Notes
advertisement

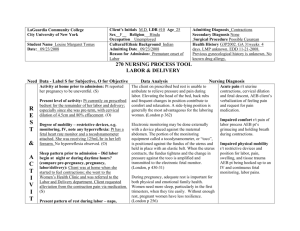
Notes Complications of Labor and Delivery The successful completion of the 40 week gestational period requires the harmonious functioning of four components: Psyche, Powers, Passenger, Passageway. A disruption in any of these components may cause DYSTOCIA. Dystocia is an abnormal, long, or difficult labor or delivery. Complications of the Psyche Hormones released in response to anxiety or stress can cause DYSTOCIA. Sources of stress vary for each individual, but pain and the absence of a support person are the two most common factors. Intense anxiety stimulates the Sympathetic nervous system which in turn releases catecholamines which lead to myometrial dysfunction. Norepinephrine and epinephrine lead to uncoordinated or increased uterine activity. Nursing Care: 1. Assess support available and be there for the patient 2. Patient Teaching on breathing and relaxation measures 3. Non-Pharmacological and Pharmacological Measures 4. Keep informed of progress 5. Provide quiet calm environment Complications of the Powers Uterine Dysfunction Uterine dystocia’s occur when labor contractions (powers) are ineffectual, erratic or unable to do the work of dilation and effacement of the cervix. I. HYPERTONIC UTERINE CONTRACTIONS Most often occur in first-time mothers, primigravidas. The contractions are uncoordinated, involve only a portion of the uterus, and are ineffective B they do not bring about dilation and effacement. The contractions increase in frequency, but the intensity is decreased. Signs and Symptoms: 1. PAINFUL contractions RT uterine muscle anoxia, causing constant cramping pain. 2. Dilation and effacement the cervix does not occur. 3. Prolonged latent phase. Stay at 2 - 3 cm. - don’t dilate as should. 4. Fetal distress occurs early – uterine resting tone is high; decreasing placental perfusion. 5. Anxious and discouraged Goal: Relieve pain and promote normal labor pattern Treatment of Hypertonic Uterine Contractions: 1. Provide with COMFORT MEASURES and Therapeutic Rest Warm shower Mouth Care Imagery Music Back rub 2. Mild Sedation or some analgesics 3. Bedrest - allow to sleep and when awakens uterine contractions may be normal 4. Hydration 5. Tocolytics to reduce high uterine tone II. HYPOTONIC UTERINE CONTRACTIONS B UTERINE INERTIA Most often occurs in the multigravida patient. Labor starts out normal and progresses through the latent phase. Once the patient reaches the active phase there is marked slowing of contractions (2 - 3 contractions in 10 minutes). The uterus is indentable even at acme of contraction. Etiology and Pathophysiology: 1. Overstretching of the uterus - large baby, multiple babies, polyhydramnios, multiple parity 2. Bowel or bladder distention preventing descent 3. Excessive use of analgesia / anesthesia Assessment: Signs and Symptoms of HYPOTONIC UTERINE INERTIA: 1. Weak contractions, infrequent and brief, and can be easily indented with fingertip pressure at peak 2. Prolonged ACTIVE Phase 3. Exhaustion of the mother 4. Psychological trauma - frustrated Intervention: Treatment of Hypotonic Uterine Inertia: 1. Ambulation 2. Nipple Stimulation - release of endogenous Pitocin 3. Enema - warmth of enema may stimulate contractions 4. Amniotomy - artificial rupture of the membranes 5. Augmentation of labor with the use of Pitocin AMNIOTOMY I. Advantages of doing this before Pitocin Contractions are more similar to those of spontaneous labor Usually no risk of rupture of the uterus Does not require as close surveillance II. Disadvantages of an Amniotomy Delivery must occur Increase danger of prolapse of umbilical cord III. Nursing Care: #1-Check the fetal heart tones Assess color, odor, amount Provide with perineal care Monitor contractions Check temperature every 2 hours PITOCIN I. Induction of Labor – Bishop’s Score II. Augmentation of Labor Use only if CPD (cephal pelvic disportion) is not present Give 20 units/1000 cc. fluid or 30 units/500 cc fluid. Hang as a secondary infusion, never as primary GOAL: Achieve contractions every 2 - 3 minutes of good intensity with relaxation between Nursing Care: 1. Assess contractions - are they increasing but not tetanic 2. Assess dilation and effacement 3. Monitor vital signs and FHT’s III. PROLONGED LABOR A labor lasting more than 18 - 24 hours Cervical dilations (Primigravida 1.2 cm/hr Multigravida 1.5 cm/hr) Descent of fetus should be 1 cm/hr. primigravida; 2 cm/hr in multigravida Etiology: CPD - Cephalo Pelvic Disportion Malpresentation, malposition Labor dysfunction Therapeutic Interventions: Depends on the cause: 1. Comfort measures 2. Conservation of energy 3. Psychological support 4. Position changes 5. Pitocin augmentation IV. PRECIPITOUS LABOR OR DELIVERY A precipitous labor is one that lasts less than 3 hours. A precipitous delivery is an unexpected fast delivery B many times outside of a sterile environment. Etiology: Lack of resistance of maternal tissue to passage of fetus Intense uterine contractions Small baby in a favorable position Complication: 1. If the baby delivers too fast, does not allow the cervix to dilate and efface which leads to cervical lacerations 2. Uterine rupture 3. Fetal hypoxia and fetal intracranial hemorrhage Nursing Care in a Rapid Delivery - Delivery Outside Normal Setting Everything is OUT OF CONTROL! The patient is frightened, angry, feels cheated 1. 2. 3. 4. 5. 6. 7. 8. Do NOT leave the mother alone - stay with her and provide reassurance. Try to make the place clean, (don’t break down table) place something clean under her hips. Try to get the mother in control - Have mom pant or blow out to decrease the urge to push. Apply gentle pressure to the fetal head as it crowns to prevent rapid change in pressure in the fetal head which can cause subdural hemorrhage or dural tears. Deliver the baby BETWEEN contractions to control delivery. Suction or hold baby’s head low, tie off the cord, and place on mom’s abdomen. Massage the uterus. Allow to breast feed. Document! Complications of the Passageway Pelvic Dystocia Pelvic Inlet or Outlet is not of sufficient size or proper shape to allow the baby to get through. Etiology: Congenital defect; Malnutrition (Rickets); Neoplasms; Fracture/Trauma. Assessment: Signs and Symptoms: Labor is arrested. Station does not decrease. It remains the same. Therapeutic Interventions: Cesarean delivery Complications of the Passenger Malpositions: Posterior position - usually mom complains of back pain Treatment: 1. Forceps - low forceps or outlet forceps usually applied after crowning 2. Vacuum extraction - disk shaped cup placed over vertex of head and vacuum applied 3. Episiotomy - surgical incision to allow more room Malpresentation: brow, face, transverse, breech Treatment: 1. May allow to deliver vaginally with caution or C-birth 2. Version B alteration or turning of the fetus to alter the position by abdominal or intrauterine manipulation External version - attempt to turn the fetus from a breech to a vertex presentation Internal version - physician inserts a hand into the uterus and changes the presentation to cephalic. Used to deliver the second fetus in the case of twins. Cephalopelvic Disproportion: Large baby or small pelvis. It is usually diagnosed when there is an arrest in descent. Station remains the same. Therapeutic Interventions: Cesarean Delivery Multiple Fetuses: May be delivered by cesarean birth CESAREAN DELIVERY An operative procedure in which the fetus is delivered through an incision in the abdomen. Remember - It is a Birth! Mom may feel less than normal, so may need support May have option of a VBAC (Vaginal Birth After Cesarean) the next time Premature Rupture of the Membranes Definition: Spontaneous rupture of the membranes before labor begins. Etiology and Pathophysiology: 1. Infections 2. Fetal abnormalities 3. Incompetent cervix 4. Recent sexual intercourse Major risk: 1. Ascending intrauterine infection 2. Precipitation of labor Therapeutic Interventions: Treatment and Nursing Care: 1. Wait and watch, bedrest, no intercourse, shower only, no tub baths 2. Betamethasone / Celestone B provides stressor to the lungs of the fetus to stimulate production of surfactant 3. Assess time membranes ruptures and if labor started 4. Check temperature frequently. Every 4 hours while awake. Report an increase of 100.4 5. Describe character of amniotic fluid and report foul smelling or increase in amount 6. Check WBC 7. Provide psychological support Preterm Labor Definition: Labor that occurs after 20 weeks but before 37 weeks. Etiology: Most common causes: urinary tract infections and premature rupture of membranes. Therapeutic Interventions: Goal : STOP THE LABOR! Suppression of uterine activity a. Drug Therapy – Tocolytics (beta-adrenergic) Uses: stop/arrest labor. Criteria for use – Do not give if: 1. Patient is in active labor, cervix has dilated to 4 cm. or more 2. Presence of severe pre-eclampsia 3. Fetal complication / fetal demise 4. Hemorrhage is present 5. Membranes have ruptured\ Side effects: 1. Palpitations 2. Tachycardia 3. Tremors, nervousness 4. Headache 5. Hyperglycemia Toxic effects: 1. PULMONARY EDEMA – noted upon routine chest assessments of rales and dyspnea. 2. Antidote: Inderal (beta-blocker) b. NURSING CARE: 1. Teach how to take medication on time 2. Teach patient to check pulse, call Dr. if > 120 - 140 3. Teach to assess fetal movement daily, kick counts 4. Drink 8 - 10 glasses of water/day 5. Monitor uterine activity. 6. Decrease activity; lie on side 7. Keep bladder empty. 8. Pelvic rest. Ruptured Uterus Definition: Spontaneous or traumatic rupture of the uterus Etiology: 1. Rupture of a previous C-birth scar 2. Prolonged labor 3. Injudicious use of Pitocin 4. Excessive manual pressure applied to the fundus during delivery Signs and Symptoms: Sudden sharp abdominal pain, abdominal tenderness Cessation of contractions Absence of fetal heart tones Shock Therapeutic Interventions: Deliver the baby! / Cesarean delivery Prolapse of the Umbilical Cord Definition: Prolapse of the umbilical cord through the cervical canal along side of the presenting part. Etiology: Occurs anytime the inlet is not occluded. Fetus is not well engaged. Occurs with rupture of membranes. Goal: Relieve the pressure on the cord to maintain oxygenation of the fetus Support the mother and the family Therapeutic Interventions: 1. Get the pressure off the Cord - place in trendlenberg or knee-chest position OR elevate part with sterile glove. Must have pulsating cord. 2. Palpate FHT’s, NEVER ATTEMPT TO REPLACE CORD! 3. Give O2 per mask - 10 - 12 liters 4. Cover exposed cord with sterile wet gauze 5. Stay with the patient and offer support Amniotic Fluid Embolism Definition: Escape of amniotic fluid into the maternal circulation. It usually enters maternal circulation through open sinus at placental site. Usually fatal to the mother because amniotic fluid contains debris, lanugo, verni, meconium, etc. Signs and Symptoms: dyspnea chest pain cyanosis shock Therapeutic Interventions: Deliver the baby Provide cardiovascular and respiratory support to Mom ICU