11) ICU and Telemetry
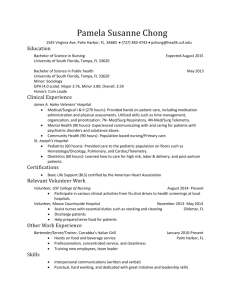
advertisement
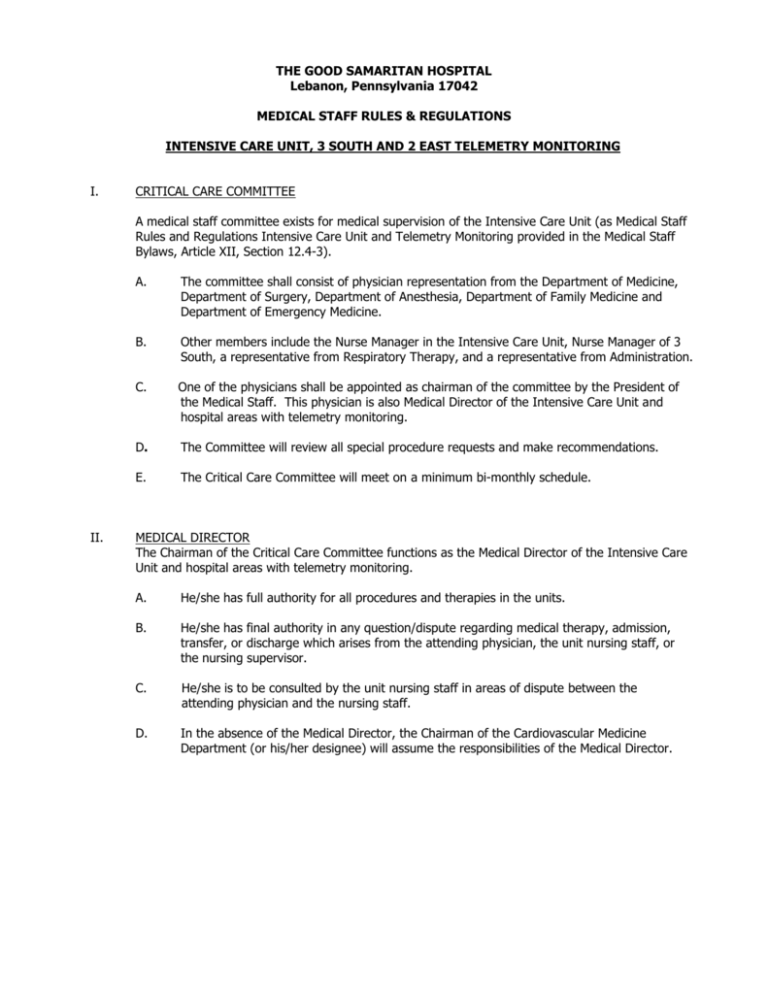
THE GOOD SAMARITAN HOSPITAL Lebanon, Pennsylvania 17042 MEDICAL STAFF RULES & REGULATIONS INTENSIVE CARE UNIT, 3 SOUTH AND 2 EAST TELEMETRY MONITORING I. CRITICAL CARE COMMITTEE A medical staff committee exists for medical supervision of the Intensive Care Unit (as Medical Staff Rules and Regulations Intensive Care Unit and Telemetry Monitoring provided in the Medical Staff Bylaws, Article XII, Section 12.4-3). II. A. The committee shall consist of physician representation from the Department of Medicine, Department of Surgery, Department of Anesthesia, Department of Family Medicine and Department of Emergency Medicine. B. Other members include the Nurse Manager in the Intensive Care Unit, Nurse Manager of 3 South, a representative from Respiratory Therapy, and a representative from Administration. C. One of the physicians shall be appointed as chairman of the committee by the President of the Medical Staff. This physician is also Medical Director of the Intensive Care Unit and hospital areas with telemetry monitoring. D. The Committee will review all special procedure requests and make recommendations. E. The Critical Care Committee will meet on a minimum bi-monthly schedule. MEDICAL DIRECTOR The Chairman of the Critical Care Committee functions as the Medical Director of the Intensive Care Unit and hospital areas with telemetry monitoring. A. He/she has full authority for all procedures and therapies in the units. B. He/she has final authority in any question/dispute regarding medical therapy, admission, transfer, or discharge which arises from the attending physician, the unit nursing staff, or the nursing supervisor. C. He/she is to be consulted by the unit nursing staff in areas of dispute between the attending physician and the nursing staff. D. In the absence of the Medical Director, the Chairman of the Cardiovascular Medicine Department (or his/her designee) will assume the responsibilities of the Medical Director. MEDICAL STAFF RULES AND REGULATIONS ICU, 3 SOUTH AND 2 EAST/TELEMETRY MONITORING PAGE 2 III. ADMITTING PRIVILEGES A. ADMITTING PRIVILEGES FOR THE INTENSIVE CARE UNIT: 1. Admission to the Intensive Care Unit must have prior complete medical evaluation by the attending physician or the consultant, or attending physician must examine the patient within six (6) hours following unit admission. 2. Sufficient information must always be available to the charge nurse in order that appropriate life saving care may be instituted. In the absence of this, the charge nurse has the right and obligation to immediately consult the Chairman of the Critical Care Committee or a physician member of the committee for professional advice. 3. All patients admitted to the Intensive Care Unit are expected to be seen by the physician in charge of their care at least once daily, or as often as dictated by the condition of the patient. Appropriate progress notes are expected to routinely reflect the patient's current status. This enables all members of the health care team to keep abreast of the patient's progress regime. 4. A nursing supervisor and/or charge nurse has the responsibility to recommend to an attending physician that an unstable patient be transferred to the Intensive Care Unit, providing the patient meets the eligibility for unit admission. Should the attending physician be unavailable, the nursing supervisor will contact the Intensive Care Medical Director for evaluation and advice. Should a discord occur between the attending physician and the nursing supervisor, the Medical Director of Intensive Care Unit will be contacted for patient evaluation and possible transfer to the Unit. 5. Failure to adequately follow patients consistent with the policies of the Intensive Care Unit will require immediate review by the Critical Care Committee Chairman to determine the need for continued critical care of the patient. The attending physician will be notified of this action. 6. Any physician may admit to the Unit within the following guidelines. a. The first consult on these patients should be completed within 12 hours after admission to the unit unless the attending physician falls into categories d, e, f, or g. b. The consult may be waived by the consulting physician after review of the case and discussion with the attending physician in special instances where appropriate. c. When areas of special expertise are required in the handling of critically ill patients, or in special circumstances, it is suggested that the care of the patient be transferred to the care of the consulting physician with that area of expertise. MEDICAL STAFF RULES AND REGULATIONS ICU, 3 SOUTH AND 2 EAST TELEMETRY MONITORING PAGE 3 7. B. d. Department of Medicine, Category II and III may admit to the ICU without consultation, but should obtain a consult when other special areas of expertise are required. e. Department of Surgery, Category III may admit to the ICU without consultation, but should obtain a consult when other special areas of expertise are required. f. Department of Pediatrics, Category II may admit to the ICU without consultation, but should obtain a consult when other special areas of expertise are required. g. Department of Ob/Gyn, Category I, II and III may admit to the ICU without consultation, but should obtain a consult when other special areas of expertise are required. h. All other physician categories may admit with consult of a physician with admitting status to the Intensive Care Unit. i. Approval for special procedures should be outlined according to category and approved by the Medical Staff when applicable. j. It is recommended that custodial care patients not be admitted to the Unit. k. All patients transferred to the unit shall have medical orders written. l. All patients in the Unit shall have orders reviewed on transfer from the Unit and if appropriate, changed or rewritten. Nurses will maintain a "triage list". When disputes arise, the Chairman of the Critical Care Committee or in his/her absence, his/her replacement will resolve the dispute. PRIVILEGES FOR ADMITTING A PATIENT FOR TELEMETRY MONITORING: It is the policy of the hospital areas with telemetry monitoring that priority for telemetry monitoring be given to only those patients who meet criteria for cardiac monitoring. 1. Patients are accepted into areas with telemetry monitoring based on bed availability and the patient's clinical requirements. 2. Transfers are acceptable to telemetry monitoring areas from ICU or in select cases from other patient care areas. MEDICAL STAFF RULES AND REGULATIONS ICU, 3 SOUTH AND 2 EAST TELEMETRY MONITORING PAGE 4 C. 3. Any physician may place a patient on telemetry monitoring within the following guidelines. a. The first consult on these patients should be completed within 12 hours after admission to the unit unless the attending physician falls into categories b, c, d, or e. b. Department of Medicine, Category II and III may place a patient on a cardiac monitor without consultation, but should obtain a consult when other special areas of expertise are required. c. Department of Surgery, Category III may place a patient on a cardiac monitor without consultation, but should obtain a consult when other special areas of expertise are required. d. Department of Pediatrics, Category II may place a patient on a cardiac monitor without consultation, but should obtain a consult when other special areas of expertise are required. e. Department of Family Medicine, Category II, if currently privileged to do so, may place a patient on a cardiac monitor without consultation, but should obtain a consult when other special areas of expertise are required. f. Department of Ob/Gyn, Category I, II and III may place a patient on a cardiac monitor without consultation, but should obtain a consult when other special areas of expertise are required. 4. The consult may be waived by the consulting physician after review of the case and discussion with the attending physician in special instances where appropriate. 5. All admissions of a patient to be placed on a cardiac monitor must have prior medical evaluation by the attending or consulting physician before admission, or be seen by their attending physician within four hours of admission. Sufficient information must be available to the charge nurse in order that appropriate care is provided. 6. Bed assignment is made by the registered nurses in the monitored bed areas. 7. Arrangements for admission will be made by the attending physician who will contact the Admitting Office and the monitored bed areas. 8. Nurses will maintain a triage list. When disputes arise, the Chairman of the Critical Care Committee, or in his/her absence, his/her replacement will resolve the dispute. 9. When the nursing staff are uncomfortable with an admission in which a patient is placed on a cardiac monitor, the case will be reviewed by the Chairperson of the Critical Care Committee, or his/her absence, the designated replacement. Those physicians who do not have telemetry monitoring privileges without consultation may, upon submission of appropriate credentials to the Critical Care Committee and appropriate credentialing through that individual department, request telemetry monitoring privileges without consultation. MEDICAL STAFF RULES AND REGULATIONS ICU, 3 SOUTH AND 2 EAST TELEMETRY MONITORING PAGE 5 IV. GUIDELINES FOR ADMISSION - ADMISSION CRITERIA TO THE INTENSIVE CARE UNIT The initial decision to admit a patient is the responsibility of the attending physician. The following shall serve as guidelines for eligible admission: A. Any patient with a known or suspected acute myocardial infarction regardless of complications. B. Any patient with known coronary artery disease presenting with new symptoms or an instability of chronic symptoms. C. Any patient presenting with a compromising dysrhythmia. D. Any patient presenting with chest pain of unknown etiology. E. Any hemodynamically unstable patient thought to have compromised cardiac function from unknown etiology. F. Any Code Blue patient. G. Hemodynamically unstable medical patients from causes other than cardiovascular in origin. H. Acute trauma patients including severe and/or multiple fractures. I. Unstable patients due to acute respiratory problems such as: 1. Status asthmaticus 2. Fresh tracheostomies 3. Acute respiratory failure J. All patients who need mechanical ventilation in any phase. K. Unstable patients due to acute neurological events such as: 1. Uncontrolled seizures 2. Unconscious state with unknown etiology 3. Cerebral vascular accident 4. Trauma L. Patients with hemodynamic compromise due to the following gastrointestinal reasons: 1. Gastrointestinal bleeding of any nature 2. Extensive G.I. or abdominal surgery M. Patients with burns N. Patients whose surgery is of a magnitude or nature which makes their present condition unstable or raises the possibility of instability. O. Patients whose past health state or intra-operative performance requires close monitoring. MEDICAL STAFF RULES AND REGULATIONS ICU, 3 SOUTH AND 2 EAST TELEMETRY MONITORING PAGE 6 P. Patients with infections of a severe nature including septic shock. Q. Contagious infections may be admitted with proper precautions, if necessary, to the appropriate rooms within the ICU. R. All patients with major thoracic surgery and major chest trauma. S. All patients requiring hemodynamic monitoring. T. Any patients with excessive drug ingestion, which compromises heart rate or rhythm, and/or level of consciousness, and/or ventilatory status. U. Patient whose medical condition or medical apparatus is out of the ordinary so that the floor nursing staff is not familiar with providing adequate care. No patient in the above categories will be excluded from admission to the Intensive Care Unit, if room is available unless his/her condition is a threat to the operation of the unit. In this instance, the need for admission to the Intensive Care Unit will be discussed with the Medical Director of the Intensive Care Unit. The final decision for admission to the Intensive Care Unit, or for telemetry monitoring in other hospital areas, is with the attending physician. V. GUIDELINES FOR ADMISSION OR TRANSFER OF PATIENTS FOR 3 SOUTH TELEMETRY MONITORING The following are guidelines are for appropriate admissions for telemetry monitoring: A. Class I - Telemetry monitoring for 72 hours (or less if cancelled by physician): 1. Patients with any hemodynamically stable dysrhythmia started on new cardiac medications; 2. The hemodynamically stable R/O MI, with the following guidelines: a. Initial EKG has no acute changes, and, b. Patient is pain free, or pain is controllable, and hemodynamically stable, and, c. No evidence of acute life-threatening arrhythmia, and, d. History is one with high to moderate probability of myocardial infarction 3. Patients requiring management of medications such as inotropic medications, Antidysrhythmics, and/or beta-blockers or calcium channel blockers (e.g. diltiazem, dobutamine, dopamine, procainamide, amiodarone, or nitroglycerine) a. A patient requiring titration of dopamine/dobutamine for blood pressure support will only be maintained in the Intensive Care Unit or CV Unit. MEDICAL STAFF RULES AND REGULATIONS ICU, 3 SOUTH AND 2 EAST TELEMETRY MONITORING PAGE 7 4. Note: B. The NPO post-operative patient being maintained on IV anti-arrhythmias until able to take oral anti-arrhythmic medications. If the attending physician feels that the patient requires telemetry monitoring beyond the above time period, the attending physician must document the reason for telemetry monitoring extension in the patient’s chart and reorder telemetry monitoring for no more than an additional 24 hours. Class II - Telemetry monitoring for 48 hours (or less if cancelled by physician): 1. 2. 3. All acute myocardial infarction patients from ICU or CVU who have been pain free, and exhibiting the following stable hemodynamic parameters: a. Stable vital signs, and, b. Electrically stable cardiac rhythm for 24 hours, and, c. Stable cardiac output measured by adequate tissue and vital organ perfusion. A patient admitted with compromised cardiac function such as stabilized angina, CHF, cardiomyopathy who is hemodynamically stable but who still requires cardiac monitoring. The patient requiring prophylactic IV or PO anti-arrhythmia drug therapy while changing or instituting oral drug agents. Note: If the attending physician feels that the patient requires telemetry monitoring beyond the above time period, the attending physician must document the reason for telemetry monitoring extension in the patient’s chart and reorder telemetry monitoring for no more than an additional 24 hours. MEDICAL STAFF RULES AND REGULATIONS ICU, 3 SOUTH AND 2 EAST TELEMETRY MONITORING PAGE 8 C. Class III – Telemetry monitoring for 24 hours (or less if cancelled by physician): 1. The hemodynamically stable R/O MI, with the following guidelines: a. Initial EKG has no acute changes, and, b. Patient is pain free and hemodynamically stable, and c. No evidence of acute life-threatening arrhythmia, and, d. History is one with low probability of myocardial infarction 2. The patient admitted for syncope to R/O arrhythmias 3. Stable post-cardiac catheterization patients 4. The hemodynamically stable patient pre- and post- insertion of a permanent pacemaker 5. Any medical or surgical patient who is hemodynamically stable but requires cardiac monitoring Note: If the attending physician feels that the patient requires telemetry monitoring beyond the above time period, the attending physician must document the reason for telemetry monitoring extension in the patient’s chart and reorder telemetry monitoring for no more than an additional 24 hours. VI. GUIDELINES FOR ADMISSION - ADMISSION CRITERIA TO 2 EAST A. Remote Telemetry monitoring for 24 hours (telemetry must be reordered or discontinued Every 24 hours. B. Reason for Remote Telemetry: 1. Ambulatory dysfunction/hemodynamically stable 2. Hemodynamically stable with known dysrhythmia 3. Syncope that is hemodynamically stable, asymptomatic and with no neurological deficits. 4. R/O CVA/TIA for patient who is hemodynamically stable asymptomatic and no neurological deficits 5. Postoperative patient who is hemodynamically stable but may require fluid and or transfusions due to fluid shifts. 6. A patient with a pacemaker who is stable, asymptomatic and is hemodynamically stable that is admitted for a procedure and required telemetry post-procedure 7. Hemodynamically stable patient who requires intravenous administration of a beta blocker and has previously been taking an oral form of the drug. 8. Patient who is admitted for elective placement of a permanent pacemaker or battery change and is hemodynamically stable. MEDICAL STAFF RULES AND REGULATIONS ICU, 3 SOUTH AND 2 EAST TELEMETRY MONITORING PAGE 9 VII. TRANSFER CRITERIA A. FROM INTENSIVE CARE UNIT AT THE GOOD SAMARITAN HOSPITAL 1. The initial decision to discharge a patient from the Intensive Care Unit at The Good Samaritan Hospital is the responsibility of the attending physician, in conjunction with the consulting physician. 2. The following serve as guidelines: a. All patients being transferred out of the Intensive Care Unit shall have their orders reviewed. If there is a problem with a decision to discharge a patient, the responsibility rests with the Chairman of the Critical Care Committee or the designee. b. B. A triage list will be maintained in both Intensive Care Units on a daily basis. This will list those patients that may be transferred should an emergency bed be required. FROM TELEMETRY MONITORING UNIT It is not necessary that all orders be rewritten when telemetry monitoring is discontinued. VIII. RULES AND REGULATIONS PERTAINING TO OPERATION OF UNIT A. The Intensive Care Unit at The Good Samaritan Hospital policies and procedures governing: 1. Admission criteria to the unit 2. Admission to the unit 3. Transfer criteria from the unit 4. Discharge criteria from the unit 5. Definitions of nursing roles 6. Routine critical care orders 7. Code Blue and drug protocol during Code Blues are detailed in the Intensive Care Unit Policy and Procedure Manual or in the Nursing Policy and Procedure Manuals. B. Policies and procedures governing hospital areas with telemetry monitoring capabilities include: 1. 2. 3. C. Admission to the unit Patient Assignment Emergency Protocols are detailed in the specific nursing unit Policy and Procedure Manual or in the Nursing Policy and Procedure Manual. All new treatment modalities must be presented to and approved by the Critical Care Committee and other Medical Staff Committees as appropriate before implementation in the Intensive Care Unit setting. SIGNATURE SHEET These Rules and Regulations for the Intensive Care Unit, 3 South and 2 East Telemetry Monitoring have been reviewed and revised by the Critical Care Committee and approved. _______________ Date ______________________________ Wilson Morris, D.O., Chairman Critical Care Committee _______________ Date ______________________________ Earl H. Brinser, D.O. President, Medical Staff