and Syncope Service o NCL: Acute Trust Falls and Syncope Service – particular expertise on syncope and vestibular dizziness; plus also MDT falls, osteoporosis screening, links with day hospitals / community teams for more extensive MDT input (PCT and Acute Trust). PCT Day Hospital (which 10 o o o o o o also does initial medical screen for community teams) includes basic syncope investigations – 12 lead ECG and beat to beat active stand. Sth Tees: Have agreed pathway and multidisciplinary falls team but this has no medical input. Close links with Consultants in Elderly Care who see patients with unexplained falls. Referral pathway for syncope investigations but not part of the Falls Service. NT&H: Consultant led falls clinic at both UHH and UHNT for medical fallers. Community falls teams can directly refer patients in if possible syncope is identified from multifactorial assessment. N’bria: Consultant / Specialist Nurse Practitioner. Ghead: Consultant led Syncope and CSM clinics in acute. MDT Falls team with links with day Hospital and all community rehab teams. CDD: Specialist service provided by acute sector in Sunderland, Hartlepool and Durham hospitals. We have direct referral access to Hartlepool and Sunderland but not yet to Durham. NthT’side: Specialist service at Rake Lane, Wansbeck run by Northumbria. Falls Prevention Service run by consultants with falls and syncope training, all attendees have ECG and beat-to-beat active stand. Falls Services screen for and treat osteoporosis o NCL: PCT Falls Service also run axial DEXA scanner; Acute Trust Falls and Syncope Service have peripheral DXA and robust referral mechanism to osteoporosis service. o Sth Tees: Falls Service screen, assess and refer for osteoporosis management. o Ghead: Osteoporosis screening as part of standardised documentation. Robust links with Fracture Liaison Nurse and Osteoporosis service. o CDD: All patients referred to the Falls Service have a bone health screening as part of the initial assessment (questionnaire). Follow up referrals for dexa scans are requested via patients GP. o NthT’side: Falls Prevention Service – all attendees FRAX screened and/or treated per NICE/NOGG/North of Tyne guidance. Falls Services delivered in the community, close to / in older people’s own homes o NCL: Community Resource Teams deliver MDT falls assessments in people’s own homes with links to Day Hospitals for medical reviews. o N’bria: Locality bases Community Rehab Teams. o Ghead: Falls assessments in Care Homes, Promoting Independence Centres and patient’s own homes with Clinic attendance for medical assessment/review if required. o Sth Tees: Falls team deliver services in patients own homes as well as local primary care hospitals. o NT&H: Community falls teams provide assessment and intervention in people’s own homes including domiciliary rehab plans with links to rehabilitation Day Units. Can refer in to falls classes if significant gait and balance issues are identified or if rehab difficult in patients own home. o CDD: There are a combination of home visits and community based clinics. House-bound patients are seen by relevant clinicians at home. o NthT’side: Falls Prevention Service based at community resource centre in North Shields. 11 Community based targeted strength and balance exercise programme following evidence based protocols o NCL: New 36 week evidence based community exercise programme funded by commissioners to start 1st June 2010. o N’bria: 12 week leisure centre based exercise programme via FISHNETS. o Sth Tees: Falls team provide 12 week programme and sports development provide 24 week programme with plans to roll out to 2 to 3 additional areas, (not all areas have classes). Home exercise programmes following the Otago programme carried out by Falls Team. Network of appropriately trained people who can deliver postural stability or chair based exercise classes. It is coordinated by the Falls Team and includes sports development staff, physiotherapists and other Health and Social Care Staff who have completed Postural Stability Instructors or Chair-Based Leaders exercise courses. o CDD: Otago exercises in community in Darlington. CDD Eas. PSI six week courses are held as part of step-down process for suitable patients. In a local community setting. o NthT’side: Falls Prevention Service/Age Concern strength and balance training classes as above. 3. In-patient / Hospital Falls Commitment to falls prevention at board / senior management level o Sth Tees: Annual report presented at both Management group and Trust Board in Acute Trust and MRCCS. Inpatient falls analysis/work reported to PCT Risk Management Forum and Governance Committee. o Ghead: Inpatient incidents/analysis via Datix presented at Patient Quality Risk and Safety Committee and also at SafeCare Council. Commitment of front line manager to implement risk reporting and falls assessment and intervention protocols o Sth Tees: very committed front line manager in trauma. Shown correlation between implementation of falls assessments and intervention and reduction in falls. Monitor and report on compliance with falls policy. Clinical lead/Falls Coordinator developed action plans with Clinical Matrons in Primary Care Hospitals, rolling programme of training available for inpatient and community staff. o Ghead: DATIX implemented across Foundation Trust. Falls Team involved from inception to identify information recorded re falls. PCT due to adopt DATIX soon. Compliance with falls policy monitored through regular audit. Accurate and complete falls reporting (e.g. via Datix) o Sth Tees: modification of Datix to try to improve falls reporting accuracy. Primary care hospitals use MIDAS system. Acute trust produces detailed monthly reports to Governance Committee, Chief Executive and Director of Nursing and Patient Safety. MRCCS (Middlesbrough Redcar & Cleveland Community Services) produce monthly reports for Clinical Matrons of each Primary Care Hospital. Training delivered by Falls Team includes reporting of falls. o N’bria: developing new system to include NPSA recommendations. 12 o Ghead: Using DATIX with good success. System now adapted to include mandatory field for falls score. Quarterly reports re inpatient falls incidence/analysis produced by falls team. Contribute to the National Hip Fracture Database o All relevant trusts do. Falls assessment documentation coupled with interventions to prevent falls / refer for further assessment o Sth Tees: Assessment triggers falls care plan. Inpatient and community. o NCL: PCT inpatient services and Falls Checklist and Prevention – Intervention plan in community. o N’bria: Assessment triggers falls care plan. o Ghead: Falls team active involvement with management of falls in hospital. Falls Risk assessment tool used across all inpatient services. Tool includes pointers to appropriate interventions/investigations Staff training in falls risk reporting / assessment of falls risks / falls prevention interventions / referral pathways o Sth Tees: Training on incident reporting and falls. Competency based training delivered to all staff by Falls Team. o N’bria: Mandatory staff training. o Ghead: Training on falls prevention / falls management / falls risk. 4. Care Homes Training package for care homes on falls prevention and on when and how to refer to falls services o Sth Tees: Training package and tools for care homes delivered by Falls Team who provide an advice line and referral pathway. o N’bria: Excellent programme as part of FISHNETS – not maintained in full. o Ghead: Direct referrals, accepted from care home staff. All care homes have falls prevention resource pack. Falls assessments undertaken in care homes. Falls awareness sessions fro care home staff offered on request basis at present. Falls training package currently being developed. o CDD: Training package offered and delivered to all care homes consists of half day session looks at bone health, falls prevention and assessment tools. Followed by all residents being assessed with support from the Falls Coordinator. This is not currently consistent across CDD. Working with commissioners to look at this. o S’drl’d: Training aimed at all staff across primary care including nursing homes, voluntary agencies, domiciliary care i.e. anyone who comes into contact with the elderly can access the training free of cost. Good links with care homes to encourage uptake of training and referral to falls services o N’bria: Excellent links as part of FISHNETS – not maintained in full. o Ghead – see above. o NT&H: postural stability exercises in care homes. 13 o Sth Tees: Good links – training and support targeted to care homes with high referral/falls rates. o CDD: Good links established and working well. 5. Training Training for health and social care professionals and others in management of falls and on when and how to refer to falls services o Sth Tees: Fantastic Training Package aimed at all health and social care staff. o NT&H: Training programme developed and delivered to health and social care professionals. A more in depth training programme for qualified staff is being developed. o NCL: Joint training (ad hoc) delivered by acute trust, PCT and NEAS. o S’drl’d: see above. o Ghead: Provided on an ad hoc / request basis. Work ongoing to develop standardised training sessions for health and social care staff. A more in depth training programme for qualified staff is currently being piloted. o CDD: Various packages available for groups including Health & Social care, voluntary agencies, Care home staff, warden services. o NthT’side: Falls Prevention Service – ongoing education for GPs and associated teams of community nursing and physiotherapy teams. Training package around inpatient falls – see above Training package for care homes – see above Training package for sheltered housing schemes and day care on falls prevention and on when and how to refer to falls services o NT&H: activity coordinators in sheltered housing. o Sth Tees: Pilot undertaken in sheltered housing. Falls awareness events held in sheltered housing and other community locations. o CDD: Wardens work closely with falls service eg in Easington falls coordinator delivers short information sessions to wardens on request. o S’drl’d: see above. o Ghead: Falls service attend wardens meetings to raise awareness re falls prevention and to highlight referral pathway to team. 6. Information Provision of falls prevention information for older people and their carers o Sth Tees: Superb provision of information distributed by Falls Team to all inpatient and community staff, GP practices, health promotion teams and libraries. o N’bria: Excellent FISHNETS web site and local events ?continuing o Ghead: Falls workbook provided as part of older persons attendance at Gait and Balance exercise group. o NT&H: Both PCTs have falls prevention leaflets that have been disseminated to patients, carers and other health and social care services. 14 o NCL: Specialist information around cardiovascular falls. o CDD: Information provided by falls teams to patients and carers, a combination of national and local information. Also within Easington a pack is sent to referred patients/carers who do not meet criteria but who can then access falls prevention info and can self refer if concerned. o NthT’side: Falls Prevention Service – paperless service apart from individualised care plan printed out and given to older people and their carers in association with printed falls prevention information, leaflets detailing home exercises for those with gait and balance problems and written conservative advice for neurally mediated disorders and orthostatic hypotension. 7. Quality metrics Data collection that allows development of clinically relevant quality metrics o Sth Tees: Falls Team developing a set of quality metrics including use of outcome measures to demonstrate reduced falls risk. Benchmark with NPSA figures. Falls, is one of the CQUINS measures. o NT&H: Working with Clinical Governance to develop measures. o CDD: developing key outcome measures to be collected consistently for falls and osteoporosis. o NthT’side: All clinical information housed on SystmOne database facilitating easy collection and analysis of relevant metrics. o All areas: SHA level metrics for falls being developed. Organisations contributing comments: South Tees Hospitals Trust Middlesborough, Redcar and Cleveland Community Services North Tees PCT Hartlepool PCT North Tees and Hartlepool Foundation Trust County Durham PCT Darlington PCT County Durham and Darlington Foundation Trust Northumbria Health Care Foundation Trust NHS Newcastle and North Tyneside Community Health Sunderland PCT Gateshead PCT Gateshead Health Foundation Trust Newcastle upon Tyne Hospitals Foundation Trust North Tyneside Falls Prevention Integrated Care Pilot 15 Purpose of this document The purpose of this document is to: 1. Provide consensus recommendations for the organisation and delivery of Falls Services. 2. Highlight areas of particularly good practice across the North East, allowing services to learn from each other. 3. Highlight for a particular service which areas may be a priority for further development. 4. Provide local comparators for Falls Services, a powerful tool in influencing change. 16 Contacts for Falls Services South Tees Hospitals Trust glynis.peat@stees.nhs.uk Middlesborough, Redcar and Cleveland Community Services julie.irwin@middlesbroughpct.nhs.uk North Tees PCT yvonne.cheung@stockton.gov.uk Hartlepool PCT justin.ditchburn@nhs.net North Tees and Hartlepool Foundation Trust Chris Ward via lorraine.bassam@nth.nhs.uk County Durham and Darlington PCTs V.hall3@nhs.net elizabeth.boal@nhs.net County Durham and Darlington Foundation Trust Carol.Robinson@cddft.nhs.uk Northumbria Health Care Foundation Trust David.Richardson@northumbria-healthcare.nhs.uk Northumberland Care Trust Helen.Thompson@northumberlandcaretrust.nhs.uk NHS Newcastle and North Tyneside Community Health Fiona.Shaw@newcastle-pct.nhs.uk Sunderland PCT Christine.Kelley@sotw.nhs.uk Sunderland Hospitals Foundation Trust andrew.davis@chs.northy.nhs.uk Gateshead Falls Service karen.hunter@ghpct.nhs.uk Newcastle upon Tyne Hospitals Foundation Trust john.davison@nuth.nhs.uk North East Ambulance Service philip.kyle@neas.nhs.uk North Tyneside Falls Prevention Service steve.parry@nuth.nhs.uk 17