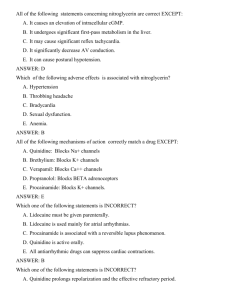
Clinical pharmacology of facilities used at the diseases of
advertisement

Module 1. Clinical pharmacology of facilities used at the diseases of the cardiovascular system and breathening organs Text tests tasks 1. All of the following statements concerning nitroglycerin are correct EXCEPT: A. It causes an elevation of intracellular cGMP. B. It undergoes significant first-pass metabolism in the liver. C. It may cause significant reflex tachycardia. D. *It significantly decrease AV conduction. E. It can cause postural hypotension. 2. Which of the following adverse effects is associated with nitroglycerin? A. Hypertension B. *Throbbing headache C. Bradycardia D. Sexual dysfunction. E. Anemia. 3. All of the following mechanisms of action correctly match a drug EXCEPT: A. Quinidine: Blocks Na+ channels B. Brethylium: Blocks K+ channels C. Verapamil: Blocks Ca++ channels D. Propranolol: Blocks BETA adrenoceptors E. *Procainamide: Blocks K+ channels. 4. Which one of the following statements is INCORRECT? A. Lidocaine must be given parenterally. B. *Lidocaine is used mainly for atrial arrhythmias. C. Procainamide is associated with a reversible lupus phenomenon. D. Quinidine is active orally. E. All antiarrhythmic drugs can suppress cardiac contractions. 5. Which one of the following statements is INCORRECT? A. Quinidine prolongs repolarization and the effective refractory period. B. Mexiletine shortens repolarization and decreases the effective refractory period. C. *Propranolol increases Phase 4 depolarization. D. Verapamil shortens the duration of the action potential. E. Amiodarone prolongs repolarization. 6. Which one of the following statements about antiarrhythmic drugs is CORRECT? A. *They may act by converting unidirectional block to a bidirectional block. B. They often cause an increase in cardiac output. C. As a group they have mild side effects. D. They all affect Na+ channels in the cell membrane. E. They are equally useful in atrial and ventricular arrhythmias. 7. The major drawback to antianginal use of propranolol is: A. *Exacerbation of congestive heart failure B. Increased blood pressure C. urine retention D. diabetes-like hyperglycemia E. blurred vision 8. Ventricular premature depolarizations A. Isosorbide dinitrate B. *Disopyramide C. Propranolol D. Nifedipine E. Nitroglycerin 9. Isosorbide dinitrate: A. Antiarrhythmic action is via alpha-adrenergic blockade B. Ventricular premature depolarizations C. *Angina pectoris prophylaxis D. Conversion of atrial fibrillation to sinus rhythm E. Treatment of ventricular fibrillation 10. When quinidine is administered to a patieny with atrial fibrilation A. the ventricular rate may increase dangerously B. arterial hypotension usually results if the drug is administered intravenously C. thrombi attached to fibrillating atria may embolize D. *all are correct E. none are correct 11. Agents which may lower circulating plasma lipids include: A. Clofibrate B. Nicotinic acid C. Cholestyramine D. Dextrothyroxine E. *All are correct 12. Decreases automaticity of ectopic pacemakers A. Quinidine B. Lidocaine C. *Both: Quinidine, Lidocaine D. Nitroglycerin E. Neither 13. Increases transmembrane action potential duration: A. Lidocaine B. *Quinidine C. Atenolol D. Digoxin E. Esmolol 14. Extensively metabolized by circulating enzymes: A. Quinidine B. Lidocaine C. Nicotinic acid D. Cholestyramine E. *Neither 15. Which one of the following is the most common side effect of antihyperlipidemic drug therapy ? A. Elevated blood pressure B. *Gastrointestinal disturbance C. Neurological problems D. Heart palpitations E. Migraine headaches 16. Which one of the following hyperlipidemias is characterized by elevated plasma levels of chylomicrons and has no drug therapy available to lower the plasma lipoprotein levels? A. *Type I B. Type II C. Type III D. Type IV E. Type V 17. Which one of the following drugs decreases de novo cholesterol synthesis by inhibiting the enzyme 3hydroxy-3-methylglutaryl CoA reductase? A. Clofibrate B. Niacin C. Cholestyramine D. *Lovastatin E. Gemfibrozil 18. Binds bile acids in the intestine, thus preventing their return to the liver via the enterohepatic circulation: A. Niacin B. *Clofibrate C. Cholestyramine D. Probucol E. Lovastatin 19. Cause a decrease in plasma triacylglycerol levels by increasing the activity of lipoprotein lipase: A. Lovastatin B. Clofibrate C. Cholestyramine D. Niacin E. *Probucol 20. Cause a decrease in liver triacylglycerol synthesis by limiting available free fatty acids needed as building blocks for this pathway: A. Cholestyramine B. *Niacin C. Clofibrate D. Probucol E. Lovastatin 21. Inhibits 3-hydroxy-3-methylglutaryl CoA reductase, the rate-limiting step in cholesterol synthesis: A. *Lovastatin B. Niacin C. Cholestyramine D. Clofibrate E. Probucol 22. Which one of the following drugs is useful in treating tachycardia? A. Phenoxybenzamine B. Isoproterenol C. Phentolamine D. *Propranolol E. Prazosin 23. Equilibrium between plasma and tissue levels for quinidine is reached: A. *in 1 or 2 d B. in approximately 1 wk C. in 1–3 wk D. in just a few minutes E. in 2 h 24. Equilibrium between plasma and tissue levels for phenytoin is reached: A. *in approximately 1 wk B. in 1 or 2 d C. in 1–3 wk D. in just a few minutes E. in 2 h 25. Equilibrium between plasma and tissue levels for amiodarone is reached: A. *in 1–3 wk B. in 1 or 2 d C. in approximately 1 wk D. in just a few minutes E. in 2 h 26. Equilibrium between plasma and tissue levels for IV lidocaine is reached: A. *in just a few minutes B. in 1 or 2 d C. in approximately 1 wk D. in 1–3 wk E. in 2 h 27. Drowsiness, paresthesias, muscle twitching, convulsions, changes in mental status (eg, confusion), hypersensitivity reactions (eg, urticaria, edema, anaphylaxis) – adverse effects of: A. *Lidocaine B. Phenytoin C. Propranolol D. Disopyramide E. Verapamil 28. Adverse effects of nitrates are: A. *hypotension, dizziness, tachycardia B. bradycardia, bronchospasm, heart failure C. peripheral edema, headache, heart failure D. nausea and constipation E. lightheadedness, weakness, peripheral edema 29. GI problems—nausea, vomiting, flatulence, constipation or diarrhea, abdominal discomfort are the most common adverse effects of: A. *dyslipidemic drugs B. calcium channel blockers C. beta-adrenergic blocking agents D. nitrates E. all of the above 30. Which of the following adverse effects is associated with nitroglycerin? A. Bronchospasm B. *Throbbing headache C. Bradycardia D. Sexual dysfunction. E. Anemia. 31. Nausea, vomiting, flatulence, constipation or diarrhea, abdominal discomfort are the most common adverse effects of: A. *dyslipidemic drugs B. calcium channel blockers C. beta-adrenergic blocking agents D. nitrates 32. All of the following statements concerning nitroglycerin are correct EXCEPT: A. It causes an elevation of intracellular cGMP. B. It undergoes significant first-pass metabolism in the liver. C. It may cause significant reflex tachycardia. D. *It can not cause throbbing headache. E. It can cause postural hypotension. 33. Which of the following adverse effects is associated with nitroglycerin? A. Hypertension B. *Increasing of intracranial pressure C. Bradycardia D. Sexual dysfunction. E. Anemia. 34. Which one of the following statements is INCORRECT? A. *Atenolol increases Phase 4 depolarization. B. Mexiletine shortens repolarization and decreases the effective refractory period. C. Quinidine prolongs repolarization and the effective refractory period. D. Verapamil shortens the duration of the action potential. E. Amiodarone prolongs repolarization. 35. The major drawback to antianginal use of atenolol is: A. Diabetes-like hyperglycemia B. Increased blood pressure C. Urine retention D. *Exacerbation of congestive heart failure E. Blurred vision 36. Nitroderm is used: A. Antiarrhythmic action is via (-adrenergic blockade B. Ventricular premature depolarizations C. *Angina pectoris prophylaxis D. Conversion of atrial fibrillation to sinus rhythm E. Treatment of ventricular fibrillation 37. When quinidine is administered to a patient with atrial fibrilation A. the ventricular rate may increase dangerously B. arterial hypotension usually results if the drug is administered intravenously C. thrombi attached to fibrillating atria may embolize D. *all are correct E. none are correct 38. Agents which may lower circulating plasma lipids include: A. Atorvastatin B. Nicotinic acid C. Cholestyramine D. Dextrothyroxine E. *All are correct 39. Which one of the following is a specific alpha-adrenergic antagonist: A. Atenolol B. Timolol C. Labetalol D. *Terazosin E. Sotalol 40. Inhibits 3-hydroxy-3-methylglutaryl CoA reductase, the rate-limiting step in cholesterol synthesis: A. *Pravastatin B. Niacin C. Cholestyramine D. Clofibrate E. Probucol 41. Adverse effects of organic nitrates are: A. nausea and constipation B. bradycardia, bronchospasm, heart failure C. peripheral edema, headache, heart failure D. *throbbing headache, dizziness, tachycardia E. lightheadedness, weakness, peripheral edema 42. What diuretic is used for the removal of hypertensive crisis? A. Dichlothiazide B. *Furosemide C. Spironolactonum D. Mannitum E. Triamteren 43. Indicate the antiarrytmic drug from of adrenoblockers group A. Nitroglycerin B. Amiodaron C. *Metoprolol D. Verapamil E. Asparcam 44. The drug related to the group of calcium antagonists A. Apressinum B. Prazosinum C. *Nifedipine D. Reserpine E. Papaverini hydrochloridum 45. Mechanism of action of cardiac glycosides A. Block the activity of COX2 B. Cause the dilatation of coronary vessels C. Block the beta-adrenoreceptors D. Block the calcium channels E. *Block the activity of adenosine-tryphosphatase (ATP-ase) 46. A drug that can selectively supress automaticity in Purkinje fibers compared to the sinus node: A. verapamil B. atenolol C. propranolol D. diltiazem E. *lidocaine 47. A drug, or class of drugs, that has been documented to reduce mortality following a myocardial infarction: A. Class Ia antiarrhythmics B. Class Ic antiarrhythmics C. *Class II antiarrhythmics D. digoxin E. Class III antiarrhythmics 48. GI upset, tinnitus and cinchonism are common side effects of: A. lidocaine B. digoxin C. propranolol D. *quinidine E. amiodarone 49. An antiarrhythmic drug with the most "non-selective" mechanism of action: lidocaine A. Quinidine B. Propranolol C. Sotalol D. *amiodarone 50. A primary mechanism by which Class I antiarrhythmic drugs produce their therapeutic effect in patients with ventricular arrhythmias: A. Block L-type Ca channels B. Block beta-adrenergic receptors C. *Increase the Effective Refractory Period D. Increase vagal tone to the AV node E. Increase the dispersion of refractoriness 51. Primary indications for treatment of cardiac arrhythmias include all of the following EXCEPT: A. *Arrhythmias that reduce cardiac output B. Arrhythmias that are prone to degenerate into more serious arrhythmias C. Arrhythmias that cause vascular stasis D. Arrhythmias that increase the risk of stroke E. Monomorphic premature ventricular beats 52. A side effect of furosemide that can increase the automaticity of ectopic cardiac pacemakers: A. hypercalcemia B. hyperkalemia C. *hypokalemia D. hyponatremia E. hypothyroidism 53. In the treatment of exertional angina: A. *nitroglycerin reduces O2 demand by decreasing preload B. nitroglycerin increases O2 supply by dilating atherosclerotic vessels C. attacks frequently occur during sleep D. nitroglycerin increases cardiac myocyte cAMP levels E. beta blocking agents have no beneficial action 54. Diltiazem: A. *decreases calcium entry through L type channels B. increases total peripheral resistance C. increases cardiac output D. increases heart rate E. increases gastrointestinal motility 55. A drug effect that is produced by therapeutic doses of both propranolol and amiodarone is blockade of: A. cardiac Na channels B. cardiac K channels C. *beta-adrenoceptors D. alpha-adrenoceptors E. L-type Ca channels 56. The most common cellular mechanism responsible for production of cardiac arrhythmias in patients with ischemic heart disease: A. Hypokalemia B. depressed automaticity C. sick sinus syndrome D. *reentrant excitation E. hormonal imbalance 57. In a patient with a high risk for coronary artery disease (LDL cholesterol 200 mg/dL, normal tryglycerides), the best lipid lowering drug would be: A. nicotinic acid B. gemfibrozil C. atorvastatin D. colestipol E. *cholestyramine 58. Indicate the antiarrythmic drug which exerts membrane-stabilizing action. A. Atenolol B. *Quinidine sulfate C. Nitroglycerin D. Digoxin E. Isadrinum 59. Nitrates relieve angina pain by reducing preload, which is: A. *Oxygen demand of the heart B. Pressure within the heart C. Blood volume within the heart D. Pressure against which the heart must pump E. Contractility of the heart muscle 60. Indicate the side effect of nitroglycerine: A. Itching of skin B. Bradicardia C. *Headache D. Rise of arterial pressure E. Intestine atony 61. Indicate the Verapamil possible side effect, as antiarrhythmic drug: A. Tachycardia B. Bronchospasm C. Stenocardia D. Mouth dryness E. *Decrease of artery pressure (hypotension) 62. Nifedipine and verapamil both A. *cause coronary vasodilation B. depress atrioventricular nodal conduction C. cause reflex tachycardia D. stimulate calcium entry into cells 63. Which of the following agents is selective for (beta1-adrenergic receptor? A. Metaproterenol B. Propranolol C. *Metoprolol D. Terbutalin E. Timolol 64. Selective blockade of beta1-adrenergic receptors: A. Labetalol B. Prazosin C. Timolol D. *Atenolol E. Sotalol 65. Is a specific alpha-adrenergic antagonist: A. *Prazosin B. Timolol C. Labetalol D. Atenolol E. Sotalol 66. Labetalol is: A. *a selective alpha-adrenergic antagonistas well as a nonspecific beta-adrenergic antagonist B. is a specific alpha-adrenergic antagonist C. is a nonspecific beta-adrenergic antagonist D. is a selective beta1-adrenergic blocker E. Neither 67. Which of the following agents is (are) pure beta1-adrenergic agonists? A. Albuterol B. Propranolol C. *Metoprolol D. Isoproterenol E. Timolol 68. Weakness or dizziness, especially with activity or exercise – adverse effects of: A. *Propranolol B. Phenytoin C. Lidocaine D. Disopyramide E. Verapamil 69. Adverse effects of beta-adrenergic blocking agents are: A. *bradycardia, bronchospasm, heart failure B. hypotension, dizziness, lightheadedness C. headache, heart failure, pulmonary edema, D. nausea and constipation E. hypotension, dizziness, tachycardia 70. Adverse effects of calcium channel blockers are: A. *dizziness, lightheadedness, peripheral edema, constipation B. bradycardia, bronchospasm, heart failure C. hypotension, tachycardia, headache D. palpitations and headache E. hypotension, dizziness 71. The mechanism by which digoxin causes a positive inotropic effect on heart tissue is by: A. increasing ATP hydrolysis B. stimulating the Na/K pump C. *increasing intracellular Na and Ca D. sensitizing the heart to catecholamines E. inhibiting the Na/H exchanger 72. Calcium channel blockers with prolong action: A. Nifedipine B. Verapamil C. Diltiazem D. *Amlodipine E. Nebivolol 73. All of the following mechanisms of action correctly match a drug EXCEPT: A. Quinidine: Blocks Na+ channels B. Brethylium: Blocks K+ channels C. Verapamil: Blocks Ca++ channels D. Propranolol: Blocks beta adrenoceptors E. *Sotalol: Blocks K+ channels. 74. The major drawback to antianginal use of metoprolol is: A. *Exacerbation of congestive heart failure B. Increased blood presure C. urine retention D. blurred vision E. diabetes-like hyperglycemia 75. Nifedipine and verapamil both: A. cause reflex tachycardia B. depress atrioventricular nodal conduction C. *cause coronary vasodilation D. stimulate calcium entry into cells E. None of the above 76. Which of the following agents is selective for beta1-adrenergic receptor? A. Metaproterenol B. Propranolol C. *Nebivolol D. Terbutalin E. Esmolol 77. Is a specific alpha-adrenergic antagonist: A. *Prazosin B. Timolol C. Labetalol D. Atenolol E. Sotalol 78. Labetalol is: A. is a specific alpha-adrenergic antagonist B. *a selective alpha-adrenergic antagonistas well as a nonspecific beta-adrenergic antagonist C. is a nonspecific beta-adrenergic antagonist D. is a selective beta1-adrenergic blocker E. Neither 79. Weakness or dizziness, especially with activity or exercise – adverse effects of: A. Doxasozin B. *Propranolol C. Lidocaine D. Novocainamid E. Verapamil 80. Adverse effects of beta-blockers are: A. hypotension, dizziness, tachycardia B. hypotension, dizziness, lightheadedness C. headache, heart failure, pulmonary edema, D. nausea and constipation E. *bradycardia, bronchospasm, heart failure 81. Call calcium channel blockers with prolong action: A. *Felodipine B. Verapamil C. Diltiazem D. Nifedipine E. Nebivolol 82. Amlodipine and verapamil both: A. *cause coronary vasodilation B. depress atrioventricular nodal conduction C. cause reflex tachycardia D. stimulate calcium entry into cells E. None of the above 83. Which of the following agents is selective for beta1-adrenergic receptor? A. Salmeterol B. Propranolol C. *Bisoprolol D. Terbutalin E. Timolol 84. Selective blockade of beta1-adrenergic receptors: A. Amiodaron B. Lisinopril C. Timolol D. *Atenolol E. Sotalol 85. Labetalol is A. Neither B. is a specific alpha-adrenergic antagonist C. is a nonspecific beta-adrenergic antagonist D. is a selective beta1-adrenergic blocker E. *a selective alpha-adrenergic antagonists well as a nonspecific beta-adrenergic antagonist 86. Which of the following agents is (are) pure beta1-adrenergic agonists? A. *Bisoprolol B. Sotalol C. Albuterol D. Isoproterenol E. Timolol 87. Which one of the following drugs is useful in treating tachycardia? A. *Bisoprolol B. Phentolamine C. Isoproterenol D. Phenoxybenzamine E. Prazosin 88. Adverse effects of beta-adrenoblockers agents are: A. hypotension, dizziness, tachycardia B. hypotension, dizziness, lightheadedness C. headache, heart failure, pulmonary edema, D. nausea and constipation E. *bradycardia, bronchospasm, heart failure 89. Adverse effects of nifedipine are: A. bradycardia, bronchospasm, heart failure B. *dizziness, lightheadedness, peripheral edema, constipation C. hypotension, tachycardia, headache D. palpitations and headache E. hypotension, dizziness 90. Call calcium channel blockers with prolong action: A. *Isradipine B. Nifedipine C. Diltiazem D. Verapamil E. Nebivolol 91. Weight gain & edema occur in patients with congestive heart failure in response to: A. increased diuresis B. *increased aldosterone levels C. decreased renin levels decreased total peripheral resistance D. decreased venous capacitance E. None of the above 92. A drug that is NOT known to increase the effect or toxicity of digoxin when given concominantly: A. furosemide B. verapamil C. amiodarone D. *propranolol E. quinidine 93. Automaticity in Purkinje fibers can be most enhanced by: A. hypercalcemia B. vagal stimulation C. hyponatremia D. *catecholamines E. lidocaine 94. A drug used in the treatment of systolic congestive heart failure that shifts the Frank Starling curve upwards and to the left, and produces its effects by inhibiting the cardiac Na/K pump: A. Furosemide B. Nifedipine C. Captopril D. Clonidine E. *Digoxin 95. In the treatment of congestive heart failure, choose a drug that would reduce dyspnea and pulmonary edema by decreasing the left ventricular preload: A. Hydralazine B. Propranolol C. *Isosorbide dinitrate D. Dobutamine E. Digoxin 96. Sodium nitroprusside: A. *is used to lower blood pressure in a hypertensive emergency B. increases smooth muscle cAMP levels C. is given orally D. has a slow onset and long duration of action E. inhibits nitric oxide formation 97. To indicate the antihypertensive drug used for the medical treatment of hypertensive disease with tachycardia and extrasystoles. A. Reserpinum B. Methyldopa C. *Anaprilinum D. Clophelinum E. Dibazolum 98. To indicate the possible side effect of Anaprilinum? A. *Bronchial spasm B. Tachycardia C. Ortostatic collapse D. Rise of АP E. Development of tolerance 99. To indicate an antihypertensive drug from the calcium channels blockers. A. Anaprilinum B. Captopril C. Dibazolum D. *Verapamilum E. Reserpinum 100. Acebutolol is: A. *Beta-adrenoreceptor antagonist B. Calcium channel blocker C. Beta-adrenoreceptor agonist D. Angiotensin II receptor antagonists E. ACE inhibitor 101. The patient suffer from hypertensive disease with bradiarrhythmia. What drug is necessary to prescribe? A. Papaverinum B. Platyphyllini hydrotartras C. Ceftriaxone D. *Methyldopa E. Paracetamol 102. Indicate the Verapamil possible side effect, as antiarrhythmic drug: A. Tachycardia B. Bronchospasm C. Stenocardia D. Mouth dryness E. *Decrease of artery pressure (hypotension) 103. What diuretic has potassium-sparing action? A. Furosemide B. Mannitol C. Dihlothiazid D. *Triamterene E. Urea 104. What diuretic is used for forced diuresis? A. Dihlothiazid B. Triamterene C. Spironolactone D. *Furosemide E. Diacarb 105. What diuretic is belonging to osmotic diuretics? A. Spironolactone B. *Mannitol C. Furosemide D. Dihlothiazid E. Triamterene 106. Treatment of digoxin overdose may include all the following EXCEPT A. withdrawal of digoxin B. intravenous injection of Fab fragments of digitalis antibodies C. potassium supplements D. antiarrhythmic drugs E. *cholestyramine to break enterohepatic circulation 107. Agents that cause accumulation of cyclic AMP produce all of the following except: A. increased cardiac contractility B. *inhibition of Na+/K+-ATPase C. increased entry of Ca2+ via voltage-operated L channels in heart D. increased uptake of Ca2+ by the sarcoplasmic reticulum in heart E. arteriolar vasodilation 108. Which of the following drugs is LEAST apt to enhance the toxicity of digoxin? A. verapamil B. furosemide C. *triamterene D. hydrochlorothiazide E. quinidine 109. The administration of digoxin to a patient with congestive heart failure results eventually in a decrease in all of the following parameters EXCEPT A. heart rate B. end-diastolic pressure C. arteriolar resistance D. *AV node refractoriness E. renal sodium and water retention 110. Each of the following agents is useful to treat diastolic heart failure EXCEPT: A. lisinopril B. *digoxin C. verapamil D. furosemide E. carvedilol 111. Which of the following maneuvers is the most likely to improve renal perfusion in a patient treated for acute cardiac failure? A. administration of phenylephrine B. administration of propranolol C. injection of esmolol D. *administration of dopamine E. administration of epinephrine 112. The drugs whose international common name ends in - sentan such as bosentan, are: A. ACE (angiotensin converting enzyme) inhibitors B. progestogens C. *antagonists of endothelin receptors D. agonists of adenosine receptors E. directly acting cholinomimetic drugs 113. Clonidine lowers blood pressure: A. by inhibiting endothelin receptors B. by inhibiting alpha-1 adrenergic receptors C. by inhibiting angiotensin converting enzyme D. *by stimulating central alpha-2 adrenergic receptors E. by inhibiting beta-adrenergic receptors 114. Sartan: the drugs whose international common name ends by the suffix - sartan are: A. antineoplastic agents B. antiemetic agents C. antihypertensive drugs D. *angiotensin II receptor antagonists E. enkephalin receptor antagonists 115. Pril: the drugs whose international common name ends in the suffix – pril are: A. anorectics B. inhibitors of type V phosphodiesterases C. *ACE (angiotensin converting enzyme) inhibitors D. agonists of alpha- adrenergic receptors E. antidiarrheal drugs 116. During treatment, a patient develops a drug-induced dry cough. The drugs possibly responsible for this cough are: A. codeine B. diclofenac C. indomethacine D. *perindopril E. acetaminophen 117. During a treatment, an patient develops a drug-induced dry cough. The drug(s) possibly responsible for this cough is (are): A. propanolol B. indomethacine C. *captopril D. perindopril E. acetaminophen 118. Item: eliminated primarily by renal excretion Agents: Digoxin, Digitoxin, Strophanthin A. *The item is associated only with agents Digoxin & Strophanthin B. The item is associated only with agent Digoxin C. The item is associated only with agent Digitoxin D. The item is associated only with agent Strophanthin E. None of the above. 119. Item: has direct vasodilating effects Agents: Milrinone, Digoxin, Digitoxin A. *The item is associated only with agent Milrinone B. The item is associated only with agent Digoxin C. The item is associated only with agent Digitoxin D. The item is associated with agents Milrinone, Digoxin, Digitoxin E. None f the above 120. Weight gain & edema occur in patients with congestive heart failure in response to: A. *increased aldosterone levels B. increased diuresis C. decreased renin levels D. decreased total peripheral resistance E. decreased venous capacitance 121. The mechanism by which digoxin causes a positive inotropic effect on heart tissue is by: A. increasing ATP hydrolysis B. stimulating the Na/K pump C. *increasing intracellular Na and Ca D. sensitizing the heart to catecholamines E. inhibiting the Na/H exchanger 122. A drug that is NOT known to increase the effect or toxicity of digoxin when given concominantly: A. furosemide B. verapamil C. amiodarone D. *propranolol E. quinidine 123. A side effect of furosemide that can increase the automaticity of ectopic cardiac pacemakers: A. hypercalcemia B. hyperkalemia C. *hypokalemia D. hyponatremia E. hypothyroidism 124. Antihypertensive drug belonging to the same class: A. Doxazosin (Cardura), prazosin (Minipress), metoprolol (Lopressor) B. *nifedipine (Procardia, Adalat), verapamil (Isoptin, Calan), diltiazem (Cardiazem) C. Clonidine (Catapres), guanabenz (Wytensin),terazosin (Hytrin) D. Lisinopril (Prinvivil, Zestril), fosinopril (Monopril), guanadrel (Hylorel) E. None of the above 125. Mechanism of action: prasosin (Minipress) A. *alpha-1 receptor blocker B. beta receptor blocker C. phosphodiesterase inhibitor D. calcium channel blocker E. none of the above 126. Side effects of this antihypertensive agent includes tachycardia, angina, reversible lupus-like syndrome A. propranolol (Inderal) B. mecamylamine (Inversine) C. *hydralazine (Apresoline) D. Diazoxide (hyperstat) E. none of the above 127. Vasoconstriction, aldosterone secretion, and renin release suppression occur upon activation of the renin-angiotensin-aldosterone system. How would captopril (Capoten) affect these responses? A. *blocks all three B. blocks only vasoconstriction C. X blocks all except vasoconstriction D. X no effect E. Block none 128. Antihypertensive drug LEAST likely to elevate serum lipids: A. propranolol (Inderal) B. metoprolol (Lopressor) C. Chlorothiazide (Diuril) D. *diltiazem (Cardiazem) E. atenolol 129. Drug intervention for acute management of aortic dissection in which the objective is to reduce shear forces generated by blood flow: A. hydralazine (Apresoline) B. nitroprusside sodium (Nipride) C. *nitroprusside sodium (Nipride) + propranolol (Inderal) D. minoxidil E. None of the above 130. Tachycardia observed after minoxidil (Loniten) may be blocked by: A. mecamylamine (Inversine) B. propranolol (Inderal) C. *both D. Neither E. All of the above 131. Antihypertensive drugs belonging to the same class: A. doxazosin (Cardura), prazosin (Minipress), metoprolol (Lopressor) B. *nifedipine (Procardia, Adalat), verapamil (Isoptin, Calan), diltiazem (Cardiazem) C. clonidine (Catapres), guanabenz (Wytensin),terazosin (Hytrin) D. lisinopril (Prinvivil, Zestril), fosinopril (Monopril), guanadrel (Hylorel) E. None of the above 132. Mechanism of action: prazosin (Minipress) A. *alpha-1 receptor blocker B. beta receptor blocker C. phosphodiesterase inhibitor D. calcium channel blocker E. none of the above 133. Mechanism of action:diltiazem (Cardiazem) A. phosphodiesterase inhibitor B. *blockade of calcium channels C. alpha-1 receptor antagonists D. beta-1 receptor antagonist E. all of the above 134. Side effects of this antihypertensive agent includes tachycardia, angina, reversible lupus-like syndrome A. propranolol (Inderal) B. mecamylamine (Inversine) C. *hydralazine (Apresoline) D. diazoxide (Hyperstat) E. none of the above 135. I.v. route of administration; few side effects; effective in treating hypertensive crisis: A. nifedipine (Procardia, Adalat) B. *nitroprusside sodium (Nipride) C. nicardipine (Cardene) D. all of the above E. none of the above 136. Vasoconstriction, aldosterone secretion, and renin release suppression occur upon activation of the renin-angiotensin-aldosterone system. How would captopril (Capoten) affect these responses? A. *blocks all three B. blocks only vasoconstriction C. blocks all except vasoconstriction D. no effect E. none of the above 137. Antihypertensive drug LEAST likely to elevate serum lipids: A. propranolol (Inderal) B. metoprolol (Lopressor) C. chlorothiazide (Diuril) D. *diltiazem (Cardiazem) E. all of the above 138. Drug intervention for acute management of aortic dissection in which the objective is to reduce shear forces generated by blood flow: A. hydralazine (Apresoline) B. nitroprusside sodium (Nipride) C. *nitroprusside sodium (Nipride) + propranolol (Inderal) D. all of the above E. none of the above 139. Tachycardia observed after minoxidil (Loniten) may be blocked by: A. mecamylamine (Inversine) B. propranolol (Inderal) C. *both D. avoid vomitting E. none of the above 140. Calcium channel blocker: vasodilation, less likely to have direct cardiac effects: A. nifedipine (Procardia, Adalat) B. diltiazem (Cardiazem) C. *nifedipine + diltiazem D. nimodipine E. none of the above 141. Total peripheral resistance (TPR) is a determining factor for mean arterial pressure, i.e. Mean arterial pressure (MAP) = cardiac output x total peripheral resistance (TPR). What are correct relationships between norepinephrine, minoxidil, and lisinopril and TPR? A. minoxidil (Loniten): TPR increases B. fosinopril (Monopril): TPR increases C. *norepinephrine (Levophed): TPR increases D. phenoxybenzamine (Dibenzyline): TPR increases E. Mioxodil (loniten) TPR increase 142. Ganglionic blocker: A. prazosin (Minipress) B. hydralazine (Apresoline) C. *mecamylamine (Inversine) D. nicardipine (Cardene) E. None of the above 143. Minoxidil (Loniten) administration produces arteriolar vasodilation with little effect on capacitance vessels. Drug(s) acting similarly: A. nitroprusside sodium (Nipride) B. propranolol (Inderal) C. *hydralazine (Apresoline) D. all of the above E. None of the above 144. Blocks both alpha and beta receptors: A. timolol (Blocadren) B. *labetalol (Trandate, Normodyne) C. propranolol (Inderal) D. diazoxide (Hyperstat) E. all of the above 145. Hypertensive emergencies: A. diltiazem (Cardiazem) B. *nitroprusside sodium (Nipride) C. reserpine D. phenylephrine (Neo-Synephrine) E. all of the above 146. ACE inhibitor A. nifedipine (Procardia, Adalat) B. *captopril (Capoten) C. timolol (Blocadren) D. methyldopa (Aldomet) E. None of the above 147. Antihypertensive: action based on inhibition of norepinephrine release from adrenergic nerve endings: A. propranolol (Inderal) B. *guanadrel (Hylorel) C. mecamylamine (Inversine) D. phentolamine (Regitine) E. None of the above 148. Initiators of baroreceptor reflexes: A. peripheral chemoreceptors B. capillary pressure receptors C. *stretch receptors located in the wall of large chest and neck arteries D. all of the above E. None of the above 149. Causes of hypertension: A. Cushing's disease B. oral contraceptives C. acromegaly D. polycystic kidney disease E. *all of the above 150. Starling's Law and related matters: A. As blood volume returning to the hard increases,ventricular dilation is reduced B. Generally, increase preloaded an increase contractility lead to decreased stroke volume C. *According to Starling's Law, increased ventricular stretch usually leads to increased myocardial contractility D. all of the above E. None of the above 151. The most specific agent for prevention of asthma is: A. *Salbutamolum B. Libexinum C. Adrenalini hydrochloridum D. Pertussinum E. Mucaltinum 152. Theophylline clearance may be reduced by: A. phenobarbital B. warfarin C. tobacco smoking D. phenytoin E. *ciprofloxacin 153. Factors which are important to consider in selecting a maintenance dose of theophylline in a patient include all of the following EXCEPT: A. smoking history B. concomitant medication administration C. presence of congestive heart failure or cor pulmonale D. presence of hepatic failure E. *presence of renal insufficiency 154. Manifestations of theophylline toxicity may include all of the following EXCEPT: A. tremors B. seizures C. tachyarrhythmias D. vomiting E. *hyperkalemia 155. In the case of an oral overdose of theophylline, clearance may be enhanced by: induction of emesis A. *oral pulse dose charcoal B. administration of cimetidine C. lavage of nasogastric contents D. forced diuresis E. None of the above 156. Regarding its actions, cromolyn is best described as: A. bronchodilator B. anticholinergic C. beta agonist D. *inhibitor of mast cell degranulation E. glucocorticoid 157. Beta-2 selective adrenergic agonists include all EXCEPT: A. terbutaline B. albuterol C. metaproterenol D. *isoproterenol E. pirbuterol 158. Adverse effects of beta-2 adrenergic bronchodilators include all of the following EXCEPT: A. nervousness B. headache C. tachycardia D. tremulousness E. *lethargy 159. Which of the following work through cholinergic receptor antagonism? A. isoetharine B. cromolyn C. ephedrine D. *ipratropium E. salmeterol 160. Which of the following pharmacologic agents antagonize adenosine? A. *theophylline B. glucocorticoids C. cromolyn sodium D. propranolol E. terbutaline 161. Theophylline, ethacrynic acid, and furosemide: A. interfere with active renal tubular reabsorption of sodium B. *increase urine volume C. are not effective in the treatment of congestive heart failure D. decrease excretion of sodium in the urine E. may precipitate in renal tubules and cause acute angiospastic necrosis 162. When comparing the relative adrenergic effects of the following drugs, the one which would have the least 2 (bronchodilatation) effect at normal doses is: A. terbutaline B. epinephrine C. isoproterenol D. isoetharine E. *norepinephrine. 163. Asthmatic patients could experience bronchoconstriction problems with which of the following agents? A. isoproterinol (Isuprel) B. digoxin (Lanoxin) C. *pindolol (Visken) D. dextromethorphan E. All of the above 164. The agent with immune boosting activity yet recently implicated with causing severe depression and suicidal ideation is: A. Echinacea B. *interferon C. dronabinol (Marinol) D. megestrol (Megace) E. All of the above 165. Typically associated with B cell proliferation and differentiation into antibody-secreting plasma cells A. tumor necrosis factor beta B. interferon-gamma C. *IL-4 (interleukin 4) D. IL-2 (interleukin 2) E. all of the above 166. T helper lymphocytes -- regulate each other; this substance produced by TH1cells inhibits TH2 cellular proliferation: A. interleukin-2 B. tumor necrosis factor beta C. *interferon-gamma D. IL-4 E. IL-6 167. Activated cytotoxic T cells induce target cell death (virus-infected cells) by: A. Fas-Fas ligand apotosis pathway B. lytic granule enzymes C. perforin D. *all C, D, B, E are correct E. none of the above 168. Examples of autoimmune diseases A. rheumatoid arthritis B. insulin-dependent diabetes mellitus C. systemic lupus erythematosis D. rheumatoid arthritis & systemic lupus erythematosis & C E. *rheumatoid arthritis, insulin-dependent diabetes mellitus, systemic lupus erythematosis, B & C 169. Which of the following asthma severity categories has a treatment including inhaled low-dose steroid, cromolyn, nedocromil, zafirlukast or zileuton? A. Mild intermittent asthma B. *Mild persistent asthma C. Moderated persistent asthma D. Severe persistent asthma E. Exercise-induced asthma 170. Which of the following combinations is false? A. Omalizumab - monoclonal anti IgE B. Zileuton - Hepatotoxicity C. Cromolyn Na - No side effects D. *Albuterol - Status asthmaticus E. Prednisolone - teratogeneciticy 171. Which of the following drugs acts through a cytosolic receptor? A. Cromolyn sodium B. *Beclomethasone C. Zafirlukast D. E. 172. A. B. C. D. E. 173. A. B. C. D. E. 174. A. B. C. D. E. 175. A. B. C. D. E. 176. A. B. C. D. E. 177. A. B. C. D. E. Omalizumab None of the above Which of the following corticosteroids is used for quick relief from asthma? Triamcinolone *Dexamethasone Budesonide Beclomethasone Fluticasone Which of the following is not true about Salmeterol? administered by inhalation long acting anti-asthmatic with a duration of 12 hour *can lead to transient increase in PaO2, especially in poorly ventilated lung tissue associated with improvement in patients homozygous for glycine at the B-16 locus of the betareceptor none of the above Which of the following is not true about Ipratropium bromide: Anticholinergic agent administered by inhalation better bronchodilator than Atropine *better anti-asthmatic than Epinephrine has no effect on mucocilliary clearance none of the above Which of the following is not a quick relief medication for asthma? Epinephrine Ipratropium bromide Prednisolone *Flunisolide All of the above The following is not true of beta-2 adrenergic agonists: cause bronchodilation by decreasing cytosolic Ca2+ cause hypotension * decrease mucocilliary activity decrease bronchial vascular permeability increase heart rate Which of the following can be administered orally and by inhalation? Epinephrine Albuterol Pirbuterol *Terbutaline Isoproterenol Situational tasks 1. A patient admitted to the hospital with a diagnosis of pneumonia asks the nurse why she is receiving codeine when she does not have any pain. The nurse's response is based on knowledge that codeine also has what effect? A. Immunostimulant. B. *Antitussive. C. Expectorant. D. Immunosuppressant. E. Antihistamine. 2. Mother, whose child suffered from dry cough that did not let her to sleep at night, consulted a pediatrician. What preparation can’t be used in such case? A. Libexyn. 3. 4. 5. 6. 7. 8. B. Tusuprex. C. *Codeine. D. Bromhexyn. E. Acetylcistein. An 81-year-old female with arteriosclerotic heart disease and pulmonaryemphysema was found to have significant bronchospasm. Her physician prescribed theophylline 400 mg every 12 hours. All of the following toxicities may be observed EXCEPT: A. cardiac arrhythmias B. nausea C. agitation D. *sodium and water retention E. vomiting When comparing the relative adrenergic effects of the following drugs, the one which would have the least bronchodilatation effect at normal doses is: A. terbutaline B. epinephrine C. isoproterenol D. isoetharine E. *norepinephrine. The combination of hydralazine and nitrates has been shown to improve survival in patients of heart failure. All of the following statements about this combination are true except: A. The combination serves to decrease both afterload and preload. B. *Prazosin is as effective as the combination in treatment of congestive heart failure. C. The concept of afterload reduction is principally derived from patients of significant mitral regurgitation. D. The VA cooperative study was a landmark trial demonstrating the beneficial effect of hydralazine and nitrate combination in patients of heart failure. E. None of the above A 45-year-old woman has had recurrent episodes of atrial fibrillation. She is receiving phenytoin and quinidine to control the atrial fibrillation. She is also taking a low dose of diazepam for insomnia and estrogen replacement therapy.You learn today that she has been receiving ciprofloxacin for a urinary track infection.The reason for her appointment today is that she has been having ringing in the ears, headache, nausea, and blurred vision. She tells you that she is also having trouble hearing the television. You suspect drug toxicity.The most likely agent is: A. Ciprofloxacin B. Estrogen C. Phenytoin D. Diazepam E. *Quinidine You are asked to treat a 55-year-old patient for continuing ventricular arrhythmias.The patient is receiving timolol drops for glaucoma, daily insulin injections for diabetes mellitus, and an ACE inhibitor for hypertension.You decide to use phenytoin instead of procainamide because of what pharmacological effect of procainamide? A. The local anesthetic effect of procainamide would potentiate diabetes. B. *The anticholinergic effect of procainamide would aggravate glaucoma. C. The hypertensive effects of procainamide would aggravate the hypertension. D. The local anesthetic effect of procainamide would aggravate the hypertension. E. The cholinergic effects of procainamide would aggravate the diabetes. Exercise-induced ventricular tachycardia in persons without overt cardiac disease is an example of delayed after-depolarizations and is characterized by an increase in intracellular ionized calcium.This type of arrhythmia is known to often respond well to which of the following combinations? A. Beta-Blocker and ACE inhibitor B. *Calcium channel antagonist and ACE inhibitor C. Beta-blocker and ACE inhibitor D. Beta-blocker and calcium channel antagonist E. Alpa-blocker and calcium channel antagonist 9. Metoprolol would produce which beneficial effect in a patient with secondary angina? A. A decrease in preload B. An increase in collateral blood flow C. An increase in afterload D. *An increase in diastolic filling time E. An increase in blood flow through a concentric stenosis 10. Although most antiarrhythmic drugs (and indeed most drugs) are chemically synthesized, some compounds that occur endogenously in humans are useful. Indicate which of the following agents occurs endogenously and is a useful antiarrhythmic agent. A. Phenytoin B. Digoxin C. *Adenosine D. Quinine E. Lidocaine 11. A patient comes to your office with effort-induced angina and resting tachycardia.You choose the following drug to treat the patient because it slows heart rate by blocking L-type calcium channels in the SA node: A. *Verapamil B. Propranolol C. Nitroglycerin D. Isosorbide dinitrate E. Metoprolol 12. Which of the following hemodynamic effects of nitroglycerin are primarily responsible for the beneficial results observed in patients with secondary angina? A. Reduction in the force of myocardial contraction B. Reduction in systemic vascular resistance (afterload) C. Increased heart rate D. *Reduction in venous capacitance (preload) E. Increased blood flow to the subepicardium 13. A woman is prescribed a combination of drugs consisting of a nitroglycerin patch and a beta-blocker, such as propranolol, to treat her attacks of secondary angina.Which effect of propranolol would counteract an adverse effect of nitroglycerin? A. A decrease in preload B. A decrease in afterload C. *A decrease in heart rate D. An increase in myocardial contractile force E. A reduction in coronary vasospasm 14. A patient who has been taking propranolol for a long period for secondary angina comes to your office complaining of increased frequency of chest pains on exertion.You decide to stop the propranolol and give him diltiazem because you suspect he has a mixture of secondary and primary angina. Why would diltiazem be more likely to relieve the angina if your new diagnosis is accurate? A. Diltiazem produces a decrease in heart rate. B. *Diltiazem dilates coronary blood vessels in spasm. C. Diltiazem produces AV blockade. D. Diltiazem reduces myocardial contractility. E. Diltiazem reduces afterload. 15. An accurate statement regarding the actions of both ACE inhibitors and AT1 receptor antagonists is that A. Both classes of drugs increase bradykinin. B. Angiotensin II can act at the AT2 receptor with both classes of drugs. C. *Both classes of drugs reduce total peripheral resistance. D. Both classes of drugs decrease circulating angiotensin II levels. E. Both classes of drugs are first-choice treatments for congestive heart failure. 16. Angiotensin II can: A. *Increase the synthesis and release of aldosterone B. Reduce the activity of the sympathetic nervous system C. Be a potent positive inotropic at the heart D. Relax vascular smooth muscle E. Reduce the growth of cardiovascular cell types 17. The most potent vasoconstrictor known is A. Bradykinin B. Angiotensin II C. Angiotensin IV D. Natriuretic peptide E. *Endothelin 18. The mechanism of action of captopril is A. Angiotensin receptor antagonist B. *ACE inhibitor C. Aldosterone receptor antagonist D. Bradykinin antagonist E. None of the above 19. Which of the following antihypertensive agents would decrease renin release? A. Prazosin B. *Clonidine C. Captopril D. Nitroprusside E. Diazoxide 20. Which of the following statements most accurately characterize the cellular action of the calcium channel blockers? A. Their interaction with membrane phospholipids results in a nonselective decrease of ion transport. B. They inhibit the Na+–Ca++ exchanger in cardiac and smooth muscle. C. *They interact at three distinct sites at the L-type voltage-gated calcium channels. D. Their interaction with the sodium pump results in an inhibition of calcium transport. E. All of the above 21. Which of the following calcium channel blockers would be most likely to suppress atrial tachyarrhythmias involving the A-V node? A. Nifedipine B. *Verapamil C. Nicardipine D. Amlodipine E. Nimodipine 22. All of the following statements are applicable with regard to the systemic effects caused by nifedipine EXCEPT: A. It typically causes peripheral vasodilation. B. It often elicits reflex tachycardia. C. It causes coronary vasodilatation D. It increases coronary blood flow. E. *Its benefit in the management of angina is related to the reduction in preload that it induces. 23. All of the following statements regarding the pharmacokinetics of calcium channel blockers are correct EXCEPT A. They are characterized by significant amount (~ 90%) of protein binding. B. They undergo significant first-pass metabolism. C. *Their half-life is not altered by hepatic cirrhosis. D. They can be administered orally. E. All of the above 24. All of the following adverse effects are likely to occur with long-term use of calcium channel blockers EXCEPT A. *Skeletal muscle weakness B. Flushing C. Dizziness D. Headache E. None of the above 25. A 55-year-old patient has been referred to you. She complains about a skin rash and a cough. In the course of history taking, she tells you that she takes high blood pressure medication but she doesn’t remember the name.You suspect a drug toxicity. Which of the following antihypertensive agents is the patient most likely taking? A. *Captopril B. Nifedipine C. Prazosin D. Propanolol E. Clonidine 26. Which of the following compounds depends least upon the release of EDRF (nitric oxide) from endothelial cells to cause vasodilation? A. Bradykinin B. Histamine C. *Minoxidil D. Hydralazine E. Acetylcholine 27. Which of the following antihypertensive drugs is contraindicated in a hypertensive patient with a pheochromocytoma? A. Metyrosine B. Labetalol C. Prazosin D. Phenoxybenzamine E. *Guanethidine 28. When a patient is treated with a thiazide diuretic for hypertension, all of the following are likely EXCEPT: A. The fall of blood pressure that occurs in the first 2 weeks of therapy results from a decrease of extracellular volume. B. The sustained fall in blood pressure that occurs after several weeks of therapy is due to a decrease of intravascular resistance. C. After the blood pressure is reduced, hypokalemia remains a complication. D. Hyperuricemia may occur. E. *Hypoglycemia may occur. 29. Furosemide increases the excretion of all of the following EXCEPT: A. Na+ B. K+ C. Ca++ D. Mg++ E. *Uric acid 30. Which of the following drugs is an appropriate initial antihypertensive therapy in an otherwise healthy adult with mild hypertension? A. Bumetanide B. Triamterene C. *Hydrochlorothiazide D. Aldactone E. Furosemid 31. When furosemide is administered to a patient with pulmonary edema, there is often symptomatic relief within 5 minutes of starting treatment.This relief is primarily due to: A. A rapid diuretic effect B. *An increase in venous capacitance C. A direct effect on myocardial contractility D. Psychological effects E. All of the above 32. A 60-year-old man with unstable angina pectoris fails to respond to heparin, nitroglycerin, beta adrenegic blockers and calcium channel antagonisst. What is the best treatment for this patient? A. Aspirin, orally B. *Coronary artery bypass grafting C. Antihypertensive therapy D. Intravenous strpetokinase E. Excercise testing 33. A 5-year-old child had an attack of palpitation with nausea, dizziness, generalized fatigue. On ECG: tachycardia with heartbeat rate of 220/min. Ventricle complexes are deformed and widened. P wave is absent. What medication is to be prescribed to provide first aid? A. *Lydocain B. Seduxen C. Novocainamides D. Strophantin E. Isoptin 34. A 46-year-old patient has ischemic heart disease, angina on exertion, II functional class. What is the drug of choice in treatment of acute attack? A. *Nitroglycerin sublingually B. Platelet inhibiting agents (aspirin) C. Spasmolitics (No-spa) IV D. Digitalis IV E. Sedative agents (Seduxenum) orally 35. A 52-year-old patient complains of intensive and prolonged retrosternal pains, decreased exercise tolerance for 5 days. Which of the following groops is the most useful? A. *nitrates B. dyslipidemic drugs C. diuretics D. ACE inhibitors E. digitalis 36. A 50-year-old patient was admitted to resusitation department with aqute myocardial infarction . Which one of the following drugs is uneffective in this case? A. Proranolol B. Nitroglycerin C. *Nifedipine D. Phentanyl E. Morfin 37. A 54-year-old patient, who suffers from IHD, stable stenocardia II, heart insufficiency I, has an attack of ventricular tachycardia, Ps 180/min, AP – 80/50 mm Hg. Choose a correct treatment: A. *Lidocain, potassium chloride B. Mezaton, strofantin C. Verapamil, potassium chloride D. Digoxin E. ATP, cordaron 38. A 55-year-old men has stenocardia on exertion II. Taking of nitroglycerin potentiate a sever headache. Which of the following drugs is the most useful in this case? A. *Molsidomin B. Amiodaron C. Nifedipine D. Propranolol E. Verapamil 39. A 49-year-old patient has ischemic heart disease, angina on exertion, II functional class. What is the drug of choice in treatment of acute attack? A. No-spa IV B. Aspirin C. Digitalis IV D. *Nitroglycerin sublingually E. Seduxenum orally 40. A patient of 42 year has arterial hypertension with bradyarrhythmia. Which of the following drugs is necessary to administer? A. Klonidine B. Bisoprolol C. *Nifedipine D. Diltiazem E. Methyldopa 41. A 58-year-old women, who suffers from IHD, stenocardia on exertion II, heart insufficiency I, has an attack of ventricular tachycardia, Ps 180/min, AP – 80/50 mm Hg. Choose a correct treatment: A. Digoxin, mezaton B. *Lidocain, potassium chloride C. Verapamil, potassium chloride D. Digoxin E. ATP, cordaron 42. A 55-year-old men has stenocardia on exertion II. Taking of nitroglycerin potentiate a sever headache. Which of the following drugs is the most useful in this case? A. Aspirin B. *Molsidomin C. Captopril D. Propranolol E. Verapamil 43. A 6 month old patient who is in the ICU following cardiac surgery for a congenital defect develops atrial flutter with an atrial rate of 300 beats/min and second degreee (2:1) AV node block. A 3rd year medical student inadvertantly administers quinidine, instead of propranolol,and the patient's ventricular rate skyrockets to 300 beats/min. The patient faints. This most likely occured because quinidine is: A. a partial beta agonist B. *antimuscarinic C. a sodium channel blocker D. a potassium channel blocker E. able to increase vagal tone 44. A 45-year-old women with diagnosis: Paroxysmal arrhythmia. Arterial hypertension II. Drug of choice for stopping attack: A. *Anaprilin B. Nitroglycerin C. Potassium chloride D. Digoxin E. Lidocain 45. A patient has arterial hypertension with bradyarrhythmia. Which of the following drugs is necessary to administer? A. *Nifedipine B. Klonidine. C. Propranolol D. Diltiazem E. Methyldopa 46. A patient has bronchial asthma for a long time. Angina pectoris attacks have appeared recently Which of the following drugs is contraindicated? A. *Propranolol B. Nitroglycerin C. Nifedipine D. Lovastatin E. Aspirin 47. A 64-year-old patient, who suffers from IHD, stable stenocardia II functional class, heart insufficiency I, has an attack of ventricular tachycardia, Ps 180/min, AP – 80/50 mm Hg. Choose a correct treatment: A. ATP, cordaron B. Mezaton, strofantin C. Verapamil, potassium chloride D. Digoxin E. *Lidocain, potassium chloride 48. A 45-year-old men with diagnosis: Paroxysmal arrhythmia. Arterial hypertension II. Drug of choice for stopping attack: A. *Metoprolol B. Nitroglycerin C. Potassium chloride D. Digoxin E. Lidocain 49. A patient of 42 year has arterial hypertension with bradyarrhythmia. Which of the following drugs is necessary to administer? A. Klonidine B. *Nifedipine C. Bisoprolol D. Diltiazem E. Methyldopa 50. A patient has bronchial asthma for a long time. Angina pectoris attacks have appeared recently. Which of the following drugs is contraindicated? A. *Propranolol B. Molsidomin C. Nifedipine D. Carvedilol E. Aspirin 51. A 65-year-old woman with unstable angina pectoris fails to respond to heparin, nitroglycerin, beta adrenegic blockers and calcium channel antagonists. What is the best treatment for this patient? A. Intravenous strpetokinase B. *Coronary artery bypass grafting C. Antihypertensive therapy D. Aspirin, orally E. Excercise testing 52. A 49-year-old women with diagnosis: Paroxysmal arrhythmia. Arterial hypertension II, heart insufficiency 0. Introduce drug of choice for stopping attack: A. *Metoprolol B. Nitroglycerin C. Potassium chloride D. Digoxin E. Lidocain 53. A patient suffers from arterial hypertension with bradyarrhythmia. Which of the following drugs is necessary to administer? A. Atenolol B. Furosemid. C. *Nifedipine D. Diltiazem E. Methyldopa 54. A patient has chronic obstructive pulmonary desease for a long time. Angina pectoris attacks have appeared recently. Which of the following drugs is contraindicated? A. Nifedipine B. Isosorbide dinitrate C. Lovastatin D. *Propranolol E. Aspirin 55. A woman 56 years old with hypertension edema develops on lower extremities, moist wheezes in the lower parts of lungs. What must be administered in the complex therapy of the patient? A. Beta-adrenomimetics, B. *Diuretics, C. Glucocorticoids, D. Preparations of calcium, E. M-cholinolitics. 56. A woman 51 years old has arterial hypertension. Which group of drugs may be used for her treatment? A. Betaadrenomimetics, B. *Angiotensin-converting enzyme inhibitors, C. Glucocorticoids, D. Preparations of calcium, E. M-cholinolitics. 57. A man 36, years old, has arterial hypertension. Which group of drugs may be used for her treatment? A. Beta-adrenomimetics B. Preparations of calcium, C. Glucocorticoids, D. *Calcium-channel inhibitors, E. M-cholinolitics. 58. Patients suffering from congestive heart failure will show signs and symptoms of peripheral vasoconstriction, moist skin, pale complextion because of: A. Na and water retention B. decreased renin release C. *increased sympathetic tone D. decreased vagal tone E. decreased aldosterone levels 59. A 67 year old patient with a history of heart disease presents to the ER with chronic atrial fibrillation, an average ventricular rate of 120-140 beats/min, and an ejection fraction of 35 %. The best drug for controlling his ventricular rate would be: A. propranolol B. quinidine C. nifedipine D. diltiazem E. *digoxin 60. A 76 year old patient being treated with digoxin, captopril and furosemide for systolic heart failure and hypertension presents to the ER with complaints of dizziness and fatigue. The patient faints immediately after an ECG recording indicates the presence of sinus bradycardia and intermittent 3rd degree AV conduction block. The most likely explanation for this patient's rhythm disturbance is: A. captopril overdose B. *increased vagal tone caused by digoxin C. decreased vagal tone caused by furosemide D. increased sympathetic tone caused by digoxin E. hyperkalemia caused by furosemide 61. A 59 year old patient with a history of systolic heart failure arrives in the ER with complaints of chest palpitations, nausea and GI upset. His chart indicates that he is currently taking digoxin, captopril, metoprolol and furosemide. A 12 lead ECG is recorded and reveals the presence of frequent runs of ventricular bigeminy. His echocardiogram indicates an ejection fraction of 40%. His blood tests indicate a serum potassium level of 4.0 mM, and an elevated digoxin level of 2.2 ng/ml. The most appropriate drug for treating this patient's arrhythmia would be: A. propranolol B. quinidine C. *lidocaine D. verapamil E. atropine 62. A patient being treated for heart failure with digoxin and furosemide is discharged from the hospital after being initiated on quinidine therapy to reduce the incidence of atrial tachyarrhythmias. The next day the patient reappears in your office complaining of fatigue, visual difficulties and nausea. The patient's ECG reveals a prolong PR interval, with occasional runs of bigeminy and 2nd degree (Mobitz type I) AV conduction block. The most likely cause of these symptoms is: A. furosemide induced hyperkalemia B. an interaction between quinidine and furosemide C. worsening heart failure D. *an interaction between quinidine and digoxin E. quinidine toxicity 63. A patient who is experiencing progressive dyspnea of effort comes to your office for a physical examination. The pulse is regular at 100 beats per minute, with a blood pressure of 126/84 mm Hg. Auscultation of the lungs reveals inspiratory crackles at both bases. There is no peripheral edema, and the cardiac apical impulse is not displaced. An echocardiogram reveals a left ventricular chamber that is not dilated, with an estimated ejection fraction of 55%. You make the diagnosis of congestive heart failure. Based on your observations, which of the following drugs would best address the problem in this patient? A. dopamine B. *verapamil C. digoxin D. hydralazine E. furosemide 64. The 56 years old woman with hypertensive disease appealed to the doctor. Methyldopa was prescribed to her. Indicate a mechanism of action of this drug. A. Violation of noradrenalin synthesis B. *alpha-adrenoreceptors blockers C. Block of beta-adrenoreceptors D. Depression of angiotensin converting enzyme activity E. Increasing of acetylcholine synthesis 65. In the complex medical treatment of hypertensive disease a diuretic was prescribed to the patient. In a few days the BP went down, but the signs of hypokaliaemia arose up. What drug could cause such complication? A. Triamterene B. Clofeline C. С. Enalapril D. Spironolactone E. *Furosemide 66. The patient has cranial trauma. The brain edema threat developed in the postoperative period. To prescribe drug for the removal of this complication. A. Spironolactone B. Papaverini hydrochloride C. *Furosemide D. Dihlothiazid E. Diacarb 67. In the patient with the considerable peripheral edema the by turns using of dihlothiazid, ethacrynic acid and furosemide did not result in the considerable diuretic effect. The analysis of blood indicated the considerable increasing of aldosteron level. Prescribe drug for treatment. A. Mannitol B. *Spironolactone C. Clopamid D. Triamterene E. Amiloride 68. To the 55 years old man for the medical treatment of gout was prescribed etamid. What is the mechanism of uric actions of the drug? A. *Depression of reabsorbing of urinary acid B. Increasing of secretion of urinary acid C. Decreasing of production of urinary acid D. Depression of activity of xantinoxydase E. Production of easy soluble salts 69. At the 46 years old patient with blink arrhythmia the edema of lungs began. What drug is necessary to inject in the first turn? A. *Furosemide B. Triamterene C. Verospirone D. Amiloride E. Euphylline 70. To the patient with edema of cardiac origin the doctor must prescribe diuretics. What drugs are contraindicated in this situation? A. Hypothiazide B. Spironolactone C. Furosemide D. *Mannitol E. Diacarb 71. In the patient with the considerable peripheral edema using of dihlothiazid did not result in the considerable diuretic effect. The analysis of blood indicated the considerable increasing of aldosteron level. Prescribe drug for treatment in this situation. A. Mannitol B. *Spironolactone C. Ethacrynic acid D. Furosemide E. Diacarb 72. In the complex medical treatment of hypertensive disease a diuretic was prescribed to the patient. In a few days the BP went down, but the signs of hypokaliaemia arose up. What drug could cause such complication? A. Triamterene B. Clofeline C. Enalapril D. Spironolactone E. *Furosemide 73. Patients suffering from congestive heart failure will show signs and symptoms of peripheral vasoconstriction, moist skin, pale complextion because of: A. Na and water retention B. decreased renin release C. *increased sympathetic tone D. decreased vagal tone E. decreased aldosterone levels 74. A 67 year old patient with a history of heart disease presents to the ER with chronic atrial fibrillation, an average ventricular rate of 120-140 beats/min, and an ejection fraction of 35%. The best drug for controlling his ventricular rate would be: A. verapamil B. quinidine C. nifedipine D. diltiazem E. *digoxin 75. A 76 year old patient being treated with digoxin, captopril and furosemide for systolic heart failure and hypertension presents to the ER with complaints of dizziness and fatigue. The patient faints immediately after an ECG recording indicates the presence of sinus bradycardia and intermittent 3rd degree AV conduction block. The most likely explanation for this patient's rhythm disturbance is: A. captopril overdose B. *increased vagal tone caused by digoxin C. decreased vagal tone caused by furosemide D. increased sympathetic tone caused by digoxin E. hyperkalemia caused by furosemide 76. A patient being treated for heart failure with digoxin and furosemide is discharged from the hospital after being initiated on quinidine therapy to reduce the incidence of atrial tachyarrhythmias. The next day the patient reappears in your office complaining of fatigue, visual difficulties and nausea. The patient's ECG reveals a prolong PR interval, with occasional runs of bigeminy and 2nd degree (Mobitz type I) AV conduction block. The most likely cause of these symptoms is: A. furosemide induced hyperkalemia B. an interaction between quinidine and furosemide C. worsening heart failure D. *an interaction between quinidine and digoxin E. quinidine toxicity 77. An elderly male patient has essential hypertension, congestive heart failure, and type I insulin-dependent diabetes. His congestive failure developed secondary to coronary vascular disease associated with hyperlipidemia. What antihypertensive drug(s) may be most appropriate for this patient? A. Chlorothiazide (Diuril) B. *captopril (Capoten) C. propranolol (Inderal) D. metoprolol (Lopressor) E. none of the above 78. An elderly male patient has essential hypertension, congestive heart failure, and type I insulin-dependent diabetes. His congestive failure developed secondary to coronary vascular disease associated with hyperlipidemia. What antihypertensive drug(s) may be most appropriate for this patient? A. chlorothiazide B. *lisinopril C. propranolol D. metoprolol E. all of the above 79. A patient presents with a blood pressure of 160/110 mm Hg. The patient has a history of coronary vascular disease, resulting in angina, but has no evidence of congestive heart failure. The patient also has asthma and has been treated mainly using terbutaline (Brethine), by aerosol inhalation Propranolol (Inderal) was prescribed to manage essential hypertension. Was this action appropriate? A. Propranolol (Inderal) is appropriate because it will reduce heart rate and cardiac output. Negative inotropism will help reduce the incidence of angina. It is an effective antihypertensive agent B. Propranolol (Inderal) is inappropriate because it is only useful in mild hypertension; a better drug would be minoxidil or hydralazine because they are more effective in lowering blood pressure C. Propranolol (Inderal) is appropriate because it is an effective, low-cost antihypertensive. It will augment the effects of terbutaline, an additional benefit D. *Propranolol (Inderal) is inappropriate because its use is contraindicated in a patient with asthma. E. all of the above 80. The patient with severe allergic bronchial asthma has been treated by oral drug during 7 months. Hypertension, “moon face”, obese trunk, oedema, insomnia occur. What drugs does he used? A. *Patient used one of orally used glucocorticoids, e.g. prednisolonum. B. Patient used one of beta-agonists. C. Patient used cromolynum. D. Patient used euphyllinum E. Patient used all above. 81. Patient 65 years old suffers from bronchial asthma. Adrenergic receptor activator is used for treatment, After two weeks of management a pain near heart, palpitation. How can these side effects be prevent? It is necessary to prescribe: A. *selective beta2-adrenergic receptor stimulator, for example salbutamolum. B. glucocorticoids. C. theophylline. D. anticholinergics E. cromolyn sodium. 82. An 81-year-old female with arteriosclerotic heart disease and pulmonary emphysema was found to have significant bronchospasm. Her physician prescribed theophylline 400 mg every 12 hours. All of the following toxicities may be observed EXCEPT: A. cardiac arrhythmias B. nausea and vomiting C. agitation D. *sodium and water retention E. tremulousness 83. A patient complains of severe expiratory dyspnea, paroxysmal dry cough, general asthenia. This condition lasts for 28 hours and is not benefite after usage of salbutamol. Data of examination: the patient is staying and leaning against window-still, diffuse cyanosis add swelling of neck veins are observed, weezes are heard on the distance, by percussion bundbox sound is heard, by auscultation – weakened wesicular breathing, elongated expiration, difuse dry rales. Which medical preparation is the most important for the patient? A. beta-agonists, B. beta-blockers; C. Expectorants: D. *Parenteral administrations of corticosteroids. E. M-cholinolithics, 84. During auscultation of patient P., 60 years old, with chronic non-obstructive bronchitis, dry buzzling rales above all parts of the lungs were heard as well as weakened vesicular breathing. What medical preparation is it necessary to prescribe to the patient? A. Diuretics; B. Antitussive agents; C. *Expectorants; D. Broncholitics; E. beta-blockers. 85. A 56-yr-old man wheezes and coughs. He has tried to give up smoking, but he finds it very difficult. He is thin and healthy looking with a rounded chest. His breathing is noisy. His cough is unproductive. What treatment has to be prescribed? A. Amoxycillin B. Prednisolone C. *Ipratropium D. Salbutamol E. Bronchial lavage 86. A 20-yr-old woman presents with a week's history of fever, rigors arid productive rusty cough. CXR shows right lower lobe consolidation. Prescribe treatment A. Erythromycin B. Co-trimoxazole C. Prednisolone D. *Amoxicillin E. Salbutamol inhaler Тests questions to figures 1. Specify minimal day's dose of the drug represented on figure 40: A. 1-2 mg B. 2-4 mg C. *5-10 mg D. 15-20 mg E. 50-60 mg 2. Specify minimal day's dose of the drug represented on figure 41: A. 10-20 mg B. 40-60 mg C. *2.5-5 mg D. 25-30 mg E. 0.5-1.0 mg 3. Specify minimal day's dose of the drug represented on figure 42: A. *60 mg B. 40mg C. 20 mg D. 10 mg E. 5 mg 4. Specify minimal day's dose of the drug represented on figure 43: A. 10 mg B. 40mg C. 25-30 mg D. *60 mg E. 0.5-1.0 mg 5. Specify minimal day's dose of the drug represented on figure 44: A. 10 mg B. 20 mg C. 25-30 mg D. *40 mg E. 5 mg 6. Specify minimal day's dose of the drug represented on figure 45: A. *1.25-1.5 mg B. 2.5-3.0mg C. 5-10 mg D. 10-20mg E. 0.5-1.0 mg 7. Specify minimal day's dose of the drug represented on figure 46: A. *2.5-10 mg B. 40mg C. 25-30 mg D. 60 mg E. 0.5-1.0 mg 8. Specify minimal day's dose of the drug represented on figure 47: A. 10 mg B. 80mg C. 25-30 mg D. *50 mg E. 100 mg 9. Specify minimal day's dose of the drug represented on figure 48: A. 100 mg B. 200mg C. 300 mg D. 400 mg E. *500 mg 10. The following statements concerning mechanism of diltiazem’ action (fig. 42) are true, EXCEPT: A. *Therapeutically active agents in this group are capable of releasing nitric oxide (NO) in vascular smooth muscle target tissues B. Calcium channel blockers bind to L-type calcium channel sites C. Calcium channel blockers useful in angina decrease myocardial oxygen requirement (by decreasing the determinations of oxygen demand) D. Calcium channel blockers increase myocardial oxygen delivery (by reversing coronary arterial spasm) E. Calcium channel blockers decrease transmembrane calcium current associated in smooth muscle with long-lasting relaxation and in a cardiac muscle with a reduction in contractility 11. What are contraindications to application represented on figure 49 drug? A. Arterial hypertension B. Heart failure C. *Hypertrophic obstructive cardiomyopathy, pheochromocytoma, ventricular fibrillation, increased sensitivity to dopamine. D. Myocardial infarction E. Pregnancy 12. The efficiency of Amlodipine (agent on fig. 41) at arterial hypertension is caused by: A. *The dilation of vessels B. The rise of myocardium contractility C. The decline of renine production D. The decline of diuresis E. The rise of diuresis 13. The basic principle of amlodipine action (agent on fig. 41): A. It increaseses the activity of potassium channels B. It blockades beta2 -adrenoreceptors C. The release of nitrogen oxide D. *It blockades the calcium channels L-type E. It blockades beta1 -adrenoreceptors 14. What are side effects caused by represented on figure 49 drug? A. tachycardia or bradycardia, chest pain. B. nausea, vomiting. C. Headache, anxiety. D. polyuria, bronchoconstriction, E. *All of the above 15. An efficiency of drug indicated on fig. 43 at angina pectoris is explained by A. *The removal of the sympathetic influences on the heart because of the blockade of the betaadrenoreceptors B. The expansion of the coronal vessels C. The increase of sympathetic influences on the heart D. The increase of cardiac abbreviations E. The decline of thrombocyte aggregation 16. Indicate the possible side effect of Propranolol indicated on fig. 43: A. *Bronchial spasm B. Tachycardia C. Rise of АP D. Ortostatic collapse E. Development of tolerance 17. Mechanism of indicated on fig. 46 lisinopril action: A. Blocks alpha-adrenoreceptors B. *Blocks carboxypeptidase C. Blocks M-cholinoreceptors D. Has diuretic action E. Has sympatholytic action 18. An annoying side effect of agent, indicated on fig. 46, that may be minimized by switching to an angiotensin receptor blocking agent includes: A. Orthostatic hypotension B. *A dry, nonproductive cough C. Fatigue D. Hypokalemia E. Hyperkalemia 19. Which of the following should not be taken concurrently with agent, indicated on fig. 46? A. Lasix B. Morphine C. *Potassium D. Natrium E. Vicasolum 20. All of the following effects of agent, indicated on fig. 46, may be useful in treating heart failure EXCEPT: A. It decrease afterload B. *It increase circulating catecholamine levels C. It reduce reactive myocardial hypertrophy D. It increase myocardial beta-1 adrenergic receptor density E. None of the above 21. All of the following statements concerning the use of agent, indicated on fig. 46, in the treatment of heart failure are true EXCEPT: A. It improve hemodynamics by decreasing afterload B. *It can increase plasma cholesterol levels C. It may slow the progression of heart failure by preventing myocardial and vascular remodeling D. It is effective first-line agents in the treatment of chronic heart failure E. All of the above are true 22. Drug, indicated on fig. 49, at low doses influences mainly: A. Alfa-adrenoreceptors (leads to peripheral vasoconstriction) B. *Dopamine receptors (leads to vasodilation of renal and mesenterial vessels) C. Beta-1 adrenoreceptors (leads to enhanced cardiac output) D. All of the above E. None of the above 23. Drug, indicated on fig. 49, at medium doses influences mainly: A. Alfa-adrenoreceptors (leads to peripheral vasoconstriction) B. Dopamine receptors (leads to vasodilation of renal and mesenterial vessels) C. *Beta-1 adrenoreceptors (leads to enhanced cardiac output) D. All of the above E. None of the above 24. Drug, indicated on fig. 49, in high doses influences mainly the: A. *Alfa-adrenoreceptors (leads to peripheral vasoconstriction) B. Dopamine’s receptors (leads to vasodilation of renal and mesenterial vessels) C. Beta-1 adrenoreceptors (leads to enhancing of cardiac output) D. All of the above E. None of the above 25. The drug represented on fig. 42 is characterized by following: A. It is a vasodilator B. It has antiarrhythmic effect C. Non-dihydropyridine Ca channel blocker D. Block Ca channels in cardiac tissue & vascular smooth muscles E. *All of the above 26. All of the following statements concerning the use of drug on fig, 44 are true EXCEPT: A. Loop-acting diuretic B. Membrane ion transport inhibitor C. Inhibits Na/K/2Cl cotransporter in ascending loop of Henle D. Indicated in edema, heart failure, hypercalcemia E. *Do not increase ototoxicity of aminoglycoside 27. Choose true statements concerning the use of agent on fig. 48 A. Antihypertensive drug B. Adrenergic alpha 2 receptor agonist C. Converted to active form methyl-norepinephrine which activates central alpha2 receptors D. It is effective in pregnancy E. *All of the above 28. Choose true statements concerning the use of drug on fig. 47 A. Antihypertensives B. Angiotensin receptor antagonist C. Blocks AT II receptor in vascular smooth muscles & adrenal cortex D. *All of the above E. None of the above 29. What are indications to application represented on figure 40 drug? A. *Hyperlipidemia B. Arterial hypertension C. Arterial hypotension D. Bradycardia E. All of the above 30. What are contraindications to application represented on figure 40 drug? A. Arterial hypertension B. Gastritis C. Arterial hypotension D. *Pregnancy E. All of the above 31. What are side effects caused by represented on figure 40 drug? A. Liver failure B. Myopathy C. Contraindicated in pregnancy D. Contraindicated in nursing mothers E. *All of the above 32. Specify maximal day's dose of the preparation represented on figure 40: A. 10 mg B. 40 mg C. 100 mg D. *40-80 mg E. 5 mg 33. The drug, represented on figure 40, belongs to: A. Anesthetics B. Antiarrhithmic Drugs C. *Antihyperlipidemic Drugs D. Diuretics E. Antiviral Drugs 34. What are indications to application represented on figure 41 drug? A. Arterial hypotension B. *Arterial hypertension C. Tachyarrythmia D. Hyperlipidemia E. Asthma 35. What are contraindications to application represented on figure 41 drug? A. Constipation B. Dry cough C. Osteoarthritis D. *Hypersensitivity E. Diarrhea 36. What are side effects caused by represented on figure 41 drug? A. *Dizziness B. Liver failure C. Myopathy D. Contraindicated in pregnancy E. Contraindicated in nursing mothers 37. Specify maximal day's dose of the preparation represented on figure 41: A. 5 mg B. *10 mg C. 15 mg D. 20 mg E. 25 mg 38. The drug, represented on figure 41, belongs to: A. Diuretics B. Beta-blockers C. ACE inhibitors D. *Ca++ Channel blockers E. Antihyperlipidemic Drugs 39. What are indications to application represented on figure 42 drug? A. Arterial hypotension B. *Angina C. Hyperlipidemia D. Migrane E. E. Hypertermi 40. What are contraindications to application represented on figure 42 drug? A. Arterial hypertension B. *Cardiogenic shock C. Osteoarthritis D. Angina E. Hepatitis 41. What are side effects caused by represented on figure 42 drug? A. Vertigo B. Headache C. Fatigue D. Hypotension E. *All of the above 42. The drug, represented on figure 42, belongs to: A. beta Blockers B. Diuretics C. *Ca++ Channel blockers D. ACE inhibitors E. Antihyperlipidemic Drugs 43. Specify maximal day's dose of the preparation represented on figure 42: A. 60 mg B. 180 mg C. 240 mg D. *360 mg E. 420 mg 44. What are indications to application represented on figure 43 drug? A. *Tachyarrythmia B. Arterial hypotension C. Hyperlipidemia D. Raynaud’s disease E. Asthma 45. What are contraindications to application represented on figure 43 drug? A. Arterial hypertension B. Osteoarthritis C. Angina D. Hepatitis E. *Second-degree AV nodal block 46. The drug, represented on figure 43, belongs to: A. *beta Blockers B. Diuretics C. Ca++ Channel blockers D. ACE inhibitors E. Antihyperlipidemic Drugs 47. What are side effects caused by represented on figure 43 drug? A. Insomnia B. Sexual dysfunction C. Fatigue D. Hypotension E. *All of the above 48. Specify maximal day's dose of the preparation represented on figure 43: A. 80 mg B. 160 mg C. 100-200 mg D. *320-480 mg E. 400 mg 49. What are indications to application represented on figure 44 drug? A. Tachyarrythmia B. *Congestive heart failure C. Hyperlipidemia D. Angina E. Asthma 50. What are contraindications to application represented on figure 44 drug? A. Arterial hypertension B. *Acute nephritis C. Angina D. Gastritis E. Diabetes 51. What are side effects caused by represented on figure 44 drug? A. *Ototoxicity B. Sexual dysfunction C. Fatigue D. Hypertension E. Headache 52. Specify maximal single dose of the preparation represented on figure 44: A. 0.04 g B. 0.08 g C. *0.16 g D. 1-1.5 g E. 2.0 g 53. The drug, represented on figure 44, belongs to: A. ? Blockers B. Ca++ Channel blockers C. ACE inhibitors D. *Diuretics E. Antihyperlipidemic Drugs 54. The drug, represented on figure 44, belongs to: A. Carbonic anhydrase inhibitors B. *Loop diuretics C. Thiazide diuretics D. Potassium-sparing diuretics E. Osmotic diuretics 55. What are indications to application represented on figure 45 drug? A. *Arterial hypertension B. Tachyarrythmia C. Diabetes mellitus D. Hyperlipidemia E. Angina 56. What are contraindications to application represented on figure 45 drug? A. Arterial hypertension B. Nephritis C. Angina D. *Diabetes mellitus decompensation E. Tachyarrythmia 57. What are side effects caused by represented on figure 45 drug? A. Ototoxicity B. *Nausea C. Osteopenia D. Hypertension E. Headache 58. Specify maximal day dose of the preparation represented on figure 45: A. 5 mg B. *10 mg C. 15 mg D. 2.5 mg E. 20 mg 59. The drug, represented on figure 45, belongs to: A. *Diuretics B. Ca++ Channel blockers C. ACE inhibitors D. ? Blockers E. Antihyperlipidemic Drugs 60. What are indications to application represented on figure 46 drug? A. *Arterial hypertension B. Arterial hypotension C. Hyperlipidemia D. Aortal stenosis E. Hypertension in pregnancy 61. What are contraindications to application represented on figure 46 drug? A. Arterial hypertension B. Diabetes mellitus C. *Hyperkalemia D. Tachyarrythmia E. Myocardial infarction 62. What are side effects caused by represented on figure 46 drug? A. Dry cough B. Hyperkalemia C. Skin rashis D. Hypotension E. *All of the above 63. Specify maximal day dose of the preparation represented on figure 46: A. 10 mg B. *80 mg C. 30 mg D. 40 mg E. 50 mg 64. The drug, represented on figure 46, belongs to: A. Diuretics B. Ca++ Channel blockers C. ? Blockers D. Angiotensin II antagonists E. *ACE inhibitors 65. What are indications to application represented on figure 47 drug? A. Arterial hypotension B. Hyperlipidemia C. Arrhythmia D. *Arterial hypertension E. Cardiogenic shock 66. What are contraindications to application represented on figure 47 drug? A. Arterial hypertension B. Heart failure C. Tachyarrythmia D. Myocardial infarction E. *Pregnancy 67. What are side effects caused by represented on figure 47 medicine? A. *Vertigo B. Constipation C. Cough D. Diarrhea E. Insomnia 68. Specify maximal day dose of the preparation represented on figure 47: A. 0.025 g B. 0.05 g C. *0.1 g D. 0.15 g E. 0.2 g 69. The drug, represented on figure 47, belongs to: A. Diuretics B. Ca++ Channel blockers C. ? Blockers D. *Angiotensin II antagonists E. ACE inhibitors 70. What are indications to application represented on figure 48 drug? A. *Arterial hypertension B. Arrhythmia C. Arterial hypotension D. Hyperlipidemia E. Cardiogenic shock 71. What are contraindications to application represented on figure 48 drug? A. Arterial hypertension B. *Coronary and cerebral atherosclerosis C. Tachyarrythmia D. Pregnancy E. None of the above 72. What are side effects caused by represented on figure 48 medicine? A. Cough B. Hypertension C. Constipation D. Insomnia E. *Sedation and drowsiness 73. Specify maximal day dose of the preparation represented on figure 48: A. 0.5 g B. 0.75 g C. 1.0 g D. *2.0 g E. 3.0 g 74. The drug, represented on figure 48, belongs to: A. *Centrally-acting adrenergic drugs B. Ca++ Channel blockers C. ? Blockers D. Angiotensin II antagonists E. ACE inhibitors 75. What are indications to application represented on figure 49 drug? A. Arterial hypertension B. *Drug of choice for shock C. Arrhythmia D. Atherosclerosis E. Angina pectoris 76. The drug, represented on figure 49, belongs to: A. Centrally-acting adrenergic drugs B. Ca++ Channel blockers C. Blockers D. ACE inhibitors E. *Direct-acting adrenergic agonists