Chapter 6 – Bones and Skeletal Tissues Cartilage Skeletal
advertisement

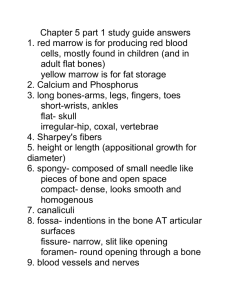
Chapter 6 – Bones and Skeletal Tissues I. Cartilage A. Skeletal Cartilages 1. Embryonic skeleton initially made up of cartilage & fibrous membranes, then gradually replaced by bone. 2. Skeletal cartilage consists primarily of water; makes it resilient (able to go back to its original shape after being compressed) 3. NO nerves or blood vessels; surrounded by dense layer of connective tissue called perichondrium (around the cartilage), which resists outward expansion of cartilage when it’s compressed. 4. Perichondrium contains blood vessels; nutrients diffuse through matrix to the chondrocytes (mature cartilage cells); limits thickness of cartilage. 5. Cartilage consists of chondroblasts (actively dividing form of cartilage cells), chondrocytes (mature form of cartilage) encased in small cavities called lacunae, and an extracellular matrix consisting of a jellylike ground substance and fibers. 6. Three types of cartilage: hyaline, elastic and fibrocartilage. B. Hyaline Cartilages 1. Resembles frosted glass; provides support with flexibility & resilience. 2. Microscopically – spherical shaped chondrocytes in matrix containing fine collagen fibers. 3. Skeletal Hyaline Cartilage – articular cartilages covering ends of most bones at movable joints, nasal cartilage supports external nose, costal cartilages connect ribs to sternum/breastbone, respiratory cartilages form the larynx/voice box and reinforce the trachea, bronchi & bronchioles C. Elastic Cartilages 1. Resembles hyaline cartilage, but contains more elastic fibers making it more flexible. 2. Pinna (external ear) & epiglottis (flap that covers the larynx/trachea when we swallow). D. Fibrocartilages 1. Highly compressible with great tensile (tension) strength; found in areas subject to heavy pressure and stretch. 2. Microscopically – parallel rows of chondrocytes alternating with thick collagen fibers. 3. Menisci/pad-like cartilages of knee, discs between spinal vertebrae. E. Growth of Cartilage 1. Appositional Growth (growth from outside) – cartilage-forming cells (chondroblasts) in perichondrium secrete new matrix against external face of existing cartilage tissue. 2. Interstitial Growth (growth from inside) – chondrocytes in lacunae of cartilage divide and secrete new matrix, expanding cartilage from within. 3. Cartilage stops growing during adolescence, which is when the skeleton stops growing. II. Classification of Bones A. General Information 1. Adult human skeleton – 206 bones 2. Infant skeleton – 300 3. Axial vs. Appendicular Skeleton a. Axial Skeleton (long axis of the body) – Involved in protecting, supporting, or carrying other body parts. **Skull, vertebral/spinal column, & rib cage b. Appendicular Skeleton – enables us to move from place to place & manipulate our environment. ** Arms, legs (upper & lower limbs) ** Shoulder & hip bones (pectoral & pelvic girdles) B. Bone Types – long, short, flat, irregular 1. Long Bones – longer than they are wide, with a shaft & 2 ends. All limb bones (arms/legs) except patella (kneecap), carpals (wrist bones) & tarsals (ankle bones). 2. Short Bones – roughly cube shaped. Carpals (wrist bones) & tarsals (ankle bones). 3. Sesamoid Bones – shaped like a sesame seed; special type of short bone that forms within a tendon. Ex: patella 4. Flat Bones – thin, flattened, usually a bit curved. Sternum (breastbone), scapulae (shoulder blades), ribs, & most skull bones. 5. Irregular Bones – Shapes other than those mentioned above. Vertebrae & hip bones (pelvic area). III. Function of Bones A. Support – framework that supports body & cradles soft organs. Ex: rib cage supports thoracic wall; lower limbs support trunk of body. B. Protection – fused skull bones protect brain; vertebrae protect spinal cord; ribs protect vital organs of thorax. C. Mineral Storage – reservoir for minerals such as calcium & phosphate; released as ions into bloodstream as needed. D. Blood Cell Formation – blood cell formation (hematopoiesis) occurs in marrow cavities of bones such as the femur, hip bones & sternum. IV. Bone Structure – Remember, bones are organs; composed of osseous/bone tissue, nervous tissue, cartilage, fibrous connective tissue lines the bone cavities, muscle & epithelial tissue form the blood vessels within bones. A. Compact & Spongy Bone 1. Compact Bone – appears smooth & solid to naked eye; dense layer of outer bone. 2. Spongy Bone – located below or internal to compact bone. Has a honeycomb appearance due to trabeculae (little beams). Open spaces between trabeculae contain yellow or red bone marrow. B. Structure of Typical Long Bone 1. Diaphysis – tubular in shape, forms shaft or long axis of the bone. Contains a medullary cavity or marrow cavity. In adults, medullary cavity contains fat (aka: yellow marrow). 2. Epiphyses – ends of the bone. Exterior composed of compact bone & interior contains spongy bone. Joint areas of epiphyses are covered with thin layer of articular hyaline cartilage, for cushioning during movement & absorbing stress. Adult long bones have an epiphyseal line, remnant of epiphyseal plate of hyaline cartilage that grows during childhood to lengthen bone. If badly injured during childhood, can affect normal bone growth. 3. Membranes – external surface (except joint surface) is covered by a white double-layered membrane called the periosteum (peri=around, osteo=bone). Outer fibrous layer is dense connective tissue; inner osteogenic layer next to bone surface contains osteoblasts (bone forming cells) & osteoclasts (bone destroying cells). Periosteum contains nerve fibers, lymphatic vessels, & blood vessels which enter the bone through the nutrient foramen (foramen=opening). Sharpey’s fibers composed of collagen secures periosteum to bone matrix. Endosteum, connective tissue membrane, lines inner bone surface & contains osteoblasts & osteoclasts. Anatomy of the Human Humerus Anatomy of a Long Bone C. Structure of Short, Irregular, and Flat Bones 1. Consist of thin plates of periosteum-covered compact bone on outside & endosteum-covered spongy bone inside. Do NOT have a shaft or epiphyses. Have trabeculae which contains bone marrow, but NO marrow cavity. 2. In flat bones, internal spongy bone is called diploe. D. Hematopoietic Tissue = Red Marrow 1. Red marrow – typically located within cavities of spongy bone of long bones & in the diploe of flat bones. Cavities referred to as red marrow cavities. 2. Newborn infants – medullary cavity and all spongy bone contain red bone marrow. 3. Adult long bones – medullary cavity contains yellow marrow (fat) & little red marrow in spongy bone cavities. Blood cell production occurs in head of femur & humerus. Diploe of flat bones such as the sternum & irregular bones like the hip are more active in hematopoiesis. These 2 areas are used for obtaining red marrow for bone marrow transplants. Yellow marrow in medullary cavity can revert to red marrow if person is anemic. V. Microscopic Structure of Bone A. Compact Bone – Identify each labeled structure. Figure a – Identification & Description of Each Labeled Part 1. Periosteum 2. Periosteal Blood Vessel 3. Sharpey’s/Perforating Fibers 4. Compact bone 5. Endosteum – 6. Volkmann’s/Perforating Canal 7. Haversian Canal - 8. Osteon/Haversian System 9. Circumferential Lamellae 10. Lamellae 11. Spongy Bone 12. Medullary Cavity - B. Spongy Bone 1. Consists of many trabeculae, which are aligned along lines of stress, making it good for support. 2. Trabeculae are a few cell layers thick and contain irregularly arranged lamellae & osteocytes interconnected by canaliculi. NO osteons. 3. Osteocytes receive nutrients via diffusion from capillaries in endosteum through canaliculi. VI. Chemical Composition of Bone A. Organic Components of Bone 1. Osteoblasts – mitotically active cells that form bone 2. Osteocytes – mature bone cells. 3. Osteoclasts – large cells that break down or resorb bone matrix. 4. Osteoid – organic part of bone matrix; composed of ground substance (proteoglycans & glycoproteins) & collagen fibers; secreted by osteoblasts. Contributes to bone strength, flexibility & allows bone to resist stretching & twisting. B. Inorganic Components of Bone 1. Hydroxyapatites – inorganic mineral salts, mainly calcium phosphates, make up 65% (by mass) of bone. 2. The calcium salts form tiny crystals which surround the collagen fibers in extracellular matrix; gives bone its hardness & allows it to resist compression. 3. Centuries old skeletal remains can tell scientists about the person’s race, size, sex, the work they did & the diseases they had (arthritis, cancer, osteoporosis). (Covered in quiz #1) VII. Bone Markings – refer to Table 5.1 (same as table 6.1 in text but with illustrations) VIII. Bone Development = osteogenesis/ossification (synonyms for bone tissue formation) – start here A. Introduction 1. Os = bone Genesis = beginning 2. Formation of boney skeleton in embryos. Ossification continues into early adulthood, enabling us to increase in height as bone length increases. Ossification of adult bones functions mainly for remodeling & repair. 3. Thickness of bone can increase throughout our lifetime, which is why weightbearing exercise is so important. 4. Prior to 8th week of gestation, embryo’s skeleton is made of fibrous membranes & hyaline cartilage. After that time, osteogenesis begins & replaces most of the fibrous membranes & cartilage. 5. Intramembranous ossification occurs when bone develops from the fibrous membranes, forming membrane bone. 6. Endochondral ossification occurs when hyaline cartilage is replaced by bone, forming endochondral/cartilage bone. NOTE: Endo=within, Chondro=cartilage B. Intramembranous Ossification–forms most skull bones & clavicles (collar bones); begins around 8th week of development. check out this site http://www.sophia.org/tutorials/bone-development-intramembranous-ossification C. Endochondral Ossification – forms all bones except skull & clavicles. Begins second month of development; more complex than intramembranous ossification because hyaline cartilage must be broken down. Uses hyaline cartilage “bones” as model or pattern for constructing new bone. check out this site http://www.sophia.org/tutorials/bone-development-endochondral-ossification C. Hormones Involved in Bone Growth During Youth 1. Growth Hormone – released by anterior pituitary; stimulates epiphyseal plate activity, especially in infancy & childhood. 2. Thyroid Hormones (T3 & T4) – regulate activity of growth hormone, making sure skeleton grows in proper proportions. 3. Estrogen & Testosterone (sex hormones) – produced in increased amounts during puberty; induce epiphyseal plate closure in long bones (longitudinal bone growth ends – height ceases to increase). IX. Bone Remodeling – bone deposit & resorption occur at periosteal & endosteal surfaces. A. Bone Deposit – involves osteoblasts & osteocytes 1. Occurs when bone is injured or when additional bone strength is needed. 2. Requires healthy diet rich in proteins, Vit. C for collagen synthesis, Vit. D for absorption of dietary calcium, Vit. A for balance between deposition & removal of bone, minerals such as calcium, phosphorus, magnesium, & manganese. 3. Alkaline phosphatase enzyme, produced by osteoblasts, allows mineralization of bone to occur. B. Bone Resorption – involves osteoclasts 1. Osteoclasts can break down bone matrix. 2. Osteoclasts also phagocytize demineralized bone matrix & dead osteocytes. C. Control of Bone Remodeling – hormonal & mechanical mechanisms 1. Hormonal Mechanism – negative feedback loop (2 diagrams) 2. Mechanical Mechanisms – muscle pull and gravity Muscle pull & gravity both promote skeletal remodeling, keeping bones strong where stress occurs. Wolff’s Law states that bone grows or remodels in response to forces or demands placed on it. X. Bone Fractures & Repair A. General Information 1. Youth Fractures – due to trauma that twists or smashes bone; sports injuries, auto accidents, falls. 2. Adult Fractures - same as youth; as we age, bones become thin & weak & fracture more easily. 3. Classification of Fractures a. Nondisplaced Fractures – bone ends retain their normal position. b. Displaced Fractures – bone ends are out of normal alignment. c. Complete Fracture – bone is broken through. d. Incomplete Fracture – bone is not completely broken through. e. Linear Fracture – occurs parallel to long axis of bone. f. Transverse Fracture – occurs perpendicular to long axis of bone. g. Compound Fracture (aka: open) – bone penetrates through the skin. h. Closed Fracture (aka: simple) – bone does not penetrate through the skin. 4. Fracture Treatment = Reduction – the realignment of broken bone ends. a. Closed Reduction – physician repositions broken bone ends using his/her hands. b. Open Reduction – broken bone ends are surgically put back together using pins, wires, screws, etc. NOTE: After reduction, broken bone is immobilized with a cast or traction. Simple fractures require 6 – 8 weeks to heal; much longer for weight-bearing bones & bones of the elderly (they have poor circulation). B. Fracture Types C. Fracture Repair – Beneath the diagram (in your own words), write an explanation of what is happening. XI. Homeostatic Imbalances of Bone = Bone Disorders A. Osteomalacia (“soft bones”) – inadequate mineralization of bones; caused by vitamin D and/or calcium deficiency in diet. Osteoid is produced, but calcium salts aren’t deposited, resulting in soft, weak bones. Person experiences pain when weight is put on affected bones. Treatment: Drinking vitamin D-fortified milk & exposing skin to sunlight. B. Rickets - inadequate mineralization of bones in children. Because young bones undergo rapid growth, bowed legs, deformities of the pelvis, skull & rib cage are common. Treatment: Drinking vitamin D-fortified milk & exposing skin to sunlight. C. Osteoporosis – group of diseases where bone resorption occurs faster than bone deposit. Bone matrix remains normal, but bone mass is reduced and bones become more porous & lighter. Entire skeleton is affected, but spine is most vulnerable & subject to compression fractures. Neck of femur susceptible to fracture leading to broken hips in elderly. Cessation of sex hormone synthesis in both sexes promotes the disease. Estrogen & testosterone help maintain normal bone density by restraining osteoclast activity & promoting deposition of new bone. Other factors include insufficient exercise to stress bones, not enough calcium & protein in diet, abnormal vitamin D receptors, smoking (reduces estrogen levels) & hormone-related conditions such as diabetes & hyperthyroidism. Immobility also contributes to osteoporosis. Treatment: Calcium & vitamin D supplements, increased weight-bearing exercise, hormone replacement therapy (estrogen). Also Fosamax (suppresses osteoclast activity & may reverse osteoporosis in spine) & Evista (works like estrogen but doesn’t increase risk of uterine or breast cancer). D. Paget’s Disease – excessive bone formation & breakdown leads to spotty weakening of the bones. Spine, pelvis, femur and skull most often involved; become deformed & painful. Rare before age 40 & affects about 3% of North America’s elderly population. Cause unknown, but virus may be involved. Treatment: calcitonin & Fosamax, which prevent bone breakdown.