Is Histamine not involved in the pathophysiology of burn induced
advertisement
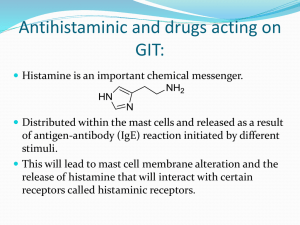
Is Histamine not involved in the pathophysiology of burn induced vascular dysfunction in humans? Joakim Johansson1, M.D., Emanuel Bäckryd1, M.D., Göran Granerus2 M.D., Birgitta Lönnqvist2 Engineer, Folke Sjöberg 1,3, M.D., Professor. Departments of Anesthesiology and Intensive Care1, Clinical Physiology2 and the Burns unit, Hand and Plastic Surgery3. Short title: Adress correspondance to: Joakim Johansson, M.D. Department of Anesthesiology and Intensive Care, Östersund Hospital SE 83183 SWEDEN Phone: + 46 63 153000 Fax: + 46 63 154501 e-mail: joakim.johansson@jll.se Abstract The increased amount of extravascular water following burns is thought to contribute to morbidity and mortality because it interferes with gas exchange in the lungs and tissue healing. There has been much effort made to explore the underlying pathophysiological mechanism that generates increased vascular permeability following burns. Many different substances have been proposed as mediators of witch histamine is one. The reason for this is that early work showed evidence of increased histamine plasma-concentrations and animal models pointing at histamine as the mediator. Modern clinical studies investigating the possible role of histamine as a mediator of postburn increased vascular permeability are lacking. Therefore we investigated urine-levels of histamine and metylhistamine following major burns in 8 patients. We found no increase in urine excreation levels of histamine or its metabolite methylhistamine even though the patients showed the characteristic signs of increased vascular permeability. We conclude that this is evidence for histamine not being a mediator of increased vascular permeability following burns in non burned areas. This study can not however exclude histamine as a local mediator in burned areas. Key words: burn, histamine, mediator, oedema, vascular permeability Introduction Extensive thermal injuries result in a massive inflammatory response with both local and systemic effects which, if not alleviated, may lead to burn shock [1-3]. To be able to reduce these deleterious effects of the inflammatory reaction, it is vital to understand the basic pathophysiological mechanisms involved. Histamine is one of the classical mediators of inflammation. Mast cells, which together with basophils store most of the histamine in humans, are present in loose connective tissue, especially around blood vessels. Mast cells are very abundant in the skin, the dermis containing 3000 - 12 000 mast cells per cubic millimetre[4]. Different stimuli can induce mast cell degranulation and subsequent release of histamine such as: mast cell IgE-stimulation by antigen; anaphylatoxins; several interleukins; physical stimuli like heat and cold; free radicals; and others [4-6]. Histamine mediates its effect through three classes of receptors: H1, H2 and H3. H1 receptors are present in, among other tissues, endothelial cells, and, when stimulated induce (a): the contraction of endothelial cells, leading to the formation of gap junctions and subsequent increased vascular permeability and (b): the release of nitric oxide, prostacyclin and other factors, leading to vasodilatation[4, 7, 8]. Vascular smooth muscle contains both H1 and H2 receptors who mediate constriction and dilatation, respectively [4, 8]. However, the net effect of histamine upon the vascular tone in skin seems to be predominantly vasodilatory [4]. Moreover, histamine induces recruitement of leukocytes to sites of inflammation [5] and seems to enhance the catalytic activity of xanthine oxidase, witch may lead to enhanced synthesis of oxygen free radicals [9]. Histamine is considered to be an important mediator of burn induced vascular dysfunction, especially in its early phase [1]. However, most of this assumption is based on animal experimental models [6, 10]. Consistent data in humans are lacking [11, 12]. Results from animal experiments may not apply to humans for different reasons, especially when considering the inter- and intraspecies heterogeneity of different mast cell subpopulations [13]. This study aimed at describing the metabolism of histamine in humans during the first 48 hours after a moderate to major burn. Patients and Methods The study was conducted at a tertiary referral university hospital in Linköping, Sweden at a specialised Burn intensive care unit. Consecutively admitted patients were included. In order to evaluate histamine metabolism, it is mandatory to measure levels of histamine metabolites in addition to histamine. Urinary levels of histamine and methylhistamine were therefore measured in 8 patients during the first 48 hours at the burn unit. Moreover, in one case, leves of methyl imidazole acetic acid were measured. On admission, the bladder was emptied (”pre-admission” urine). The urine was then collected every 6 hrs for two days. Upon collection, the urine was immidiately acidified and the volume carefully measured. A sample was kept and frozen. The samples were later analysed by reversed phase ion-pair High Performance Liquid Chromatography (HPLC) [14, 15] at the department of Clinical Physiology, Linköping University Hospital. The excretion levels were compared to a healthy control group (n=20) from an earlier study of co-worker Granerus [16] using the same method. The urinary excretion of creatinine was also determined for each sample. Histamine and methylhistamine levels were then normalized for creatinine excretion, thereby correcting for differences in body size. Moreover, in 6 patients, day 1 creatinine clearance was determined. Results The mean extent of the burn (Total Burn Surface Area) was 23%, 11-37 (median, range), with no mortality. For further patient data, see Table 1. Pat 1 Pat 2 Pat 3 Pat 4 Pat 5 Pat 6 Pat 7 Pat 8 Gender (M/F) Age (years) Weight 0- TBSA (%) 24 hrs postadmiss ion (kg) Transport time to burn unit (h) M M M F M F M F 43 50 44 13 89 52 9 75 121 60 103 59 75 64 36 * 20 * 13 3,5 8 5 10 4 30 11 23 32 14 24 37 17 Time from admission to operation (h) 18 19 11 15 16 10 15 15 Mode of injury Scald Flame Scald Flame Flame Flame Flame Flame * No data Table 1. Patient data. The urinary excretion of histamine per 6 hours is shown in figure 1. Initially (0 – 18 hrs postadmission), the urinary levels of histamine were normal. During the period 18 – 30 hrs postadmission, there were increased variation in histamine-levels. This was largely dependent on patient 1, whose histamine-levels were largely increased in these samples. For the remaining observation period, we also found normal levels. There were no statistically significant variation in histamine-levels within the patient group as tested with Kendalls coefficient of concordance. The same result was obtained regardless of whether or not patient 1 was considered a statistical outlier. Further, when levels were compared to healthy controls there were still no statistically significant variation to be found. The urinary excretion per 6 hours of methylhistamine is shown in figure 2. There were no significant changes over time within the patient group and no significant changes as compared to healty controls. In Patient 1, the excretion of methyl imidazole acetic acid was also determined and was found to be within normal range (data not shown). To further investigate the possibility of an early large release of histamine immediately post-burn, we also determined levels of histamine and methylhistamine in ”pre-admission” urine; these levels were not substantially elevated in comparison to healthy controls (data not shown). Hence, we found no direct evidence of an early systemic release of histamine immediately post-burn. In 6 of the patients, we were able to calculate endogenous creatinine clearance at some point during day 1. 4 patients had a moderatly lowered creatinine clearance (range 60 – 76 mL/min). Patient 5 had a very low clearance (28 mL/min); this patient was 89 years old. Only Patient 1 had a good clearance (182 mL/min). Hence, despite adequate resuscitation and good diuresis, the renal function does not seem to be optimal during day 1 post-admission. The dynamics of u-creatinine adjusted histamine and metylhistamine are shown in figure 3 and 4 respectively. According to Kendalls coefficient of concordance there were no statistically significant variation in the two variables during the time-period studied. Discussion The interest in the role of histamine in burns has a long history. In 1936, Barsoum and Gaddum showed high and rising blood-histamine levels for days after a major burn [17]. Since then, histamine has been considered to play an important role in the pathophysiology of burns, especially in the early phase of postburn oedema [1]. Histamine is known to be potently vasoactive, as manifested by its alleged role in anaphylaxis [18]. Hence, as animal experimental models have shown that histamine is released into the plasma after a burn [9, 10], it is reasonable to hypothesize that histamine is being released from human burned skin and may play a role in systemic burn induced vascular dysfunction. However, evidence in humans is conflicting. In 1957, Birke et al demonstated high urine postburn levels of histamine in humans[12], whereas Agrup and coworkers failed to confirm this [11]. Hence, conclusive evidence for a huge release of histamine from human skin postburn is at best scarce. Results from administration of systemic antihistamines postburn are conflicting. While the H2antagonist cimetidine reduces postburn oedema in animals [9, 19, 20], another H2-antagonist (ranitidine) does not [21]. It is therefore likely that non H2-receptor dependent effects of cimetidine are at work, e.g hydroxyl radical scavenging [9] or SOD-like activity, e.g. [21]. Antihistamine treatment aiming at reducing vascular leak are tested and found not effective [ref]. In all modern intensive care facilities however, pharmacological stress-ulcer prevention is standard of care. Proton-pump inhibitors are the most often used drugs but histamine-blockers may also be used for this purpose. In this study, histamine metabolism was studied by measuring the excretion of histamine and methylhistamine (a metabolite of histamine), and in one case methylimidazole acetic acid, into the urine. As histamine is rapidly cleared from the plasma, urinary output levels is the most reliable way to study histamine metabolism [18]. The kidney removes histamine from plasma very effectively, the renal extraction ratio being aproximately 80% [22, 23]. Moreover, the kidney has capacity to metabolise histamine. Only a few percent are excreted unchanged in the urine [16, 18, 22, 24]. Consequently, to be able to evaluate histamine metabolism, it is mandatory to measure levels of histamine metabolites in addition to histamine. Urinary excretion of histamine and metylhistamine, as well as most other excretion products, are affected by the fact that burn-patients experience extreme alterations in water content in different body compartements. This alterations affects most of all the extracellular space with is expanded following burns due to the large amount of intravenous fluids that must be administered during the first 24 hours. The volume of distribution of all solutes in the body is hence increased. If patients are resuscitated according to the Parkland formula, witch is the most common method to guide the initial fluid therapy, they often gain 10-15 % of body weight [behövs ref?, Folke] during the first 24-48 hours. This was also true for our patients (redovisas eller ej, Folke?). During the following days of intensive care it is common with an increased urine-production to restore water hoemostasis. If there were an alteration in histamine- or metylhistamine-metabolism it may be masked by these changes in water physiology. Urinary excretion of creatinine is known to follow the excretion of histamine and metylhistamine. To be able to compensate for the effect of altered water physiology we also analysed urinary creatinine for every patient in every 6 hour-fraction of urine. We were then able to calculate the fraction of excreted histamine/metylhistamine per amount of excreted creatinine. This is the u-creatinine adjusted histmine and metylhistamine levels respectively. Histamine can be synthezied in the kidney [25, 26]. Some studies suggest that the major source of urinary histamine may be de novo synthesis in the kidney [25]. There was a tendency for increased urinary histamine and metylhistamine during the study period. This tendency was seen largely because of patient #1 who showed a large increase. With his data considered as statistical outliers there was no tendency at all for a dynamic change in either histamine or metylhistamine during the first 48 h after admittance. The patients were operated on 10 to 19 h after arrival. It can not be excluded that the trauma of operation could lead to the second-day output of histamine seen in some of the patients, and seen in other earlier studies, especially when considering that some drugs used in the perioperative period (and also in the intensive care setting) can induce histamine release [27]. As described above, the bladder was emptied on admission. The content of histamine and methylhistamine was analyzed in this sample as well. Due to the great range of transport time to the Burns Unit (see Table 1) and due to uncertainty in urine collection during that period, it is difficult to compare the excretion pre-admission. Nevertheless, there is no evidence of a huge release of histamine during the pre-admission period (data not shown). Other proposed mediators of increased vascular permeability following burns are serotonin, prostaglandins and oxygen radicals, as reviewed by Arturson [1]. Most data rely on animal studies and follow up in humans have not been convincing with regard to the involvement of the respective proposed mediator. In recent years, increasing interest has been shown leukocytes and the products released by them following severe physiological challenges such as burns, trauma and sepsis [28, 29]. Our group has recently shown that neutrophils release heparin binding protein (HBP) following burns [in press]. HBP has, in preclinical models, been shown to alter vascular permeability [30, 31] In conclusion; This study could not confirm a release of histamine from burned skin 0-48 hours after a modrate to major burn. We conclude that histamine is unlikely to mediate the increased vascular permeability in non burned tissues following burns. This study, however, can not exclude a role for histamine as a local mediator of increased vascular permeability in burned areas. 100 80 60 histamine 40 20 0 ctrl 6-12 h 18-24 h 30-36 h 42-48 h 0-6 h 12-18 h 24-30 h 36-42 h time of urine sampling post-burn Mean Mean±SE figure 1. Urinary histamine-levels in 8 burned patients compared to healthy controls. No significant variation over the time period studied or compared to control-levels. Mean and standard error of the mean (SEM). 140 120 100 80 60 metylhistamine 40 20 0 ctrl 0-6 h 6-12 h 18-24 h 30-36 h 42-48 h 12-18 h 24-30 h 36-42 h Mean Mean±SE time of urine sampling post-burn Figure 2 Urinary metylhistamine-levels in 8 burned patients compared to healthy controls. No significant variation over the time period studied or compared to control-levels. Mean and standard error of the mean (SEM). Mean; Box: Mean±SE 300 250 200 150 100 u-creatinine adjusted histamine 50 0 0-6 h figure 3 (alternativ 1) 12-18 h 24-30 h 36-42 h 6-12 h 18-24 h 30-36 h 42-48 h time of urine sampling post-burn Mean Mean±SE 900 800 700 600 500 400 300 u-creatinine adjusted histamine 200 100 0 0-6 h 12-18 h 24-30 h 36-42 h 6-12 h 18-24 h 30-36 h 42-48 h Median 25%-75% Outliers Extremes time of urine sampling post-burn figure 3 (alternativ 2) U-creatinine adjusted histamine-levels in 8 burned patients. No significant variation over the time period studied. 600 500 400 300 200 u-creatinine adjusted metylhistamine 100 0 0-6 h 12-18 h 24-30 h 36-42 h 6-12 h 18-24 h 30-36 h 42-48 h Mean Mean±SE time of urine sampling post-burn figure 4 (alternativ 1). U-creatinine adjusted metylhistamine-levels in 8 burned patients. No significant variation over the time period studied. 700 600 500 400 300 200 u-creatinine adjusted metylhistamine 100 0 0-6 h 12-18 h 24-30 h 36-42 h 6-12 h 18-24 h 30-36 h 42-48 h Median 25%-75% Outliers Extremes time of urine sampling post-admittance Figure 4 alternativ 2 References 1. 2. 3. 4. 5. 6. 7. 8. 9. Arturson G. Pathophysiology of the burn wound and pharmacological treatment. The Rudi Hermans Lecture, 1995. Burns 1996;22:255-74. Youn YK, Lalonde C, and Demling R. Oxidants and the pathophysiology of burn and smoke inhalation injury. Free Radic Biol Med 1992;12:409-15. Gibran NS and Heimbach DM. Mediators in thermal injury. Semin Nephrol 1993;13:344-58. Atkinson TP WM, Kaliner MA, Histamine and Serotonin. In: Gallin JI GI, Snyderman R, Inflammation: Basic Principles and Clinical Correlates. ed, New York: Raven Press, Ltd; 1992. p. 193-209. Kubes P and Granger DN. Leukocyte-endothelial cell interactions evoked by mast cells. Cardiovasc Res 1996;32:699-708. Metcalfe D, Mast Cell Activation. In: Mast Cells. Physiol. Rev. ed, 1997. p. 1044-1050. Ehringer WD, Edwards MJ, and Miller FN. Mechanisms of alpha-thrombin, histamine, and bradykinin induced endothelial permeability. J Cell Physiol 1996;167:562-9. Chiba S and Tsukada M. Mechanisms for histamine H1 receptor-mediated vasodilation in isolated canine lingual arteries. Eur J Pharmacol 1997;329:63-8. Friedl HP, Till GO, Trentz O, and Ward PA. Roles of histamine, complement and xanthine oxidase in thermal injury of skin. Am J Pathol 1989;135:203-17. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. Yurt RW and Pruitt BA, Jr. Base-line and postthermal injury plasma histamine in rats. J Appl Physiol 1986;60:1782-8. Agrup P, Graneurs G, Jacobsson S, Wetterqvist H, and White T. Histamine metabolism in burn injuries. Scand J Plast Reconstr Surg 1974;8:198-201. Birke G DH, Liljedahl S-O, Pernow B, Plantin L-O, Troell L. Histamine, catecholamines and adrenocortical steroids in burns. Acta Chir Scand 1957;114:87-98. Church MK, el-Lati S, and Okayama Y. Biological properties of human skin mast cells. Clin Exp Allergy 1991;21 Suppl 3:1-9. Granerus G, Current Techniques of Histamine Determination: Determination by High-Performance Liquid Chromatography. In: Uvnäs B, Handbook of Experimental Pharmacology, Vol. 97. ed, Springer-Verlag; 1991. p. 49-57. Granerus G and Wass U. Urinary excretion of histamine, methylhistamine (1-MeHi) and methylimidazoleacetic acid (MeImAA) in mastocytosis: comparison of new HPLC methods with other present methods. Agents Actions 1984;14:341-5. Granerus G. Urinary excretion of histamine, methylhistamine and methylimidazoleacetic acids in man under standardized dietary conditions. Scand J Clin Lab Invest Suppl 1968;104:59-68. Barsoum GS GJ. The effect of cutaneous burns on the blood - histamine. Clinical Science 1936;2:357-362. Kaliner M, Shelhamer JH, and Ottesen EA. Effects of infused histamine: correlation of plasma histamine levels and symptoms. J Allergy Clin Immunol 1982;69:283-9. Boykin JV, Jr., Eriksson E, Sholley MM, and Pittman RN. Histamine-mediated delayed permeability response after scald burn inhibited by cimetidine or cold-water treatment. Science 1980;209:815-7. Tanaka H, Wada T, Simazaki S, Hanumadass M, Reyes HM, and Matsuda T. Effects of cimetidine on fluid requirement during resuscitation of third-degree burns. J Burn Care Rehabil 1991;12:425-9. Boykin JV, Jr. and Manson NH. Mechanisms of cimetidine protection following thermal injury. Am J Med 1987;83:76-81. Helander CG, Lindell SE, and Westling H. The renal removal of C-14-labelled histamine from the blood in man. Scand J Clin Lab Invest 1965;17:524-8. Lindell SE and Schayer RW. The renal removal of injected [14C] histamine from the blood in dogs. Br J Pharmacol Chemother 1958;13:44-51. Cooper JA and Schayer RW. Metabolism of C14 histamine in man. J Appl Physiol 1956;9:481-3. Abboud HE and Dousa TP. Renal metabolism and actions of histamine and serotonin. Miner Electrolyte Metab 1983;9:246-59. Lindell SE and Schayer RW. Formation of histamine in the kidney of the dog. Br J Pharmacol Chemother 1958;13:89-90. Moss J and Rosow CE. Histamine release by narcotics and muscle relaxants in humans. Anesthesiology 1983;59:330-9. Talbott G, Sharar S, Harlan J, and Winn R. Leukocyte-endothelial interactions and organ injury: the role of adhesion molecules. New Horiz 1994;2:545-54. Brown KA, Brain SD, Pearson JD, Edgeworth JD, Lewis SM, and Treacher DF. Neutrophils in development of multiple organ failure in sepsis. Lancet 2006;368:157-69. Gautam N, Olofsson A, Herwald H, Iversen F, Lundgren-Akerlund E, Hedqvist P, et al. Heparin-binding protein (HBP/CAP37): a missing link in neutrophil-evoked alteration of vascular permeability. Nat Med 2001;7:1123-7. Herwald H, Cramer H, Morgelin M, Russell W, Sollenberg U, Norrby-Teglund A, et al. M protein, a classical bacterial virulence determinant, forms complexes with fibrinogen that induce vascular leakage. Cell 2004;116:367-79.