7 Briefing Paper extracts
advertisement

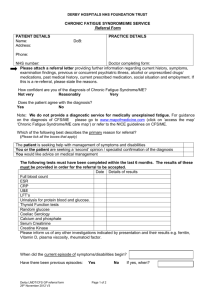
What is happening to ME? the distinguishing features of myalgic encephalomyelitis and their relationship to current diagnostic practice _______________ The clinical profile of ME is unique and does not mimic any other illness “The clinical symptoms were consistent in over sixty recorded epidemics of ME spread all over the world’. ME was known to run a chronic course and patients had disabilities due to persistent symptoms of pain, fatigue and loss of endurance to normal physical activities with conspicuous deterioration of symptoms after exercise (post-exertional malaise)” 1 The following description of the clinical profile of ME is presented with acknowledgement to: CFS Research Foundation: A response to a human tragedy, Rickmansworth, Herts; Ramsey, M (1988): Myalgic Encephalomyelitis and Postviral Fatigue States, The saga of Royal Free disease, London, Gower Medical Publishing/The ME Association, p30; Ramsey, M. (1991): Clinical Identity of the Myalgic Encephalomyelitis Syndrome, Stanford-le-Hope, The ME Association; and Shepherd, C & Chaudhuri, A (2001): ME/CFS/PVFS: an exploration of the key clinical issues, England, Thornton & Pearson/The ME Association, p5. Post-exertional malaise is a key defining feature. Patients experience a considerable exacerbation of symptoms which may precipitate a significant relapse, even after minor amounts of physical exertion. Mental activity can also exacerbate symptoms Cardinal symptoms are: 1 Abnormal muscle fatiguability: “Muscle fatiguability whereby, after even a minor degree of physical effort, three, four or five days, or longer, elapse before full muscle power is restored is unique.” 2 Muscle pain (myalgia) that may include tenderness. Scottish Executive Health Department (2003): Report of the Short Life Working Group on CFS/ME, Edinburgh, The Scottish Executive, p7, referring to: [1] Ramsey, M (1988): Myalgic Encephalomyelitis and Postviral Fatigue States, The saga of Royal Free disease, London, Gower Medical Publishing/The ME Association, p30; and [2] Parish JG. Early outbreaks of "epidemic neuromyasthenia". Postgraduate Medical Journal 1978, 54: pp711-717. [Document 7] A special feature of this disease is that the condition waxes and wanes. Cognitive / neurological dysfunction affecting, for example: memory, concentration, balance, vision, hearing, sleep rhythm, temperature, appetite, hormone production. Symptoms tend to vary and fluctuate in severity from hour to hour and day to day. The illness often follows a pattern of flare-ups interspersed with periods of relative remission. However, some patients experience no remission at all. The illness tends to persist over the long-term. Although the pattern of symptoms and their severity varies from person to person, these cardinal features are common to all. ME can be diagnosed clinically on the basis of these distinguishing features, which are reflected in recently published guidelines by Carruthers et al., 2003.3 Unfortunately, most doctors are unaware of the unique and distinctive presentation of this illness, and the breadth of relevant biomedical research. Misconceptions are widely held, in particular: ME is not synonymous with tiredness “……CFIDS* is not about being tired. Researchers have demonstrated numerous abnormalities of the immune, muscular, cardiovascular, and central nervous systems in people with CFIDS. It is truly a multi-system disease with a strong component of immune dysfunction.”4 *Chronic Fatigue and Immune Dysfunction Syndrome (the term used in the US) “ME is not T.A.T.T. – ‘tired all the time’. ” 5 As with many chronic illnesses, fatigue may be present in ME patients. However, the fatigue is post-exertional, often delayed, disproportionate to effort and quite unlike the ‘fatigue’ experienced by healthy people. 2 Ramsey, M (1988): Myalgic Encephalomyelitis and Postviral Fatigue States, The saga of Royal Free disease, London, Gower Medical Publishing/The ME Association, p30. 3 Carruthers, B et al. (2003): Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols in the Journal of Chronic Fatigue Syndrome, Vol. 11 [1] 2003, pp7-115. 4 US congressional statement by DeFreitas, E 1991; quoted in Shannon, M. M (2000): An International Perspective on ME, presented at the All Party Parliamentary Group on ME AGM, 22 March. 5 The National ME Centre (2003): What is ME and What It’s Not, Harold Wood Hospital, Romford, Essex [Document 7] 2 ME and ‘Chronic Fatigue Syndrome’ – is there a difference in terms of diagnosis? The term ME is rarely used now in medical circles, and most doctors are unaware of the unique and distinctive presentation of this illness. Instead, people presenting with the clinical features of ME are given a diagnostic label of ‘Chronic Fatigue Syndrome’ (CFS). “In 1988, the term ‘Chronic Fatigue Syndrome’ was introduced as a diagnostic term to define all chronic fatiguing disorders that are otherwise unexplained by known medical conditions”6 Rather than providing a viable alternative name for the distinct clinical condition previously known as ME, CFS almost certainly encompasses several different conditions. Although some researchers and clinicians use a strict definition of CFS,7 this term is interpreted in different ways. Some interpretations are broad and inappropriate to ME. Chronic fatigue is a symptom common to many illnesses, and inadequate to describe what ME patients experience. As one patient, giving evidence to the Chief Medical Officer’s Working Group, observed: “Alzheimer’s Disease is not known as ‘Chronic Forgetfulness Syndrome’!” 8 This unfortunate situation has produced an unhelpful change in the medical perception of patients with ME, with resulting in considerable confusion in research and clinical practice. In particular, CFS is perceived by authorities in the UK – including, for example, the Medical Research Council - as synonymous with chronic fatigue which has no medical basis. This use of the expression CFS fails to acknowledge a critical distinction: Unexplained fatigue is listed as a mental and behavioural disorder in the World Health Organisation International Classification of Diseases [ICD] 10, at section F48.0. ME, however, is classified as neurological, at section G93.3: no illness or condition may appear in more than one category. The impact of this on patients has been significant as the implications for health care and management are quite different in respect of these two conditions. For the individual patient, the illness is very real and his or her suffering is exacerbated by the current diagnostic mess. 6 Scottish Executive Health Department (2003): Report of the Short Life Working Group on CFS/ME, Edinburgh, The Scottish Executive, p7. 7 Notably, see Carruthers B et al. (2003): Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols in the Journal of Chronic Fatigue Syndrome, Vol. 11 [1] 2003, pp7-115. This definition equates well to ME. 8 Department of Health (2002): Report of the CFS/ME Working Group: Report to the Chief Medical Officer of an Independent Working Group, London, The Stationery Office p15. [Document 7] 3