Lithium shared care guideline - South West London and St George`s
advertisement

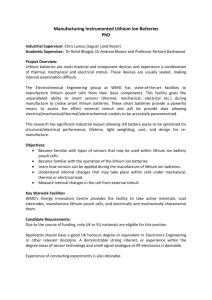
SHARED CARE PRESCRIBING GUIDELINE Shared Care Guideline: Prescribing Agreement Oral Lithium for Affective Disorders Section A: To be completed by the hospital consultant initiating the treatment GP Practice Details: Patient Details: Name: ……………………………………… Name: ……………………………………………… Address: …………………………………… Address: …………………………………………… Tel no: ……………………………………… DOB: ……/………/………… Fax no: ……………………………………… Hospital number: ………………………………… NHS.net e-mail: …………………………… NHS number (10 digits): ………………………… Consultant name: …………………………… Clinic name: …………………………………. Contact details: Address: ......................................................................................................................... Tel no: ……………………………………… Fax no: ……………………………………… NHS.net e-mail: …………………………… Diagnosis: Drug name & dose to be prescribed by GP: …………………………………………………… ……………………………………………………………. Next hospital appointment: ……/……/…….. Dear Dr. …………………….., Your patient was seen on …../..…/………and I have started …………………………………………….(insert drug name and dose) for the above diagnosis and are stabilised on this treatment. I am requesting your agreement to sharing the care of this patient from …../.…./…….. in accordance with the attached Shared Care Prescribing Guideline (Title: Oral Lithium for Affective Disorders) Please take particular note of Section 2 where the areas of responsibilities for the consultant, GP and patient for this shared care arrangement are detailed. Patient information has been given outlining potential aims and side effects of this treatment and lithium booklet supplied. The patient has given me consent to treatment possibly under a shared care prescribing agreement (with your agreement) and has agreed to comply with instructions and follow up requirements. . The following investigations have been performed on ……/……/……… and are acceptable for shared care. Please monitor………...........every ……….. Test Result Test Result Lithium level U&E (Na, Ca, Cr & eGFR) TFT (T4, TSH) Weight (or BMI) Latest blood results attached (tick) Other relevant information: ……………………………………………………………………………………….. ……………………………………………………………………………………………………………………….. Section B: To be completed by the GP and returned to the hospital consultant as detailed in Section A above Please sign and return your agreement to shared care within 14 days of receiving this request Tick which applies: □ I accept sharing care as per shared care prescribing guideline and above instructions □ I would like further information. Please contact me on:………………………. □ I am not willing to undertake shared care for this patient for the following reason: ………………………………………………………………………………………………………………. GP name: ………………………………………….………. GP signature: ………………………………………………Date: …/…/….. Date original approved: February 2004 Date next review due: Feb 2015 Date last review approved: Feb 2013 1 SHARED CARE PRESCRIBING GUIDELINE working in partnership with SHARED CARE PRESCRIBING GUIDELINE Oral Lithium for Affective Disorders NOTES to the GP The expectation is that these guidelines should provide sufficient information to enable GPs to be confident to take clinical and legal responsibility for prescribing this drug. The questions below will help you confirm this: Is the patient’s condition predictable or stable? Do you have the relevant knowledge, skills and access to equipment to allow you to monitor treatment as indicated in this shared care prescribing guideline? Have you been provided with relevant clinical details including monitoring data? If you can answer YES to all these questions (after reading this shared care guideline), then it is appropriate for you to accept prescribing responsibility. If the answer is NO to any of these questions, you should not accept prescribing responsibility. You should write to the consultant within 14 days, outlining your reasons for NOT prescribing. If you do not have the confidence to prescribe, we suggest you discuss this with your local Trust/specialist service, who will be willing to provide training and support. If you still lack the confidence to accept clinical responsibility, you still have the right to decline. Your PCT pharmacist will assist you in making decisions about shared care. It would not normally be expected that a GP would decline to share prescribing on the basis of cost. The patient’s best interests are always paramount Date first prepared: January 2004 Date reviewed: January 2013 Date review approved: February 2013 Next review date: February 2015 Prepared by: Carl Holvey, Principal Pharmacist SWLStG MH Trust Approved by: S W London Mental Health Prescribing Forum (January 2013) S W London & St Georges Mental Health NHS Trust Drug & Therapeutics Committee (Feb 2013) Participating Primary Care Organisations Kingston CCG Dr Anthony Hughes, GP on behalf of Medicines Management Committee Seema Buckley, Chief Pharmacist Richmond CCG Dr Darren Tymens, Associate Medical Director Emma Richmond, Head of Medicines Management Merton CCG Dr Andrew Otley, Mental Health Lead Brigitte van der Zanden, Chief Pharmacist NHS Wandsworth Dr Gillian Ostrowsky, Associate Medical Director Nick Beavon, Chief Pharmacist Sutton CCG Dr Chris Kears, Mental Health Lead Brigitte van der Zanden, Chief Pharmacist Participating Hospital Trusts SWL & St. George’s Mental Health Trust Helen Miller (DTC Chair & Consultant Psychiatrist) Dianne Adams (DTC secretary & Chief Pharmacist) Date original approved: February 2004 Date next review due: Feb 2015 Date last review approved: Feb 2013 2 SHARED CARE PRESCRIBING GUIDELINE ORAL LITHIUM FOR AFFECTIVE DISORDERS 1. CIRCUMSTANCES WHEN SHARED CARE IS APPROPRIATE Prescribing responsibility will only be transferred when the consultant and the GP are in agreement that the patient’s condition is stable or predictable. The patients will only be referred to the GP once the GP has agreed in each individual case and the hospital will continue to provide prescriptions until successful transfer of responsibilities as outlined below. The hospital will provide the patient with a minimum initial supply of 2 weeks therapy. 2. AREAS OF RESPONSIBILITY In general the various responsibilities will be shared as outlined below, but for an individual patient there may be some variation in the detail (e.g. on who does which blood tests) but this must be clearly agreed between the consultant and GP Consultant GP Formulate diagnosis and initiate Prescribe specific dosage, form and brand of lithium ensuring treatment plan monitoring results indicate it is safe to do so, adjusting dosage as required. If liquid is prescribed note, SWLStG uses only the Follow mental Health Trust guidelines for prescribing and monitoring lithium high strength lithium citrate liquid (1018mg/5ml, 400mg therapy lithium carbonate = 5ml of this strength). Provide verbal and written information Measure lithium plasma levels every 3 months in accordance to the patient and answer their questions with NICE guidelines (or at any other time if signs of toxicity) and about lithium send a copy of the results to the CMHT. Establish willingness for adherence to If monitoring results not available at the time of prescribing, lithium treatment (to avoid abrupt prescribe only a limited supply (e.g. maximum 14 days) and cessation of treatment) arrange for blood tests. Perform baseline checks of physical If patient refuses blood tests, prescribe only a limited supply health (including body weight and ECG), (e.g. maximum 14 days) and discuss urgently with CMHT. Patients renal and thyroid function, serum calcium, who have the capacity to decide and who refuse 3 monthly blood creatinine, eGFR and sodium (recorded in levels, may encounter problems with obtaining supplies from the electronic care notes). FBC should be community pharmacies. Appendix 1 of this document may be done if indicated. useful to aid this communication. Initiate lithium treatment and establish Measure thyroid function and renal function every 6 months in desired dose / blood level accordance with NICE guidelines and send a copy of the results to Provide lithium treatment pack to the CMHT. patient containing lithium information Update the patient’s lithium record book with all results and booklet, lithium alert card and lithium changes in treatment when presented by patient record book, and complete with relevant Perform annual health checks including record of body weight in details accordance with NICE guidelines (including serum calcium) Check on going monitoring of lithium Monitor mental state occurs Monitor adherence to medication Communicate to GP: Assess for signs of adverse effects Dosage, form & brand of lithium to be Be alert for medicines that interact with lithium; if any are added, prescribed (this must be specified in all stopped or have their dosage changed re-check the lithium level correspondence, prescriptions and the and observe for any signs of toxicity or of relapse of symptoms. patient’s lithium record Contact mental health community team or medicines Current lithium plasma level information for advice on: dosage adjustment to maintain lithium Desirable plasma level range to be level, management of adverse effects or patients who refuse blood maintained tests. Frequency of follow-up appointments Refer patient back to CMHT if concerns over mental state or with CMHT and communicate treatment concerns over poor compliance with treatment and of physical changes to the GP promptly within Trust health issues that affect dosing or treatment. recommended times. N.B. results of all tests and investigations should be copied by / to both consultant and GP Patient and Carers responsibilities Carry lithium book to required appointments and allow Health Care professionals involved in their care to see the book. Date original approved: February 2004 Date next review due: Feb 2015 Date last review approved: Feb 2013 3 SHARED CARE PRESCRIBING GUIDELINE 3. COMMUNICATION AND SUPPORT Hospital contacts: Out of hours contacts & procedures: (the referral letter will indicate named consultant) ENTER CONTACT DETAILS OF YOUR LOCAL CMHT The on-call psychiatrist at your local hospital can be contacted via the hospital switchboard: Springfield 020 3513 6000 Tolworth 020 8390 0102 Tel: Fax: E-mail: Specialist support/resources available to GP including patient information: Additional information on any aspect of lithium treatment is available from Mental Health Medicines Information 020 3513 6829 Patient information leaflets & lithium books for patients are available from Springfield Hospital Pharmacy 020 3513 6204. Information leaflets, choice of treatment for illnesses & illness leaflets (funded by SWLStG): http://www.choiceandmedication.org/swlstg-tr/ 4. CLINICAL INFORMATION Place in Therapy: Therapeutic summary: Dose & route of administration: Duration of treatment: Monitoring Requirements: The NPSA Patient Safety Alert states that NHS providers “should ensure that patients prescribed lithium are monitored in accordance with NICE guidance” Date original approved: February 2004 Date next review due: Feb 2015 One of the drugs of first choice for established recurrent illness instead-of or in addition to antipsychotics and/or antidepressants as appropriate. Treatment and prophylaxis in mood disorders – exact mechanism of action unknown Dose - established for each individual patient to produce the desired blood level (usual therapeutic range 0.4 – 1.0mmol/l but specific target level will be individual for each patient). Route of administration – oral (see notes on formulations in “practical issues” section below). For prophylaxis, likely to be for several years General monitoring of the patient’s mental state, adherence to treatment and for any adverse effects of their medication. Every three months*:(*NICE recommendations) o lithium blood level (sample taken 12 hours after last dose) Every six months*: o measure thyroid function o measure renal function Annually*: o physical health check including measure of body weight and serum calcium. In addition, measure lithium blood levels if signs of toxicity or relapse of illness appear, or if any medication is added / removed which may affect lithium blood levels (See interactions section) Request on each laboratory form that a copy of all results be sent to both consultant & GP. Date last review approved: Feb 2013 4 SHARED CARE PRESCRIBING GUIDELINE Summary of adverse effects: Adverse effect Frequency Management (See summary of product characteristics (SPC) for full list) N.B. because of potential risk to unborn child, women of childbearing age should be clearly informed of the risks of pregnancy and should be encouraged to discuss with you any possible pregnancy, plans to breastfeed (or plans to conceive) as early as possible. Lithium toxicity (signs: Unknown Stop lithium, vomiting, diarrhoea, polyuria, increased thirst, coarse tremor, ataxia, muscle pain / weakness, drowsiness, confusion) (affected by dosage, drug interactions, physical illness, salt & fluid balance) measure lithium blood level urgently, rehydrate, contact CMHT, DO NOT force diuresis, consider A+E referral Impaired renal function Unknown contact CMHT (identified by monitoring) Impaired thyroid function Unknown contact CMHT ACE inhibitors and Angiotensin-II antagonists – increased lithium blood level (monitor lithium closely until stabilised) Analgesics – decreased lithium excretion by azapropazone, diclofenac, ibuprofen, indometacin, ketorolac (avoid concomitant use), mefenamic acid, naproxen, parecoxib, piroxicam, rofecoxib, and probably other NSAIDs (risk of lithium toxicitymonitor lithium closely until stabilised) Antidepressants – SSRIs may increase risk of CNS effects Antipsychotics – increased risk of EPSE / neurotoxicity with clozapine, haloperidol, phenothiazines, sulpiride; increased risk of ventricular arrhythmias with amisulpride, sertindole, thioridazine Acetazolamide – increased lithium excretion (monitor lithium closely until stabilised) Diuretics – decreased lithium excretion/increased lithium blood level. Loop diuretics safer than thiazides (monitor lithium closely until stabilised) Methyldopa – neurotoxicity without increased lithium blood level (monitor patients for sign of toxicity) (identified by monitoring) Clinically relevant drug interactions: N.B. included are the “potentially hazardous” interactions as listed in the BNF – see BNF / SmPC for more complete information N.B. increased lithium plasma level/decreased lithium excretion brings the risk of lithium toxicity N.B. the effect of adding these drugs to lithium treatment is described here – the opposite effect is likely if the drug is withdrawn N.B. care may also be needed if one interacting drug is switched for another (e.g. change in diuretic) Practical issues: Date original approved: February 2004 Date next review due: Feb 2015 Formulations of lithium Different brands and forms of lithium are likely to produce different lithium blood levels The brand & formulation of lithium should remain unchanged for a patient & should be specified on each prescription, in all correspondence and on the patient’s lithium record card/book Take extra care when prescribing lithium in liquid form, as different brands contain very different concentrations of lithium (e.g. Li-Liquid (Rosemont) is available in 2 strengths) SwLSTG only uses 1018mg/5mL Lithium citrate liquid. 5mL of this liquid is equivalent to 400mg of lithium carbonate (Li-liquid). If the lithium level is outside the desired range for this patient If level is above 1.0mmol/l contact the patient to arrange urgent assessment and to ensure that they take no more lithium and monitored for signs of toxicity. Otherwise: Confirm correct dosage is being prescribed / taken Confirm blood sample taken 12 hours post-dose Date last review approved: Feb 2013 5 SHARED CARE PRESCRIBING GUIDELINE Check for drug interactions (N.B. some over-the-counter drugs may interact e.g. ibuprofen) Check hydration and salt intake or loss Assess physical & mental state of the patient Adjust the dosage if indicated and repeat level after 5-7 days Potential risk in pregnancy Because of the potential risk to the unborn child, women of childbearing age should: Be clearly informed of the risks of pregnancy Be encouraged to discuss with you any possible pregnancy as early as possible Be encouraged to discuss with you any plans to conceive as early as possible Contact Mental Health Medicines Information (020 3513 6829) or the Perinatal Mental Health Service for advice. Key references: Date original approved: February 2004 Date next review due: Feb 2015 NPSA Patient Safety Alert NPSA 2009/PSA005 “Using lithium safely” Drug & Therapeutics Bulletin 1999, 37, 22 “Lithium for maintenance treatment of mood disorders” (Cochrane review), Burgess S et al In: The Cochrane Library, Issue 3, 2001 British National Formulary March 2010, no 59 NICE clinical guideline 38 - Bipolar Disorder, July 2006 SwLSTG Lithium prescribing and monitoring. TWC21j. Date last review approved: Feb 2013 6 SHARED CARE PRESCRIBING GUIDELINE Date: Psychiatric team to Insert GP Address Insert unit/team/hospital address & Telephone number Dear Colleague, RE: (APPENDIX 1): Healthcare professional letter regarding patients’ refusal of lithium monitoring. First name Surname – DOB – NHS number Patients address The above patient refuses to have three monthly monitoring of their lithium level (and or other regular blood testing) as recommended by the National Institute of Clinical Excellence and The National Patient Safety Agency. The patient will have at least yearly monitoring of all the physical parameters. The clinician below has discussed the risks of not complying with these tests, which are an inability to check for side effects and toxicity due to lithium therapy. The patient has been given written information regarding lithium but still refuses to have on going blood tests. Our discussion is fully documented in the electronic care notes. This patient therapeutically benefits from this treatment and considers the risk of not having on going monitoring one worth taking. In the opinion of the clinician below this patient has the capacity to make this decision and requests that you continue to prescribe and/or supply lithium as described on the prescription under the wishes of the patient. Yours sincerely, Clinician signature Service user signature Name of clinician & designation Date original approved: February 2004 Date next review due: Feb 2015 Date last review approved: Feb 2013 7