Dr Margaret Mysor, Dr Jonathan Booth, Dr Jon
advertisement

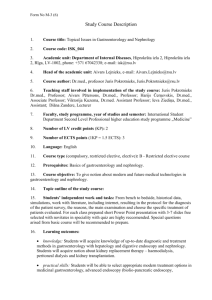
HEALTH EDUCATION THAMES VALLEY - SPECIALTY TRAINING PROGRAMME IN GASTROENTEROLOGY About Health Education Thames Valley We are the Local Education and Training Board (LETB) for Thames Valley covering Berkshire, Buckinghamshire and Oxfordshire. Our vision is to ensure the delivery of effective workforce planning and excellent education and training to develop a highly capable, flexible and motivated workforce that delivers improvements in health for the population of Thames Valley. Thames Valley LETB is responsible for the training of around 2000 Foundation and Specialty trainees. Health Education Thames Valley is a relatively small organisation with a defined geographical area which serves as a single unit of application. In the majority of cases successful candidates will be asked to preference their choice of location for either one or two years. Some programmes will require successful candidates to indicate a location and specialty. Future placements will usually be based on individual training and educational needs. Please note that applications are to the Health Education Thames Valley as a whole. This may mean that you may be allocated to any geographic location within the deanery depending on training needs. The Gastroenterology Training Programme The gastroenterology training programme is a 5 year programme, starting at with competitive entry at ST3 level. During this time, the trainee's work will be monitored for satisfactory progress and subject to annual reviews in the form of ARCPs. Progression on the programme will be dependent upon these reviews. The posts on this rotation have been approved for Specialist Training by the JRCPTB. The posts attract National Training Numbers and provide training towards a Certificate of Completion of Training (CCT). The Postgraduate Dean has confirmed that this post has the necessary educational and staffing approvals. The programme is based in several different Trusts throughout Health Education Thames Valley so trainees may find themselves employed by any of the following Trusts and placed in any of the following hospitals: Trust Oxford University Hospitals NHS Trust Hospitals and Locations John Radcliffe Hospital, Oxford http://www.ouh.nhs.uk/ The Horton Hospital, Banbury http://www.ouh.nhs.uk/ Royal Berkshire NHS Foundation Trust Royal Berkshire Hospital, Reading http://www.royalberkshire.nhs.uk/ Buckinghamshire Healthcare NHS Trust Wycombe Hospital, High Wycombe & Stoke Mandeville Hospital, Aylesbury http://www.buckshealthcare.nhs.uk/ Milton Keynes Hospital NHS Foundation Trust Milton Keynes General Hospital http://www.mkgeneral.nhs.uk/ Rotation Information Rotations may at times change in response to clinical need from the Trusts. Expected rotation arrangements for this programme are: There are 12 posts within the Health Education Thames Valley programme in Gastroenterology/General Internal Medicine. 2 posts - Gastroenterology and G(I)M Supervisors: 3 posts - Gastroenterology and G(I)M Supervisors: 3 posts - Gastroenterology and Hepatology Supervisors: Milton Keynes Hosp. Dr S Lanzon-Miller Dr G MacFaul Royal Berks Hosp Reading Dr M Myszor Dr A DeSilva Dr J C L Booth Dr J Simmons Dr C Green (P/T) Dr Alex Evans John Radcliffe, Oxford Dr A Bailey Dr J Collier Dr SPL Travis Dr S Keshav Dr B Braden Dr AA Bailey Dr J East 2 posts - Gastroenterology and G(I)M Supervisors: 2 posts Hospital - Gastroenterology and G(I)M Supervisors: Horton Hospital, Banbury Dr A Ellis Dr J Marshall Dr B Braden (1 day) Dr A Bailey (1 day) Wycombe/Stoke Mandeville Dr D Gorard Dr E Johns Dr S Cullen (P/T) Dr R Sekhar The rotation is built up on an individual basis taking into account the trainee’s interests, training requirements and prior experience. These requirements will be balanced by the availability of local posts and the needs of others in the Training Programme. A rotation will usually consist of a year 1 placement in either Banbury or Milton Keynes. Subsequently trainees may move to either Reading or High Wycombe. A year of training in Oxford tends to occur in years 3 or 4. Over a 5 year period most trainees will spend 12 months at each of the training centres. Year 6 placements may be at any centre in the region. Most trainees undertake a formative period of research culminating in the award of an MD or DPhil. Where appropriate, trainees have undertaken an MSc. See: http://www.expmedndm.ox.ac.uk/home and http://www.expmedndm.ox.ac.uk/gastroenterology-unit for clinical and basic science research projects undertaken by trainees. The output from the training programme is good and recent appointments as consultants have been to centres including Southampton, Gloucester, Exeter, St Marks, and Manchester. The full outline scheme is shown on the enclosed rotations. Research is actively encouraged during the tenure of the post. Trainees are encouraged to undertake clinical research whilst working in the 5 centres and to undertake a formal period of research either in Oxford or other major centre of research. Within the rotations and centres to which a Trainee will be attached, all sub-specialty parts of the curriculum are covered. These include: specialist management of inflammatory bowel disease, intestinal failure and nutrition, experience in specialised hepatobiliary and pancreatic disorders, general hepatology, interventional endoscopic techniques, capsule endoscopy, endoscopic ultrasound, oesophageal pH testing, oesophageal and anorectal manometry, liaison psychiatry, and paediatric gastroenterology. Oxford is also one of two centres in the UK for intestinal transplantation. The only aspect of gastroenterology not formally covered in a local centre is liver transplantation. Trainees wishing to obtain such experience will normally undertake a 2 year training programme in Hepatology within their 5 yr rotation, 1 year of which would be in Oxford with a 3 month secondment at a major transplant centre. These posts are competitive and decided by separate interview and are advertised on a national basis. Trust Information – WYCOMBE / STOKE MANDEVILLE HOSPITAL Dr David Gorard (Training Lead), Dr Sue Cullen, Dr Emily Johns, Dr R Sekhar Buckinghamshire Healthcare NHS Trust encompasses Wycombe Hospital, Amersham Hospital and Stoke Mandeville Hospital. It serves residents in Buckinghamshire, Thame (Oxfordshire), Tring (Hertfordshire) and Leighton Buzzard (Bedfordshire) with a combined population of 550,000. Following the reconfiguration of acute services, Wycombe Hospital performs predominantly elective work, while acute emergency services are mainly provided at Stoke Mandeville Hospital. The 2 registrars in gastroenterology are each based at the more elective Wycombe Hospital site for 4 months, and based at the more acute Stoke Mandeville Hospital site for 8 months. Gastroenterology at Wycombe Currently most elective Gastroenterology training is organised at Wycombe Hospital: although from 2014 some elective outpatient sessions take place at the Stoke Mandeville site in Aylesbury on a rotational basis. The department of Gastroenterology at Wycombe consists of three Consultants; Dr Sue Cullen, Dr David Gorard, Dr Emily Johns. They are supported by an Associate Specialist (Dr Christine Helmer). During the 4 months at Wycombe Hospital, the gastroenterology trainee will attend 3 outpatient clinics each week, and 3 or 4 endoscopy lists each week. There is a dedicated viral hepatitis clinic which runs weekly, in addition to general gastroenterology clinics and endoscopy lists. Gastroenterology at Stoke Mandeville Hospital During the 8 months at Stoke Mandeville Hospital, the gastroenterology registrars have a pivotal role in managing a team of junior doctors and are involved in the day-to-day care of acute gastroenterology, hepatology and general medicine inpatients. The consultants (Dr Cullen, Dr Gorard, Dr Johns, Dr Sekhar) are also rostered as duty gastroenterologist at Stoke Mandeville Hospital for a week at a time. On a daily basis, patients with acute gastroenterology/hepatology problems are triaged to the gastroenterology inpatient team. Dr Cullen leads a Nutrition Team and undertakes a once weekly nutrition ward round at Stoke Mandeville Hospital. Depending on the registrar’s experience, he/she will attend at least one endoscopy session at Stoke Mandeville Hospital each week and gain experience in endoscoping upper GI bleed patients. Although based at Stoke Mandeville Hospital, during the 8 month period, the registrar will spend Wednesdays at Wycombe Hospital (+/- Amersham hospital) to attend one clinic and one endoscopy session. Endoscopy Training The Endoscopy Suite at Wycombe Hospital has two procedure rooms equipped with Fuji endoscopes. The Endoscopy Suite at Stoke Mandeville Hospital has two procedure rooms equipped with Olympus endoscopes. Most of the lists are run by the Gastroenterology Department with a handful run by Consultant Surgeons. Training opportunities vary widely from the ability to teach basis diagnostic endoscopy and flexible sigmoidoscopy, through to colonoscopy for those in their third year. For those in more senior years advanced colonic polypectomy techniques, PEG insertions and oesophageal stenting are available. A wide range of haemostatic techniques including injection, banding, clipping and heater probe therapy are available. Depending on a trainee’s experience, appropriate lists are allocated and adjusted to allow for optimal training and experience. There is one ERCP list at Wycombe and one at Stoke Mandeville Hospital each week – although these are available for training those who wish, such training is supplemental to more formal training elsewhere. Teaching and Training Specialist Registrars in Gastroenterology are released on Thursday afternoons each week to attend central training in Oxford. Trainees are also released to attend general medical training one day a month. Within the hospital there is a weekly grand round. The gastroenterology journal club runs approximately fortnightly at Wycombe Hospital. There is a weekly upper GI cancer MDT meeting and a weekly lower GI cancer MDT meeting, involving review of X-rays and histology. There is a once monthly joint gastroenterology and surgical clinic meeting where X-rays and histology are discussed. At Stoke Mandeville there is a weekly Wednesday morning general medical teaching session and there are opportunities for the Registrar to teach junior doctors and medical students on secondment from Oxford. Research Wycombe has been a productive department in terms of gastroenterology research and audit. Time is allowed for Registrars to develop and supervise projects and most Registrars have successfully completed papers or abstract submissions whilst being at the hospital. Examples of timetables 4 months at Wycombe Hospital: Mon Tues Wed Thurs Fri 8.15 Upper GI MDT DG clinic (AH) DG clinic SC clinic (AH) or Endoscopy Endoscopy Lunchtime: Journal Club & GI meeting/ lower GI MDT Endoscopy admin Endoscopy or EJ clinic On calls at WH as per WH stroke/cardiology rota Oxford Endoscopy 8 months at Stoke Mandeville Hospital: Mon Ward Work Ward Work Tues Wed Ward Work or endoscopy SC clinic (AH) or Endoscopy Ward Work WH: Endoscopy or EJ clinic Thurs 8.15 Upper & lower GI MDT Fri Ward work Ward work Oxford Ward work or Endoscopy On calls at SMH, as per SMH acute medical registrar rota. General Internal Medicine at Stoke Mandeville and Wycombe Hospitals Acute services at Wycombe Hospital consist of dedicated Cardiology Services (fully functional angiography Unit) and Acute Stroke services. There are no gastroenterology or general medical inpatient services at Wycombe Hospital. The gastroenterology registrar when based at Wycombe will participate in an out-of-hours on call rota for cardiac/stroke patients at Wycombe as part of GIM training. Acute medicine is centred at Stoke Mandeville Hospital which receives unselected medical take, apart from cardiac and stroke patients who are admitted to Wycombe Hospital. The gastroenterology registrars will participate in an on call rota for unselected medical patients at Stoke Mandeville as part of GIM training. Experience will include: Acute general medicine. including CCU experience and ward follow up clinic. Gastroenterology a) Management of gastroenterology inpatients b) Gastroenterology outpatients to include general gastroenterology, inflammatory bowel disease and hepatology clinics. c) Experience of emergency gastroenterology (in particular upper gastrointestinal bleeding) and including emergency endoscopy under consultant supervision. d) Therapeutic upper gastrointestinal endoscopy including variceal injections/ variceal banding, oesophageal dilatations, insertion of oesophageal stents, insertion of feeding gastrostomy tubes. e) Colonoscopy including training in colonoscopic polypectomy. f) ERCP training where appropriate g) Experience in parenteral nutrition ROYAL BERKSHIRE HOSPITAL Dr Margaret Mysor, Dr Jonathan Booth, Dr Jon Simmons (Training Lead), Dr Des deSilva, Dr Caroline Green, Dr Nish Chandra, Dr Alex Evans The Royal Berkshire NHS Foundation Trust (650 beds) is the District General Hospital serving West Berkshire, an area extending from Hungerford in the west to Henley-on-Thames in the east, and including Wokingham and parts of Hampshire to the south and parts of Oxfordshire to the north. The resident population served by the Trust is around 550,000. The hospital provides all those services normally associated with a very large District General Hospital. Only cardio-thoracic surgery, complex hepato-biliary and transplant surgery, neurological surgery, plastic and major neonatal surgery are referred outside the district to specialist centres in Oxford or London. Gastroenterology , Endoscopy and General Internal Medicine There are five speciality based medical firms within the Trust. Each team has a home base ward, and looks after any patients admitted to their ward. Where possible, patients are triaged to the ward most relevant to their specialty problem. All acute medical patients are currently admitted via the Acute Medical Unit (AMU), which is based near the X-ray and A+E Departments. Within the AMU there is a Higher Monitoring Area (Medical HDU) of four beds providing care of the critically ill including non-invasive ventilation, CVP monitoring and step down from ITU. The HMU is supported by the ITU outreach team. The gastroenterology ward consultant and registrar provide daily input into AMU to see new admissions with gastroenterological problems The Gastroenterology unit is currently based on 28-bedded Sidmouth Ward and in the Endoscopy and Outpatients’ Departments. Outpatient clinics and endoscopy lists are also carried out at West Berkshire community hospital in Newbury. Approximately 2000 new patients and 3500 follow-up patients are seen annually in the Department’s outpatient clinics. In addition to general gastroenterology, we have specialist inflammatory bowel disease, intestinal failure and viral hepatitis clinics. Endoscopy: The trust runs a modern purpose built 4 room endoscopy unit with xray facilities in one of the rooms. The unit perform in excess of 6000 procedures a year and offers the full range of endoscopic modalities including diagnostic and therapeutic upper and lower GI endoscopy, push enteroscopy, endoscopic ultrasound and ERCP. The unit is managed by gastroenterology but work is shared with the surgical specialities with pooling of lists. The unit has JAG accreditation and is a screening centre for the National Bowel Cancer Screening programme. In addition to hospital based medical staff the unit is staffed by 2 GP assistants and 2 nurse endoscopists. There is also a GI physiology lab, managed by the surgical directorate, providing pH monitoring and manometry for oesophageal diseases. Reduced points training lists are provided and active participation with JETS is strongly encouraged. The trust provides a regional service for wireless capsule endoscopy. A specialist PEG nurse provides a comprehensive enteral feeding access service to the hospital and community. There is a multidisciplinary hospital nutrition team providing support for enteral and parenterally fed patients. Meetings within the Gastroenterology Department: The Department holds fortnightly X ray and pathology meetings, and a fortnightly seminar / journal club for which the junior members of the gastroenterology medical team prepare papers in rotation. There is a well-attended weekly medical grand round meeting. Links with Surgery: We continue to enjoy a close working relationship with both the upper GI and colorectal surgeons, with joint management of difficult hepatobiliary and inflammatory bowel disease patients and those with acute GI bleeding. The department contributes to weekly upper and lower GI cancer MDT meetings and a monthly pancreatico-biliary MDT with Oxford. Existing Gastroenterology Staff Establishment: 7 Consultant Gastroenterologist / Physicians 3 Specialist Registrars in gastroenterology (Oxford Regional Rotation) 1 Associate Specialist 1 F2 4 Clinical Nurse Specialists (PEG/wireless endoscopy, IBD, hepatitis, bowel screening) 1ST1 2 FY1 Examples of weekly timetables when not on call for General medicine Ward week Monday Tuesday Wednesday Thursday Friday Consultant WR X-Ray meeting Consultant WR Nutrition WR Consultant WR Ward work Clinic or Endoscopy Endoscopy Grand Round Oxford Teaching Wednesday Thursday Gastro Meeting UGI MDT Non-ward week Monday Tuesday Friday IBD clinic Gastro clinic Endoscopy LGI MDT endoscopy Nutrition WR IBD clinic Grand Round Oxford Teaching Hepatitis clinic Training will include 1. Acute General Medicine To include rotad weeks running the Acute Medical Unit with supervision of the junior team and Consultant post take ward rounds, general medical inpatient care and ward rounds,. 2. Gastroenterology a) Management of gastroenterology inpatients b) Gastroenterology outpatients to include general gastroenterology, inflammatory bowel disease and hepatology clinics. c) Experience of emergency gastroenterology (in particular upper gastrointestinal bleeding) and including emergency endoscopy under consultant supervision. d) Therapeutic upper gastrointestinal endoscopy to include variceal banding, oesophageal dilatations, insertion of oesophageal stents, insertion of feeding gastrostomy tubes. e) Colonoscopy - training under supervision including polypectomy. f) ERCP as appropriate g) Experience in parenteral nutrition MILTON KEYNES Drs. Lanzon-Miller, Madhotra and MacFaul (TPD and training Lead) MKFT is a district general hospital and a foundation trust, serving a catchment area of 270,000 population. There are 3 gastroenterologists: Dr Sandro Lanzon-Miller, Dr Ravi Madhotra, and Dr George MacFaul. Dr Sandro Lanzon-Miller is a senior general gastroenterologist. He did his GI training at London and area of research was on acid-peptic disease. He has special interest in inflammatory bowel disease. He is the Lead clinician for Upper GI cancer for the trust. Dr Ravi Madhotra is the Lead clinician for gastroenterology and endoscopy. He is Director of Bowel Cancer Screening programme for Buckinghamshire. Dr George MacFaul is a gastroenterologist trained in the Oxford deanery. He has special interest in nutrition, hepatology and general gastroenterology, is a keen endoscopist and an accredited bowel cancer screener and colonoscopy trainer, currently leading Endoscopy training. He also leads the Nutrition team in the hospital. He is the Gastroenterology Training programme Director for the Oxford Deanery. The Gastroenterology firm consists of 2 SpRs (Oxford rotation), 2 Staff Grade doctors, 2 FY2/ST1 and 2 FY1 doctors, Clinical There are a variety of training opportunities in gastroenterology and general internal medicine, available for specialist registrars at Milton Keynes. Each ST/SpR has 2 or more endoscopy training sessions available for supervised training. For senior trainees ERCP training is available. The trainees have access to therapeutic endoscopy including oesophageal stent insertion, variceal banding and PEG/PEJ insertion. A brand new state-of-the-art 4-room endoscopy unit opened in April 2009 (Olympus scopes) with Scopeguide in 2 rooms. MKHFT is a designated Screening centre for Buckinghamshire bowel cancer screening programme. An induction pack is available for all trainees when they join the department, with a Nurse lead for training who co-ordinates the training lists as per the needs of the trainee. There is arrangement for regular feedback between trainees and trainers, and a monthly endoscopy users group meeting which the trainee is encouraged to attend. There are 2 supervised clinics per week in general gastroenterology and IBD, mixed for new and follow up patients. The trainees are required to attend colorectal, UGI, hepatobiliary and IBD MDTs on Thursday between 12-1.30pm, before attending Gastro SpR teaching at Oxford. The trainees get good experience in general medicine while on-call for unselected admissions, with predominantly gastro in-patients on the dedicated gastrointestinal ward. There are plentiful opportunities to gain experience in seeing inpatient referrals under supervision. There is a multi-disciplinary nutrition meeting weekly, led by Dr MacFaul and the Nutrition ANP. There is a weekly general medicine grand round on Wednesdays and Journal club on Fridays. 1. General medicine at MKHFT Acute general medicine to include inpatient ward rounds, acute general medical take, post take ward rounds, some general medical follow-up and including CCU Unit experience. There is a busy MAU with 5 acute physicians and an excellent Ambulatory Care Unit. 2. Gastroenterology Management of gastroenterology in-patients including 2 general medical/gastroenterology ward rounds per week. b) Gastroenterology outpatients: 2 gastroenterology outpatient clinics will be held weekly. a) c) Endoscopy - Upper Gastrointestinal Endoscopy under supervision, it will also include therapeutic procedures like Sclerotherapy, variceal banding, oesophageal stent insertion and PEG d) Rigid and Flexible Sigmoidoscopy e) Colonoscopy and polypectomy training f) Training in therapeutic ERCP for senior GI trainees g) Experience in delivering a nutrition service. MILTON KEYNES HOSPITAL Post 1 (Dr Lanzon-Miller) Monday Tuesday Wednesday Thursday Friday Consultant WR Ward round OPD (IBD) Consultant Ward Round Registrar Ward Round Postgraduate Teaching CME/audit Endoscopy Training MDT Colorectal/UGI Meeting Endoscopy Training Oxford Study Half Day OPD Gastro Wednesday Thursday Friday SpR WR CME OPD Gastro Post 2 (Dr MacFaul) Monday Tuesday SpR WR Consultant round ward Postgraduate Teaching Endoscopy Training Gastro OPD Endoscopy Training MDT Colorectal/UGI/ IBD Meeting Oxford Study Half Day Horton Hospital - Oxford University Hospitals NHS Trust Dr Antony Ellis (Training Lead), Dr Jonathan Marshall. Ward work The Horton hospital is situated in Banbury and serves a population of approximately 160,000. Since 1998 it has been part of the John Radcliffe Hospitals NHS Trust. The hospital currently provides services in acute medicine, acute surgery, trauma and orthopaedics, obstetrics, gynaecology, and paediatrics. There are many visiting consultants from Oxford who deliver sub-specialty services including rheumatology, neurology, ophthalmology, ENT to name a few. The Department of Medicine has 106 beds in a dedicated medical block with in addition a 10 bedded medical assessment unit. The average number of admissions is 20 with takes of up to 40 on occasion. There are 8 medical consultants who cover the acute medical take on a 1:8 rota. They are supported by 6 SpRs and 2 trust grade registrars. There is additional on-call support utilising research fellows from Oxford. The F1 programme involves doctors rotating within the JRII trust. The ST1 and ST2 grades are all in training programmes. The Department of Gastroenterology consists of 2 Consultant Gastroenterologists, Dr Antony Ellis and Dr Jonathan Marshall based in Banbury. There are 2 further Consultant Gastroenterologists, Dr Barbara Braden and Dr Adam Bailey who are based in Oxford and work in Banbury for 1 day each. The Consultants are supported by 2 SpRs in gastroenterology, 2 ST1/ST2’s and 1F1. Both Dr Ellis and Dr Marshall have undertaken the ‘Train the Trainers’ course and have an interest in postgraduate medical education. The endoscopy suite has recently been modernised and consists of 2 rooms equipped with Olympus Lucera stacks. For upper GI endoscopy we have lucera scopes with a twin channel therapeutic gastroscope for emergency upper GI bleeding. We have NBI capability for Barrett's surveillance. Haemostatic techniques taught include adrenaline injection, heater probe, variceal banding, cyanoacrylate injection, clipping and argon plasma coagulation (APC). We have the Olympus scope guide system which is used to facilitate colonoscopy training. The department is accredited for the bowel cancer screening programme (BCSP) ERCP services are now delivered in Oxford and Dr Ellis undertakes a list on this site. Trainees identified as appropriate for ERCP training may utilise this list. Dr Marshall undertakes a weekly dedicated colonoscopy training list in Oxford which is open to all StR’s within the Trust At present there are 6 out-patient clinics for training purposes which are supervised by consultants. These do not take place if a consultant is absent. To facilitate the rapid evaluation of patients these clinics remain coded as general gastroenterology but contain a mix of luminal and solid organ pathology. General medicine accounts for less than 5% of all follow ups seen in clinic. There are 31 in-patient beds run by Gastroenterology of which between 12 and 15 are filled by ‘specialty patients’. In addition to the above there is a weekly journal club, X-Ray meeting, and 1 hour case presentation session. SpRs are encouraged to attend the upper GI and HPB MDTs with Dr Ellis on a Monday morning. There is weekly teaching in Oxford which is timetabled to allow for regular attendance. This includes a lecture, pathology – including Banbury histology, and interesting cases. The StR’s are released on a monthly basis to attend the general medicine teaching. The unique affiliation with the JRII allows for a seamless transition for patients requiring tertiary intervention with rapid repatriation to their local community when investigation/treatment is complete. StR’s are able to monitor progress of patients both with visits to the wards in Oxford on training days and remotely via the integrated computer system. Feedback from previous StR’s has been positive with particular reference to endoscopy training and personal support. During this post experience will be gained in 1. General Medicine a) Acute general medicine to include general medical take and post take ward round. b) Management of acute general medicine inpatients. c) General Medical Outpatients to include general medical referrals and ward follow up clinic. d) Coronary care / HDU experience. 2. Gastroenterology a) Management of gastroenterology in-patients including 2 general gastroenterology ward rounds per week. b) Gastroenterology outpatients. One clinic in general gastroenterology / IBD and one general gastroenterology / hepatology. c) Training in upper gastrointestinal endoscopy under supervision 2 sessions per week under consultant direction. d) Focused training in colonoscopy e) Rigid and flexible sigmoidoscopy. f) Work with Dr Marshall for nutrition round and participate in PEG service g) ERCP. Senior SpR’s can arrange training with Dr Ellis Examples of timetables at HGH Monday Tuesday Wednesday Thursday Friday Ward Round (Dr A Ellis) UGI / pancreatico biliary MDT Endoscopy Research / audit Clinic Gastroenterology / IBD (Dr A Ellis) Endoscopy (Dr Braden) Medical cases Grand round Oxford Ward round Journal Club OPD Ward Ward round Gastroenterology / Hepatology Monday round reg (Dr A Ellis) Tuesday Study Half Day Wednesday (Dr A Ellis) Thursday Friday Reg round / Admin Admin Ward Round (Dr J Marshall) Teaching Medical cases Endoscopy (Dr J Marshall / Dr J Harrison) Oxford training half day Grand Round Clinic (Dr J Marshall) X-Ray Meeting Endoscopy (Dr J Marshall Admin Journal Club Clinic (Dr J Marshall) Ward Round (Dr Marshall) John Radcliffe Hospital – Oxford University Hospitals NHS Trust The John Radcliffe Hospital serves a local population of 620,000, with an allied clinical gastroenterology service at the Horton Hospital, Banbury (Dr Tony Ellis, Dr Jonathan Marshall), which is an independent component of the regional rotation. The Unit sees 2000 inpatients, 3250 new patient referrals, 14500 follow-ups and 12500 endoscopic procedures/year, of which 15% are tertiary referrals with inflammatory bowel disease, liver disease or intestinal failure. Organisation The Service is consultant led. There are two 'sides': a Luminal side (Dr Travis and Dr Keshav) and Hepatobiliary side (Dr Collier and Dr Cobbold), with combined outpatient clinics and shared Consultant care on each side. A 200 page Gut Doctors’ Guide (2012) is available on line to every trainee, explaining local protocols and practice. Consultants John Radcliffe Dr Jane Collier MD FRCP Dr Ollie Brain Dr Satish Keshav DPhil FRCP Dr Simon Travis DPhil FRCP Dr Barbara Braden MD PhD Dr Adam Bailey FRACP Dr James East MD MRCP Dr Jeremy Cobbold Dr Beth Bird - Lieberman Honorary Consultants Dr E Barnes DPhil FRCP Special Interest Hepatology Endoscopy/IBD IBD IBD, intestinal failure Endoscopy/EUS Upper GI Endoscopy Hepatology Endoscopy /upper GI Hepatic viral immunology Dr A Simmons PhD FRCP Mucosal T-cell immunology Trainees rotate through posts and clinics There are 3 rotation StR’s and 1 Hepatology* StR (3 months Cambridge and 9 month oxford post- nationally appointed). Each week there are 3 general gastroenterology and specialist clinics in liver disease, hepatitis C, inflammatory bowel disease and coeliac disease, as well as regular nutrition, adolescent IBD, HIV and haemophilia clinics. There are also 12 joint liver transplant clinics/year.There is a 19 bed specialist gastroenterology ward and 6 bed day unit (for ERCP, paracentesis, anti-TNF therapy, venesection). There are 5 endoscopy rooms. There are over 40 endoscopy lists/week, including all diagnostic and interventional procedures, EUS (2) and ERCP (3). Great emphasis is placed on multidisciplinary care, with close cooperation between colorectal and upper gastrointestinal surgeons, gastrointestinal Specialist Senior Clinical histopathology and radiology. There is a Registrars Fellows specialist IBD multidisciplinary team meeting Luminal 4 posts, each with 6 each week. Intestinal transplantation started endoscopy and 4 Hepatology* in Oxford in 2009. The hepatobiliary radiology academic Hepatobiliary sessions/week meeting is attended by the hepatobiliary Nutrition surgeons acting as a benign MDT. Allied professions Other trainees F1 (1) ST 1 (1) ST 2 (1) ACF (1) CNS; hepatology (2.5), IBD (2), nutrition (3) Dietitians (4) Research (2) GI Pharmacy (1) Teaching and Training Education of junior medical staff is carried out through two gastroenterology teaching sessions each week, together with Consultant-lead regional Specialist Registrar teaching each week. There is a weekly joint postgraduate teaching session held between physicians and surgeons, a journal club, separate luminal and hepatobiliary histopathology and X-ray sessions each week. The Gastroenterology Unit undertakes training of first and third year clinical Oxford medical students, as well as medical students from overseas. These activities specifically include tutorials, teaching ward rounds and seminar sessions as well as less formal ward and outpatient based teaching. Research The Oxford Gastroenterology Unit is acknowledged as one of the premier units for gastroenterological research in Europe and attracts research fellows from all over the world. It is lead by Fiona Powrie, Sidney Truelove Professor of Gastroenterology, a mucosal immunologist. She has established the Translational Gastroenterology Unit, situated in the John Radcliffe Hospital, with laboratories adjacent to the clinical service offices and the Gastroenterology ward. The Unit builds on excellent clinical programmes in inflammatory bowel disease and hepatology as well as cutting edge basic science programmes in mucosal immunology. The new state of the art laboratories bring together scientists, clinician scientists and gastroenterologists with the objective of translating fundamental research in mucosal immunology into enhanced treatments for inflammatory bowel disease, liver disease and cancer. Oxford has an international reputation in the aetiopathogenesis and therapeutics of inflammatory bowel disease, viral hepatitis and primary sclerosing cholangitis. There is a 3 bed Clinical Trials’ Facility within the new Endoscopy Unit. The gastroenterology Specialist Registrars rotate in 3-4 month blocks round subspecialty areas (luminal, hepatology, hepatobiliary, nutrition). The general medical commitment is limited to night cover in rotation with all the specialist registrars (32) at the John Radcliffe. a) Management of Gastroenterology inpatients including 2 gastroenterology ward rounds per week. The specialist GI ward has 21 beds for secondary and tertiary referrals needing inpatient treatment. b) Gastroenterology outpatients. A general weekly gastroenterology clinic and weekly hepatology or inflammatory bowel disease clinic. c) Advanced endoscopy/colonoscopy/ERCP training. The opportunity to learn endoscopic ultrasound techniques. d) Opportunity to learn upper and lower GI motility techniques, including oesophageal manometry, oesophageal pH testing and rectal manometry. e) Nutrition training, including management of complex intestinal failure and intestinal transplantation Examples of timetable (i) Hepatology Monday Tuesday Hepatitis Clinic Gastro Clinic Wednesday MDT HPB cancer Endoscopy (training list) Thursday Friday Endoscopy List Journal Club OPD Hepatology Student and SHO teaching Grand Round Consultant Liver Ward Round Radiology Meeting ERCP (training list) Oxford Study Half Day Ward work Liver Histology (ii) Luminal Monday Tuesday Wednesday Thursday Friday Journal Club Emergency Endoscopy list Colonoscopy/ Endoscopy Ward Round (Dr Travis or Dr Keshav) GI X Ray Meeting OPD General Gastro (Dr Travis/ Dr Keshav) Intestinal failure ward round (Dr Travis) Student and SHO teaching IBD MDT meeting Oxford Study Half Day IBD Clinic (Dr Travis/ Dr Keshav) Teaching and Research There is a fixed half-day teaching session in Oxford each week. Teaching includes formal lectures, histology review sessions, clinical cases and talks from guest speakers. The lectures are designed to cover the curriculum over a 3 year cycle. All trainers within the rotation are committed to training StR’s in Gastroenterology. Teaching is arranged both locally at the base hospitals and centrally in Oxford on a weekly basis. General Medicine is taught locally with monthly formal teaching arranged by the deanery Research is encouraged at every level, with almost three quarters of all trainees doing a PhD or MD. The Translational Gastroenterology Unit in Oxford is co-located with the clinical service, integrating basic science and clinical practice. Each year trainees will be expected to develop a project in conjunction with their Education Supervisors. It is expected that this work will lead to presentation to a learned Society at Regional, National or International level and to publication. All trainees would be expected to present a project at least once during the year and those that have not presented to a learned Society will present to the members of the Specialty Training Committee Duties of Post – MAIN DUTIES AND RESPONSIBILITIES These vary slightly and according to the exact part of the rotation the trainee is attached to, but all posts include 6 fixed sessions consisting of 2 out-patients, 2 endoscopy and 2 ward round sessions. All posts in Banbury, High Wycombe, Milton Keynes and Reading include General Medicine and a commitment to acute General Medical Take with experience on CCU and/or ICU. StRs based in Oxford have no inpatient or out-patient general medicine exposure but may participate in the medical on-call rota. Daily Commitment This varies between posts but is outlined in the timetables given with each rotation which is enclosed with this job description. Main Conditions of Service Appointments to this programme are subject to the Terms and Conditions of Service (TCS) for Hospital Medical and Dental Staff (England and Wales). In addition appointments are subject to: Applicants having the right to work and be a doctor or dentist in training in the UK Registration with the General Medical Council Pre-employment checks carried out by the Trust HR department in line with the NHS employment check standards, including CRB checks and occupational health clearance. The employing Trust’s offer of employment is expected to be on the following nationally agreed terms: Hours – The working hours for junior doctors in training are now 48-hours (or 52hours if working on a derogated rota) averaged over 26 weeks (six months). Doctors in training also have an individual right to opt-out if they choose to do so, but they cannot opt-out of rest break or leave requirements. However, the contracts for doctors in training make clear that overall hours must not exceed 56 hours in a week (New Deal Contract requirements) across all their employments and any locum work they do. http://www.nhsemployers.org/your-workforce/need-to-know/european-working-timedirective Pay – you should be paid monthly at the rates set out in the national terms and conditions of service for hospital medical and dental staff and doctors in public health medicine and the community health service (England and Wales), “the TCS”, as amended from time to time. The payscales are reviewed annually. Current rates of pay may be viewed at http://www.nhsemployers.org/your-workforce/pay-and-reward/pay/pay-andconditions-circulars/medical-and-dental-pay-and-conditions-circulars Part time posts will be paid pro-rata Pay supplement –depending upon the working pattern and hours of duty you are contracted to undertake by the employer you should be paid a monthly additional pay supplement at the rates set out in paragraph 22 of the TCS. The current payscales may be viewed at http://www.nhsemployers.org/your-workforce/pay-and-reward/pay/pay-andconditions-circulars/medical-and-dental-pay-and-conditions-circulars The pay supplement is not reckonable for NHS pension purposes. The pay supplement will be determined by the employer and should be made clear in their offer of employment and subject to monitoring. Pension – you will be entitled to join or continue as a member of the NHS Pension Scheme, subject to its terms and rules, which may be amended from time to time. If you leave the programme for out of programme experience you may have a gap in your pension contributions. More information can be found at http://www.nhsbsa.nhs.uk/pensions Annual Leave – your entitlement to annual leave will be five or six weeks per annum depending on your previous service/incremental point, as set out in paragraphs 205206 of the TCS. The TCS may be viewed at http://www.nhsemployers.org/your-workforce/pay-and-reward/nhs-terms-andconditions/junior-doctors-dentists-gp-registrars/junior-doctors-terms-and-conditionsof-service-and-associated-documents Sick pay – entitlements are outlined in paragraph 225 of the TCS. Notice –you will be required to give your employer and entitled to receive from them notice in accordance with paragraphs 195-196 of the TCS. Study Leave –the employer is expected to offer study leave in accordance with paragraphs 250-254 of the TCS. Local policy and procedure will be explained at induction. Travel Expenses – the employer is expected to offer travel expenses in accordance with paragraphs 277-308 of the TCS for journeys incurred in performing your duties. Local policy and procedure should be explained at induction. Subsistence expenses – the employer is expected to offer subsistence expenses in accordance with paragraph 311 of the TCS. Local policy and procedure should be explained at induction. Relocation expenses – the employer will have a local policy for relocation expenses based on paragraphs 314 – 315 of the TCS and national guidance at http://www.nhsemployers.org/PayAndContracts/MedicalandDentalContracts/JuniorD octorsDentistsGPReg/Pages/DoctorsInTrainingJuniorDoctorsTermsAndConditions150908.aspx You are advised to check eligibility and confirm any entitlement with the employer before incurring any expenditure. Pre-employment checks – all NHS employers are required to undertake preemployment checks. The employer will confirm their local arrangements, which are expected to be in line with national guidance at http://www.nhsemployers.org/your-workforce/recruit/employment-checks/nhsemployment-check-standards Professional registration – it will be a requirement of employment that you have professional registration with the GMC/GDC for the duration of your employment. Though the post is covered by NHS Indemnity, you are strongly advised to register with the MPS for professional indemnity. Health and Safety – all employers have a duty to protect their workers from harm. You should be advised by the employer of local policies and procedures intended to protect your health and safety and expected to comply with these. Disciplinary and grievance procedures – the employer will have local policies and procedures for dealing with any disciplinary concerns or grievances you may have. They should advise you how to access these, not later than eight weeks after commencement of employment. Educational Supervisor – the employer or a nominated deputy (usually the Director of Medical Education) will confirm your supervisor on commencement. General information on the LETB’s management of Specialty Training programmes, including issues such as taking time out of programme and dealing with concerns or complaints, is available at www.oxforddeanery.nhs.uk and in the national ‘Gold guide’ to Specialty Training at http://specialtytraining.hee.nhs.uk/. Please ensure that you inform Health Education Thames Valley of any changes to your contact details. January 2015