2012 Medical Student Scholarship Winner – Christina Sarris
advertisement
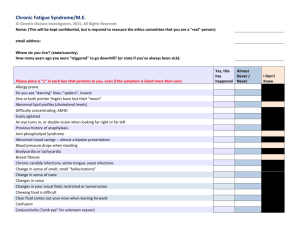
Christina Sarris 2012 Medical Student Scholarship Winner Enumerate the various possible causes of Chronic Fatigue Syndrome (also referred to as Myalgic Encephalomyelitis). Discuss the evidence for and against these causes. Introduction Feelings of fatigue are common complaints in the general population, yet in the majority of cases, the fatigue is self-limited or has a known cause. Chronic Fatigue Syndrome, also referred to as Myalgic Encephalomyelitis, is a frustrating medical condition characterized by unexplained persistent fatigue that results in significant deficits in one’s daily social, educational, and occupational activities. When those affected first become symptomatic, the main complaint is generally an abrupt onset of impairing fatigue that hinders daily activity.1 Symptoms include sore throat, muscle and joint pain, headaches, and sleep that fails to cause one to feel refreshed. Chronic fatigue syndrome is only diagnosed when other medical conditions that may explain the presence of the fatigue are ruled out.1 Frustratingly, the cause of Chronic Fatigue Syndrome is still poorly understood and widely speculated. It has proven to be very difficult to identify a single cause, and much of the current scientific thought suggests that Chronic Fatigue Syndrome is multifactorial, with both environmental and genetic components playing a role in manifestation of the disease symptoms.2 One of the major obstacles in elucidating the causes of Chronic Fatigue Syndrome is the difficulty of finding a large, homogeneous group of patients who fit the current definition of the disease. One can imagine that for a patient suffering from such debilitating symptoms, with a poorly understood cause, it can be a very trying and difficult experience. In the world of twentyfirst century medicine and science, it is often expected that we have the answers to why someone would suffer with a disease such as this. When a patient is told that the answer is unknown, it can be extremely disheartening and frustrating. Thus, it is critical that medical providers, as well as the general population, become aware of the challenges associated with Chronic Fatigue Syndrome so that compassionate care can be provided with a firm knowledge of the reality those afflicted endure on a daily basis. As more become aware of what Chronic Fatigue Syndrome 1 entails, as well as informed of the promising research currently being conducted, the future of those suffering with the disease can be improved substantially. It is only with increased dissemination of the current knowledge regarding Chronic Fatigue Syndrome that we can hope to make progress towards greater understanding and potential treatments. In this review, the current ideas surrounding the etiology and pathogenesis of Chronic Fatigue Syndrome are discussed. Infectious Agents and Chronic Fatigue Syndrome Speculation over the true cause of the disease has existed since the early 1980s. In many cases of chronic fatigue, patients have become symptomatic after combating a specific infectious disease. Thus, infectious agents have been suggested in many instances, yet there remains no single pathogen that can be identified in a significant proportion of cases. In 1985, two large studies of patients with significant chronic fatigue and other symptoms were reported to have elevated antibody titers against Epstein-Barr virus (EBV) in comparison to healthy controls3,4, and thus it was suggested that chronic fatigue syndrome was actually caused by chronic mononucleosis infection. This idea failed to persist as further studies did not confirm the role of EBV in cases of chronic fatigue syndrome.5-7 Over the years, Chronic Fatigue Syndrome has been linked to a wide variety of other diseasecausing agents such as enteroviruses, cytomegalovirus, Candida albicans, Borrelia burgdorferi, and human herpesvirus.2 Evidence implicating these agents in the disease etiology has not been substantiated in subsequent studies. In a study of 22 monozygotic twin pairs, there was no difference in plasma levels of antibodies to human herpesvirus (HHV)-6, HHV-8, cytomegalovirus, and EBV between the group of twins with Chronic Fatigue Syndrome and the healthy twins.8 Enterovirus VP1, RNA and non-cytopathic viruses have been found in stomach biopsy specimens of Chronic Fatigue Syndrome patients, suggesting that a significant subset of patients may have a chronic enteroviral infection.9 Giardia enteritis appears to have caused an outbreak of Chronic Fatigue Syndrome in 5% of those infected in a large community.10 It has also been estimated that postinfectious fatigue occurs at a rate of 12% following infection with EBV, Q fever, or Ross River virus11, and that postinfectious fatigue has symptoms that are clinically indistinguishable from idiopathic cases of fatigue.12 Because of such common manifestations of fatigue symptoms following numerous infectious diseases, it has been suggested that Chronic Fatigue Syndrome is a product of a variety of types of infections rather than a disease with a single specific etiology. Recently in the research of infectious agents as cause of Chronic Fatigue Syndrome were the 2009 studies suggesting that most cases were associated with a newly described gamma retrovirus, xenotropic murine leukemia virus-related virus (XMRV).13 A study detected the virus in 67% of patients suffering, compared with only 3.7% in healthy controls. There was much excitement surrounding this supposed breakthrough in the frustrating disease, but soon after publication concerns arose. Further studies could not find any evidence of XMRV infection in the same samples tested in the 2009 study, and it was suggested that the XMRV virus arose as the consequence of recombination between two mouse proviruses years following the first documented description of Chronic Fatigue Syndrome. 14,15 As much excitement surrounded XMRV and its role in the disease etiology, the heated debate stressed the importance of full scientific validation in the search for understanding of Chronic Fatigue Syndrome.16 2 Genetics and Chronic Fatigue Syndrome Possible genetic predisposition to Chronic Fatigue Syndrome has been investigated. Using the CDC guidelines for diagnosis of Chronic Fatigue Syndrome, a study demonstrated a concordance of 38% in monozygotic twins versus 11% in dizygotic twins.17 Several genes have been implicated in those affected with Chronic Fatigue Syndrome in recent studies. 18,19 NMR metabolic profiling of a group of patients with Chronic Fatigue Syndrome has demonstrated a significant reduction of glutamine and ornithine in the blood of those affected, suggesting a possible disturbance in amino acid and nitrogen metabolism in disease etiology.20 Cifuentes and Barreto identified a reliable profile of single nucleotide polymorphisms associated with Chronic Fatigue Syndrome, suggesting markers for genetic predisposition to the disease.21 Such findings suggest a genetic component to Chronic Fatigue Syndrome, further highlighting the disease as a multifactorial syndrome. Large-scale genomic studies will prove invaluable to further research in the genetics of Chronic Fatigue Syndrome in the near future. Immunology, Neurophysiology, and Chronic Fatigue Syndrome The associations that have been made between Chronic Fatigue Syndrome and infectious agents have caused attention to shift towards an immunological basis for the condition. Decreased cytotoxic activity has been shown in patients in many studies.22-24 It has been demonstrated that those with Chronic Fatigue Syndrome may have deficient natural killer cell activation and effector capacity.25-27 This suggests an underlying immunodeficiency in those affected that would thus cause a more severe inflammatory response to infectious agents. Such an inflammatory response may result in presentation with Chronic Fatigue Syndrome. Furthermore, Zhang et al. demonstrated that the expression of TGF-B1 in peripheral blood mononuclear cells is significantly elevated in patients with Chronic Fatigue Syndrome.28 Notably, several immune-related microRNAs have been implicated as potential biomarkers for Chronic Fatigue Syndrome, as they play a role in regulating natural killer cells and CD8+T cell related lytic proteins, receptors, and cytotoxic activity.29 Changes in the microRNAs of these cells may disrupt proper functioning in immune response, thus leading to disease symptoms. Because Chronic Fatigue Syndrome generally involves neuropsychological symptoms and alterations in hormone levels regulated by the hypothalamus, many feel that the central nervous system is the main site involved in the pathophysiology of the disease. Regions of decreased cerebral blood flow were observed in patients with Chronic Fatigue Syndrome30, however these findings were not confirmed in subsequent studies.31 Dysfunction of the hypothalamic-pituitaryadrenal axis has also been implicated, with reported studies of exaggerated adrenal responsiveness to corticotropin infusions and lower urinary free cortisol levels in those affected.32 It is evident that both immunologic and neurologic factors may be involved in the pathogenesis of Chronic Fatigue Syndrome. Some argue that Chronic Fatigue Syndrome etiology lies in the immunophysiology of the central nervous system, resulting from inflammatory events in the brain.33 Natelson et al. demonstrated that IL-8 and IL-10 were significantly elevated in the cerebrospinal fluid collected from patients with Chronic Fatigue Syndrome.34 A variety of immunological and neurological abnormalities have been reported in patients with Chronic 3 Fatigue Syndrome, including mitochondrial dysfunctions, abnormalities in proinflammatory cytokines, brain pathology, and autonomic disturbances. Morris and Maes35 propose that initial infection and immune activation caused by a variety of infectious agents leads to a state of chronic peripheral immune activation guided by activated oxidative and nitrosative stress pathways. Such a response produces mitochondrial damage, and subsequent ATP deficits together with inflammation are suggested to cause the symptoms of Chronic Fatigue Syndrome.35 A variety of neuroimmune models for the disease have been proposed very recently, and such studies are encouraging as the etiology of this complex disease becomes elucidated. Conclusion While this review does not provide a single, concrete cause for the pathogenesis of Chronic Fatigue Syndrome, it is evident that a tremendous amount of new and promising research is currently taking place in the field. The cause(s) of the disease are most likely multiple and complex, involving delicate interactions among a variety of systems within the body and the environment. With such enthusiasm for understanding the etiology of this debilitating disease, it is unquestionable that further investigations will lead us closer to firm knowledge of the pathogenesis and treatment options for those affected by Chronic Fatigue Syndrome. In the meantime, it remains paramount that physicians, as well as the general public, be made aware of the signs, symptoms, and implications of Chronic Fatigue Syndrome in order to best aid those affected in a compassionate and knowledgeable manner. References 1. Bennett RM. Goldman: Goldman's Cecil Medicine. 24 ed. Philadelphia, PA: Elsevier; 2012. 2. Mandell GL. Principles and Practice of Infectious Disease. Philadelphia, PA: Elsveir; 2010. 3. Straus SE, Tosato G, Armstrong G, et al. Persisting illness and fatigue in adults with evidence of Epstein-Barr virus infection. Annals of internal medicine 1985;102:7-16. 4. Jones JF, Ray CG, Minnich LL, Hicks MJ, Kibler R, Lucas DO. Evidence for active Epstein-Barr virus infection in patients with persistent, unexplained illnesses: elevated anti-early antigen antibodies. Annals of internal medicine 1985;102:1-7. 5. Mawle AC, Nisenbaum R, Dobbins JG, et al. Seroepidemiology of chronic fatigue syndrome: a case-control study. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 1995;21:1386-9. 6. Buchwald D, Ashley RL, Pearlman T, Kith P, Komaroff AL. Viral serologies in patients with chronic fatigue and chronic fatigue syndrome. Journal of medical virology 1996;50:25-30. 7. Swanink CM, van der Meer JW, Vercoulen JH, Bleijenberg G, Fennis JF, Galama JM. Epstein-Barr virus (EBV) and the chronic fatigue syndrome: normal virus load in blood and normal immunologic reactivity in the EBV regression assay. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 1995;20:1390-2. 8. Koelle DM, Barcy S, Huang ML, et al. Markers of viral infection in monozygotic twins discordant for chronic fatigue syndrome. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2002;35:518-25. 9. Chia JK, Chia AY. Chronic fatigue syndrome is associated with chronic enterovirus infection of the stomach. Journal of clinical pathology 2008;61:43-8. 4 10. Naess H, Nyland M, Hausken T, Follestad I, Nyland HI. Chronic fatigue syndrome after Giardia enteritis: clinical characteristics, disability and long-term sickness absence. BMC gastroenterology 2012;12:13. 11. Hickie I, Davenport T, Wakefield D, et al. Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. BMJ 2006;333:575. 12. Buchwald D, Umali J, Pearlman T, Kith P, Ashley R, Wener M. Postinfectious chronic fatigue: a distinct syndrome? Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 1996;23:385-7. 13. Lombardi VC, Ruscetti FW, Das Gupta J, et al. Detection of an infectious retrovirus, XMRV, in blood cells of patients with chronic fatigue syndrome. Science 2009;326:585-9. 14. Knox K, Carrigan D, Simmons G, et al. No evidence of murine-like gammaretroviruses in CFS patients previously identified as XMRV-infected. Science 2011;333:94-7. 15. Paprotka T, Delviks-Frankenberry KA, Cingoz O, et al. Recombinant origin of the retrovirus XMRV. Science 2011;333:97-101. 16. Etzioni A. Chronic fatigue syndrome: still a long way to go. The Israel Medical Association journal : IMAJ 2011;13:761. 17. Buchwald D, Herrell R, Ashton S, et al. A twin study of chronic fatigue. Psychosomatic medicine 2001;63:936-43. 18. Kerr JR. Gene profiling of patients with chronic fatigue syndrome/myalgic encephalomyelitis. Current rheumatology reports 2008;10:482-91. 19. Kerr JR, Petty R, Burke B, et al. Gene expression subtypes in patients with chronic fatigue syndrome/myalgic encephalomyelitis. The Journal of infectious diseases 2008;197:117184. 20. Armstrong CW, McGregor NR, Sheedy JR, Buttfield I, Butt HL, Gooley PR. NMR metabolic profiling of serum identifies amino acid disturbances in chronic fatigue syndrome. Clinica chimica acta; international journal of clinical chemistry 2012;413:1525-31. 21. Cifuentes RA, Barreto E. Supervised selection of single nucleotide polymorphisms in chronic fatigue sindrome. Biomedica : revista del Instituto Nacional de Salud 2011;31:613-21. 22. Klimas NG, Salvato FR, Morgan R, Fletcher MA. Immunologic abnormalities in chronic fatigue syndrome. Journal of clinical microbiology 1990;28:1403-10. 23. Brenu EW, Staines DR, Baskurt OK, et al. Immune and hemorheological changes in chronic fatigue syndrome. Journal of translational medicine 2010;8:1. 24. Maher KJ, Klimas NG, Fletcher MA. Chronic fatigue syndrome is associated with diminished intracellular perforin. Clinical and experimental immunology 2005;142:505-11. 25. Bassi N, Amital D, Amital H, Doria A, Shoenfeld Y. Chronic fatigue syndrome: characteristics and possible causes for its pathogenesis. The Israel Medical Association journal : IMAJ 2008;10:79-82. 26. Lorusso L, Mikhaylova SV, Capelli E, Ferrari D, Ngonga GK, Ricevuti G. Immunological aspects of chronic fatigue syndrome. Autoimmunity reviews 2009;8:287-91. 27. Aspler AL, Bolshin C, Vernon SD, Broderick G. Evidence of inflammatory immune signaling in chronic fatigue syndrome: A pilot study of gene expression in peripheral blood. Behavioral and brain functions : BBF 2008;4:44. 28. Zhang HY, Liu ZD, Hu CJ, Wang DX, Zhang YB, Li YZ. Up-regulation of TGF-beta1 mRNA expression in peripheral blood mononuclear cells of patients with chronic fatigue syndrome. Journal of the Formosan Medical Association = Taiwan yi zhi 2011;110:701-4. 5 29. Brenu EW, Ashton KJ, van Driel M, et al. Cytotoxic lymphocyte microRNAs as prospective biomarkers for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Journal of affective disorders 2012. 30. Schwartz RB, Komaroff AL, Garada BM, et al. SPECT imaging of the brain: comparison of findings in patients with chronic fatigue syndrome, AIDS dementia complex, and major unipolar depression. AJR American journal of roentgenology 1994;162:943-51. 31. Lewis DH, Mayberg HS, Fischer ME, et al. Monozygotic twins discordant for chronic fatigue syndrome: regional cerebral blood flow SPECT. Radiology 2001;219:766-73. 32. Demitrack MA. Neuroendocrine correlates of chronic fatigue syndrome: a brief review. Journal of psychiatric research 1997;31:69-82. 33. Arnett SV, Alleva LM, Korossy-Horwood R, Clark IA. Chronic fatigue syndrome--a neuroimmunological model. Medical hypotheses 2011;77:77-83. 34. Natelson BH, Weaver SA, Tseng CL, Ottenweller JE. Spinal fluid abnormalities in patients with chronic fatigue syndrome. Clinical and diagnostic laboratory immunology 2005;12:52-5. 35. Morris G, Maes M. A neuro-immune model of Myalgic Encephalomyelitis/Chronic fatigue syndrome. Metabolic brain disease 2012. 6