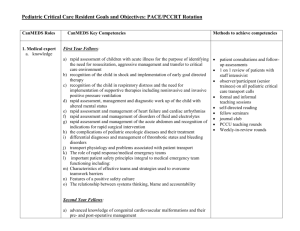
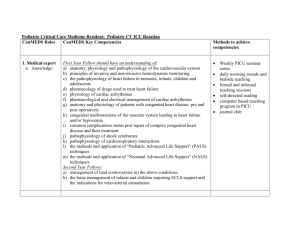
to read the full list of fellowship goals.
advertisement

New York Presbyterian Hospital/Columbia University Fellowship Program in Pediatric Gastroenterology, Hepatology, and Nutrition Educational Goals and Objectives The general goals and objectives of the Pediatric Gastroenterology Hepatology and Nutrition Fellowship Program are found in the Pediatrics-Gastroenterology, Hepatology and Nutrition Fellowship Program binder. During the three years of training our Pediatric-GI fellows will gain progressive clinical mastery including a more extensive breadth and depth of knowledge that encompasses the core compliances. Fellows consult on a broad range of clinical gastroenterological problems including a wide range of general GI diseases, liver diseases, liver and small bowel transplantations, intestinal rehabilitation as well as a wide range of nutritional disorders. Fellows will interact with general pediatric residents and faculty as well as fellows and faculty from other subspecialty divisions within Pediatrics, Radiology, Pathology and Surgery. Fellows will develop diagnostic and therapeutic expertise in the areas of gastrointestinal, hepatologic and nutritional disorders. Fellows will always behave responsibly and respectfully, with high quality interactions with patients’ families, healthcare workers, physicians, nurses and ancillary staff. The Pediatric-Gastroenterology, Hepatology and Nutrition fellows will gain proficiency in the procedural skills of gastroenterology including upper endoscopy, colonoscopy, polypectomy, biopsy techniques of the intestine, cauterization and injection of bleeding intestinal lesions, sclerotherapy, band ligation, percutaneous gastrostomy tube placement, liver biopsy, intestinal stricture dilatations, foreign body retrieval and ph probe placement. By the completion of the three years of training the Fellow will have achieved competence and independence to practice Pediatric Gastroenterology, Hepatology and Nutrition in the community. INDEX OF COMPETENCIES: PC=Patient Care; MK=Medical Knowledge; PBLI=Practice-Based Learning & Improvement; ICS=Interpersonal & Communication Skills; PROF=Professionalism; SBP=Systems-Based Practice The Fellow will: Objective 1: (MK, ICS) Acquire and demonstrate knowledge about core areas in pediatric gastroenterology, hepatology, and nutrition by: Year 1 Participating in daily multi-disciplinary Pediatric GI/Liver Attending rounds Attending pediatric GI didactic Fellows’ conferences, GI Grand Rounds, radiology and pathology conferences and GI Journal Clubs. Teaching sessions with pediatric residents and students Attending and/or participating in General Pediatric Grand Rounds and Chief of service rounds Demonstrating independent directed reading. Year 2 – as above with the following additions: Preparing and presenting at GI Grand Rounds, GI Journal Club, GI didactic Fellows’ conference and Chief of service rounds Preparing and presenting at GI Combined Pediatric and Adult Gastroenterology conference Preparing and presenting abstract submissions to local, national and international conferences Preparing and presenting IRB submissions for clinical studies Year 3 – as above with the following additions: Preparing and presenting products of independent research Mentoring junior Fellows Objective 2: (MK, PC, ICS, PBLI) Develop and demonstrate patient history-taking, diagnostic, and management-planning knowledge and skills by: Year 1 Learning to take a focused history with emphasis on factors affecting GI/Liver/Nutrition health and disorders in both the inpatient and outpatient setting Learning to recognize presentations of various gastroenterological liver and nutritional diseases Learning to recognize modalities for diagnoses and treatment Learning to generate a differential diagnoses Learning to develop treatment plans in unison with the GI/Liver Attending Learning to effectively communicate treatment plan to pediatric residents, patient families, nursing staff and other team members. Learning to communication the progression and outcomes of needed diagnostic and therapeutic interventions Coordinating consultations with other pediatric and surgical subspecialties Coordinating discharge planning with social work and nursing staff Attending weekly Fellow continuity outpatient clinic Year 2 – as above with the following additions: Honing skills acquired during the first year Developing greater independence with continued guidance by Attending Physician Year 3 – as above with the following additions: Teaching and mentoring junior Fellows in the development of the skills perfected throughout the fellowship Objective 3: (PC, ICS, PBLI) Acquire and demonstrate patient management skills for patients with acute and chronic diseases of the digestive system and liver by: Year 1 Learning through direct interaction and observation of the Attending Physician with patient, family and staff Learning through assessment, presentation and discussion with the continuity clinic Attending Physician Learning to recognize, prioritize, and act based on diagnostic and therapeutic needs Learning to describe the appropriate treatment interventions with emphasis on timing and evolution of patient needs Learning to make treatment recommendations in concert with Attending Physician and associated treating health care workers Coordinating patient care and discharge planning with pediatric housestaff, subspecialty services, nursing, social work, family, referring physician and home care companies Year 2 – as above with the following additions: Honing skills acquired during the first year Developing greater independence with continued guidance by Attending Physician Year 3 – as above with the following additions: Teaching and mentoring junior Fellows in the development of the skills perfected throughout the fellowship Objective 4 (PC, MK, PBLI): Acquire and demonstrate the ability to perform gastroenterology procedures by: Year 1 Learning the following procedural skills with close supervision provided by GI attending physicians: o upper endoscopy o colonoscopy o polypectomy o biopsy techniques of the intestine o cauterization and injection of bleeding intestinal lesions o sclerotherapy o band ligation o percutaneous gastrostomy tube placement o liver biopsy o intestinal stricture dilatations o foreign body retrieval o ph probe placement Year 2 Continuing to improve clinical and procedural skills, mentioned above, through continuity clinic, 2-3 week inpatient coverage, and participation in advance procedure rotations Year 3 Solidifying clinical skills through continuity clinic, 2-3 week inpatient coverage, and participation in advance procedure rotations. Honing procedural skills through continued participation in the advanced procedure rotation and performance of procedures on continuity clinic patients. Objective 5 (ICS, Prof, SBP): Acquire and demonstrate ability to communicate in high quality interactions with patients, families, and healthcare workers as well as physician, nursing, and ancillary staff by: Year 1 Learning to provide patients and families with information in a way that is easy to understand and culturally sensitive Demonstrating responsible and respectful behavior with patients and families. Learning to interact with general pediatric residents and faculty Learning to interact with faculty from other subspecialty divisions within Pediatrics, Radiology, Pathology, and Surgery. Learning to communicate effectively with referring physicians and outside institutions through correspondence, HIPPA compliant electronic communications and direct phone contact Learning to field questions, gather information from outside sources, interpret data and offer preliminary advise for further discussion with Attending physician Learning to limit discussions regarding patients and families to appropriate faculty and staff in the appropriate and private venue Year 2 Continuing to develop and demonstrate competency in the above areas To model appropriate behavior and skills for junior Fellows Year 3 Solidifying and honing communication skills through continued adherence to the developed standards Assuming a leadership and mentoring role for junior Fellows Objective 6 (MK, PBLI): Acquire and demonstrate the ability to support one’s own education and provide accessible information to patients by: Year 1 Learning to participate in the education of patients, families, medical students, residents, and other fellows Learning to accept and use feedback to identify areas of need and set goals for improvement Developing effective and efficient self-learning skills that include electronic resources, published data and evidence-based practice Year 2 Demonstrating the ability to effectively teach patients and families within a learned scope of practice supported by available data Demonstrating the ability to use feedback to set goals for improvement. Demonstrating the ability to teach medical students, residents, other fellows through journal clubs and combined Pediatric/Adult GI clinical conferences. Demonstrating the ability to effectively lecture during Chief of Service Rounds, didactic Fellows’ conference and GI Grand Rounds Year 3 Continuing to teach students, residents, GI Fellows, and in-rotating Fellows in formal electives, through journal clubs and case conferences Objective 7 (SBP): Demonstrate knowledge of important systems and regulatory requirements of medical training and practice; and demonstrate adeptness in using the system of care in a way that is beneficial and vital for excellent patient care by: Year 1 Active knowledge and participation in the hospital policy and procedures related to medical errors and medication reconciliation with an understanding of reported problem resolution Knowing and complying with rules and regulations of hospital/HIPAA policies Knowing and complying with rules and regulations of institution/Division/ACGME in regards to moonlighting, duty hours, substance abuse and stress management Familiarity with American Board of Pediatrics guidelines for fellowship accreditation Knowing and complying with ongoing faculty and program evaluation Developing awareness/consideration of cost and risk benefit analysis in rendering patient care decisions with understanding of resource allocation Recognizing the rules and regulations of the institution and governing bodies concerning conflict of interest in medical decision making Year 2 Continuing to develop and demonstrate competency in the above areas Modeling appropriate behavior and skills for junior Fellows Developing familiarity with rules and regulations of the institutional IRB and Federal regulatory commissions concerning basic science, clinical and animal research Recognizing the rules and regulations of the institution and governing bodies concerning conflict of interest in medical research Year 3 Solidifying and honing skills learned in year one and two Assuming a leadership and mentoring role for junior Fellows Developing familiarity with rules and regulations regarding funding opportunities to support research interests Objective 8 (MK): Demonstrate the ability to work on original research by: Year 1 Indentifying a particular area of interest and the appropriate mentor for a research project Formulating and initiating plans for future research (basic, clinical, or translational) under the guidance of a selected mentor Reviewing the available literature and back ground pertaining to the area of research and identifying gaps in knowledge to focus a research project with mentor guidance Presenting research ideas to the Scholarly Oversight Committee (SOC) in accordance with the American Board of Pediatrics guidelines Using the critiques of the SOC to modify the focus and particulars of the proposed research Year 2 Designing a project that is hypothesis driven with identified resource needs and that is feasible in the remaining 2 years of Fellowship to produce a meaningful end-product worthy of publication Considering the elements of data collection guided by the foreseen statistical analyses to be employed Submitting the needed IRB support documents Initiating the research project Updating research progress to the Scholarly Oversight Committee (SOC) in accordance with the American Board of Pediatrics guidelines Year 3 Completing the research project First authoring a paper, chapter, case report, and/or case series Submitting an abstract to a national meeting such as NASPGHN, AASLD, DDW and ATC Presenting research as a poster or oral presentation at national meeting such as NASPGHN, AASLD, DDW and ATC Presenting final research intra-departmentally and/or intra-institutionally Presenting final research to SOC for approval of scholarly work Guiding junior Fellows in the early stages of research development with lessons learned