Thyroid - This Is Not A Clinic
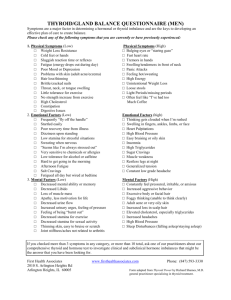
advertisement

Overview of Thyroid Functioning in the ICU Setting Introduction Abnormal thyroid functioning is a complicated entity in the critical care unit because of its uncertain significance. Abnormal thyroid panels in critical care patients can be attributed to both changes in the hypothalamic-pituitary-thyroid axis and peripheral thyroid hormone regulation. Often these patients are given the diagnosis of euthyroid sick syndrome (ESS). Controversy has surrounded around whether ESS should be considered thyroid dysfunction or a beneficial physiological response to illness. And further, whether critically ill patients could benefit from thyroid replacement. Normal Thyroid Hormone Synthesis and Regulation Thyroid Hormone Production Thyroid hormone is, obviously, produced in the thyroid. The requirement for thyroid hormone production is 1 mg of iodine per week 6. Thyroid hormone is produced via a five- step process 1: 1. The trapping on Iodide (I-) within the gland 2. The Oxidation of I- to I2 3. The incorporation of I2 into thyroglobulin to form either monoiodotyrosine (MIT) or diiodotyrosine (DIT) (also called the “organification of iodide”) 4. The coupling of MIT and DIT. One MIT and one DIT can couple to form triiodothyronine (T3) or two molecules of DIT can couple to form thyronine (T4) 5. Storage of iodinated thyroglobulin within the follicular lumen until the thyroid gland is stimulated to release thyroid hormones 2 1 Peripheral Conversion of Thyroid Hormone T3 is three to five times more potent in effect than T4 1. Approximately 20% of T3 is synthesized in the thyroid gland while 80% of comes from peripheral conversion 4. T4 is converted by peripheral tissues, chiefly the liver and kidneys, to T3 by the enzyme type I iodothyronine-5’-deiodinase 7. Additionally, T4 can be converted peripherally to the metabolically inert molecule reverse T3 (rT3) by the enzyme 5-deiodinase. rT3 is cleared much quicker than T4 with its half-life being only several hours instead of a week 10 . Normal Regulation of Thyroid Secretion Centrally, thyroid secretion is controlled by the hypothalamic-pituitary axis. Thyroid Releasing Hormone (TRH) is secreted by the hypothalamic paraventricular nucleus. TRH acts on the anterior pituitary to stimulate the secretion of Thyroid Stimulating Hormone (TSH). TSH acts on the thyroid gland to cause secretion of iodinated thyroglobulin and, if over stimulated, hypertrophy 1. There are many ways in which thyroid hormone release may be suppressed. First among these as a physiological mechanism is the negative feedback action of T3 1. T3 released from the thyroid or synthesized peripherally can act on the anterior pituitary to down-regulate TRH receptors 1. Fasting states and starvation also effectively reduce levels of T3, although levels of T4 and TSH remain within normal levels 5. Cytokines commonly released during infection and illness such as interleukin, interferon and tumor necrosis factor have a complex and not yet totally elucidated role on thyroid function. These cytokines may act to cause a shunting of T4 to inactive rT3 8. Some pharmacological agents commonly used in the ICU setting can also affect thyroid function. Chief among these are the glucocorticoids and dopamine, both of which can cause TSH suppression 4. The dose of glucocorticoid that causes TSH suppression varies depending on the particular steroid used, while dopamine causes suppression when used in doses greater than 1 μg/Kg/min 11. Long-term steroid use does not result in hypothyroidism because the decreased available T4 eventually has a feedback action on the pituitary to return TSH to normal levels 11. 3 2 Actions of Thyroid Hormone Thyroid hormone affects nearly every organ system. Below is a short table highlighting some of the roles that thyroid hormone plays 1: Organ System Bone Central Nervous System Autonomic Nervous System Basal Metabolic Rate Cardiovascular System Respiratory System Metabolic Effects Gastrointestinal Role Promotes bone formation and maturation. Controls the excitability of the CNS. Hyperthyroidism causes hyperexcitability and irritability. Hypothyroidism causes listlessness, slowed speech, somnolence, impaired memory, and decreased mental capacity. Similar to β-adrenergic stimulation. Increased O2 consumption via the sodium-potassium pump and increased heat production in all tissues except brain, gonads, and spleen. Increases in both heart rate and stroke volume Increased ventilation rate (receptors on type II pneumatocytes) Increased glycogenolysis, gluconeogenesis, glucose oxidation, and lipolysis. Both protein synthesis and degradation are increased. Increases GI motility Thyroid Functioning and Critical Illness Changes in the Thyroid Functioning with Illness Thyroid functioning changes with the onset of critical illness. The initial response of the thyroid has been hypothesized to occur with the intention of minimizing energy expenditure so that energy reserves will be available for the body’s vital functions 4. This response has been called “low T3 syndrome” or “euthyroid sick syndrome” and is typified by the thyroid panel results shown below 4. ESS Thyroid Panel Values T3: Low Total Thyroid Hormone: Low T4: Normal/Low TSH: Normal/Low rT3: High Euthyroid Sick Syndrome Abnormal values in the thyroid panel may reflect underlying etiologies reflecting either thyroid disease or illnesses that modify thyroid functioning (sepsis, ACS, etc) 5. ESS falls are of the latter class. These patients do not reflect normal hypothyroidism either clinically (as seen by a decreased basal metabolic rate or a decreased Achilles tendon reflex time) or by other laboratory abnormalities such as increased cholesterol 5. 3 However the diagnosis of ESS may be tricky because some patients in the ICU with nonthyroidal illness (NTI) may have the classic signs of hypothyroidism such as hypotension, dry skin, bradycardia, and hypothermia due to the overlap of symptoms between different clinical diseases 7. ESS is hypothesized to be a change in the normal Hypothalamic-Pituitary-Thyroid Axis (HPTA) “set point” which is actually beneficial during times of illness. This set point change is a homeostatic correction for the disease state of the patient 7. After the illness has past, recovery is seen with an early increase in TSH and then a subsequent increase in T4 and T3 5. No difference in oxygen consumption has been observed during these times of thyroid recovery, which again leads credence to the idea that this is a homeostatic correction to maintain normal state 5. Decreased T3 Decreased T3 may be due to the decreased peripheral conversion of T4, which as discussed above, is the major source of T3 4. The decrease in T3 levels is accomplished by several inhibitory mechanisms that regulate the action of type I iodothyronine-5’deiodinase enzyme 9,12: Increased glucocorticoid levels (either endogenous or exogenous use) Increased levels of free fatty acids Medications such as amiodarone and high doses of propranolol Cytokines such as IL, TNF and IFN Iodinated contrast Decreased T3 results in decreased total protein turnover by the body, thereby conserving energy 4. Similar decreases in T3 are seen with food deprivation at 24-36 hours 7. Starvation has been shown to suppress T3 in the same manner and in fasting participants is related to a decrease in blood urea nitrogen (BUN) 4. Conversely, subsequent administration of exogenous T3 in these participants causes a rapid rise in BUN and so a presumed increase in total protein turnover 4. This is significant since nutritional deficiency and fasting can be normal course for many patients in the first days of an ICU stay before long term nutritional support is initiated. It is reasonable that decreased T3 is a beneficial physiologic response to illness that conserves protein in starvation states. Decreased Total T4 Levels of T4 often remain normal in ESS but can be decreased especially in chronic disease or severe systemic illness 7. T4 is decreased in 50% of patients in the ICU setting 9. Low T4 levels are hypothesized to occur because there is a reduction in T4 protein carriers. The three primary carriers of T4 are thyroxine binding globulin (TBG), transthyretin (TTR) and albumin 9. Low levels of binding protein can also change the free T4 value because the T3-resin uptake test upon which the free T4 value is based fails to adequately correct at very low binding levels 9,12. There is also a concomitant rise in rT3 during critical illness but this is due to decreased clearance of rT3 rather than increased conversion of T4 4. 4 When T4 levels do fall into the low range it may be due to a binding defect to TBG . During critically ill states the amount of TBG does not decrease, but there is an acquired defect in the ability of T4 to bind to TBG 4. Free fatty acids and some medications may play a role in blocking this T4 binding 12. Interestingly, total T4 levels less than 51.6 nmol/L (4ug/dL) have been associated with an increase in mortality 7. 4 Decreased TSH TSH levels can be found in lower than the normal range of values in 15% of hospitalized patients 4. Both the amount of TSH secreted and the pulsatility of that secretion by the anterior pituitary is suppressed by a prolonged critical illness 4. Also, as mentioned above, commonly used ICU medications including dopamine and glucocorticoids can suppress TSH secretion 4. That having been said, TSH levels rarely fall below 0.01 mU/L at which point they should be considered to represent frank thyrotoxicosis 4. The level 0.01 mU/L is significant because it is the threshold below which TSH is undetectable by third generation TSH laboratory tests 9. 75% of patients with undetectable TSH levels on these tests have hyperthyroidism 9. Thyroid Supplementation in Critical Care Patients I have been slightly biased in my presentation of abnormal thyroid values as “normal” homeostatic correction. There are many clinicians concerned that thyroid dysfunction in our sickest patients is an untreated illness. And they are rightly concerned, as a direct correlation has been shown between the lowest thyroid T3 levels and poor outcome in critically ill patients 5. It can be argued that many ICU patients have been pushed beyond the boundaries of their physiologically adaptive mechanisms, and so the drop in thyroid hormone values is not adaptive but an attenuation of what should be the patient’s ability to maintain hormone values within normal range 7. Others have cautioned against the use thyroid supplementation. If low T3 is a mechanism to spare protein turnover as has been proposed, then iatrogenically raising a patient’s T3 may lead to increased protein turnover and thereby impaired muscle function (with special concern for respiratory muscle function) 5. Others have stated that the idea of treating ESS with levothyroxine is futile because exogenous T4 will be shunted to rT3 8 . Lastly, supplementing thyroid hormone in critically ill patients has been shown to prolong the depression of TSH levels during the recovery phase when they should rebound 4. As of yet, there have been no studies demonstrating improved outcomes by treating ESS 12. Randomized trials have been performed with burn patients, patients in the ICU, and patients immediately post-CABG 9. None of these studies has shown that thyroid hormone replacement was beneficial (there was a transient increase in cardiac index in the post-CABG study) 9. Thyroid hormone replacement may be beneficial only in cases of true hypothyroidism and not in ESS. Testing for Thyroid Dysfunction During Critical Illness Because of the alterations in the normal thyroid set point during periods of illness and the ambiguity associated with interpretation of thyroid panels during critical illness, thyroid tests should be ordered only when there is a clinical suspicion of thyroid disease 5 9 . ESS also complicates the picture in that a TSH measurement alone is not sufficient for assessing thyroid function 9. When thyroid function needs to be assessed in the ICU, a full thyroid panel is recommended including TSH, total T4, free T4, and a T3 9. Interpretation of The Thyroid Panel in the Face of NTI So your overly enthusiastic intern ordered, unbeknownst to you, a thyroid panel on an ICU patient and the results have just come back. The problem now becomes one of deciding how the thyroid hormone values should be interpreted in this critically ill patient. What values can be considered “normal” for critically ill patients even if they fall outside the normal range for a healthy patient? The answer to the challenge of the ICU patient with an abnormal thyroid panel is determining whether or not there is “true” thyroid illness 7. Although there is a correlation between dysfunctional thyroid levels in NTI and increased mortality, there has been no proof of a causal link between them. And thyroid supplementation has not yet yielded improvements in outcome in NTI. So separating out NTI from thyroidal illness is key to the interpretation and management of thyroid hormone levels in the ICU. Important Thyroid Panel Values in the ICU TSH < 0.01 mU/L are indicative of true hyperthyroidism TSH > 20 mU/L are indicative of true hypothyroidism T3:T4 ratio of > 100 is indicative of true hypothyroidism TSH A normal TSH level is a reassuring finding in an ICU patient. A TSH within the range of normal essentially negates the diagnoses of thyrotoxicosis and hypothyroidism regardless of the T3/T4 levels 7. A low TSH suggests ESS but, as has been stated before, levels lower than 0.01 mU/L are rarely seen in ICU patients and more indicative of true thyroid dysfunction. Levels below normal but still above 0.01 mU/L need further corroborating clinical and laboratory evidence to implicate hyperthyroid disease. As patients recover from NTI, suppressed levels of TSH will begin to rise. The TSH level may even over-correct for a time and be above the range of normal (0.4 – 4.8 mIU/L) 7. TSH has been shown to increase as high as 20 mU/L in the recovery phase of NTI, but in general TSH will only rarely over-correct to above 10 mU/L 9. For TSH values greater than 10 mU/L, an attempt should be made to correlate it to physical symptoms of hypothyroidism and to parallel decreases in T4 and T3. TSH values, especially those in the intermediate range of 5 to 20 mU/L, can also be repeated over the course of several days to establish a trend 7. Patients with TSH values greater than 20 mU/L generally have hypothyroidism that will not self-correct and will need thyroid supplementation and follow-up thyroid function tests 7. 6 T3 and T4 Although T3 is not a good screening tool for thyroid disease in the outpatient setting, it is useful for differentiating NTI from hyperthyroidism in the critical care setting 9. In NTI, T3 will be low-normal as has been discussed above. In hyperthyroidism, T3 will most likely be high 9. Total T4 may be decreased in ESS, but free T4 remains normal or may even increase 12. Also, the T3:T4 ratio may help differentiate NTI from hypothyroidism. A ratio of T3:T4 that is greater than 100 is suggestive of hypothyroidism over NTI 7. Other Laboratory Values rT3 can be measured to differentiate NTI (in which it is increased due to decreased clearance) and central hypothyroidism (in which it is low due to low levels of its T4 substrate) 9. It has been suggested that a pituitary panel can also be considered in low TSH states to evaluate the integrity of the HPA 7. One must bear in mind though that the gonadal axis and other hormones are often also suppressed during states of critical illness and this may falsely lead to a diagnosis of central HPA disease that does not exist 12 . Other Clinical Factors In the art of medicine, one should never forget to use common sense along with laboratory values. Before acting on abnormal thyroid panel values a simple medication review should be performed to look for medications that may be disrupting thyroid functioning. A history should be obtained from the patient or family to search for prior diagnosed thyroid disorders or recent undiagnosed thyroid symptoms. Lastly, an attempt to clinically correlate the patient’s condition to the lab values should be made. Is the patient have unexplained arrhythmias? Are they bradycardic? Has the patient been hyper or hypothermic? Are there any physical exam findings that corroborate thyroid dysfunction? Conclusions Thyroid abnormalities are the norm during critical illness although whether this is a homeostatic correction or part of the illness is debatable. Thyroid hormone supplementation has not been shown to improve outcomes in critically ill patients with non-thyroid disease. The index of suspicion for thyroid disease should be high before deciding to order thyroid function tests and the results of these tests need to be examined carefully according to the patient’s situation. References 1. Costanzo, Linda. Board Review Series Physiology (2nd Edition). Baltimore, MA: Lippincott Williams & Williams. 2. http://www.myoops.org/cocw/tufts/courses/14/content/D265882/C82210.jpg 3. http://www.bmb.leeds.ac.uk/teaching/icu3/lecture/25/index.htm 4. Ligtenberg J.J.M. Hormones in the Critically Ill Patient: To Intervene or Not to Intervene. Intensive Care Med 2001; 27:1567-1577 7 5. Stathatos, Nikolaos. The Controversy of the Treatment of Critically Ill Patients with Thyroid Hormone. Best Practice and Research Clinical Endocrinology and Metabolism 2001; 15(4): 465-478 6. Holcomb, Susan. Thyroid Diseases: A Primer for the Critical Care Nurse. Dimensions In Critical Care Nursing 2002; 21(4): 127-133. 7. Nylen, ES. Endocrine Changes in Critical Illness. Journal of Intensive Care medicine 2004; 19: 67-82. 8. Wyne, Kathleen. Commentary: The role of Thyroid Hormone Therapy in Acutely Ill Cardiac patients. Critical Care 2005; 9:333-334 9. UpToDate: Thyroid Function in Nonthyroidal Illness. 10. Gardener, David. Greenspan’s Basic and Clinical Endocrinology (8th Edition). The McGraw-Hill Companies. 11. Surks M. Drugs and Thyroid Function. The New England Journal of Medicine 1995; 333(25):1688-94. 12. Sakharova, Olga. Endocrine Assessments During Critical Illness. Critical Care Clinics 2007; 23: 467-490. 8