INTERNAL MEDICINE SYLLABUS - Clinical Departments

INTERNAL MEDICINE SYLLABUS
THIRD YEAR MEDICINE SELECTIVES
Jeremy Richards, M.D., Associate Clerkship Director
Deborah DeWaay, M.D., Associate Vice Chair for Medical Education
Mary Ann Snell, Student Education Coordinator
Medical University of South Carolina
Charleston, South Carolina
2015 - 2016
JUNIOR SELECTIVES
OVERVIEW
This month is, in essence, three weeks of core medicine. You will experience the daily work schedule of the subspecialty division to which you are assigned. This will include consultations, clinics, and conferences.
GOALS
1.
Learn and practice the personal and professional characteristics of a superb physician.
2.
Learn the core concepts and clinical skills of Internal Medicine specific to each selective course.
3.
Have fun.
OBJECTIVES
1.
Patient Care a.
Demonstrate proper techniques for interviewing a patient to obtain a medical history and performing a physical examination. b.
Demonstrate analysis, synthesis, and integration of pertinent patient data. c.
Formulate a comprehensive, ordered differential diagnosis. d.
Demonstrate an ability to build a positive, healing relationship with a patient.
2.
Professionalism a.
Demonstrate professional demeanor and ethical behavior.
3.
Medical Knowledge a.
Apply knowledge of the pathophysiology, epidemiology, and natural history of diseases to the diagnosis and management of common patient conditions in Internal Medicine.
4.
Interpersonal Skills and Communication a.
Present patient data gathered from patient interviews, physical examinations, and laboratory sources, including progress notes on patients, in standardized format. b.
Document patient data gathered from patient interviews, physical examinations, and laboratory sources, including progress notes on patients, in standardized format. c.
Demonstrate effective and professional interpersonal and communication skills in interactions with patients and families, including an awareness of psychosocial factors related to patients’ problems.
5.
Practice Based Learning and Improvement a.
Use evidence based medicine to determine patient care decisions. b.
Identify errors in patient care and knowledge deficits. Change future practices based on past mistakes. c.
Use information technology successfully to access and manage patient information.
6.
Systems Based Practice a.
Demonstrate appreciation and collaboration with other members of the health care team including nursing, social workers, care managers, pharmacy etc as applicable to the specific course. b.
Identify issues related to the cost-effectiveness of diagnostic evaluations and patient care.
Allergy &
Immunology Selective
OBJECTIVES OF SPECIFIC SELECTIVES
LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Explain how to diagnosis and treat allergic and non-allergic rhinitis, asthma, atopic dermatitis, urticarial, and chronic sinusitis (MK, PC)
2. Define indications for skin testing and immunotherapy (MK, PC)
2
Hepatology
3. Demonstrate appropriate history and physical exam techniques for this patient population (MK, PC)
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Reading an allergy/immunology review provided during the rotation
2. Direct observation by faculty during direct patient care and review of other clinical and didactic activities (history and physical, progress notes, prescriptions, etc.
3. Ungraded quiz at the end of the rotation that Dr. Ramey will review with the student to help them evaluate knowledge.
PATIENT ENCOUNTERS: Students will be expected to work-up patients with these specified conditions:
1. Allergic and non-allergic rhinitis
2. Asthma/COPD
3. Atopic dermatitis/Contact dermatitis/Urticaria
4. Recurrent infections
5. Food allergy
LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Demonstrate proficiency in assessing patients with liver disease and understanding the components of the history and physical exam that are essential for managing these patients. (PC, MK)
2. Understand the pathophysiology and management of complications that result from cirrhosis and portal hypertension. (MK)
3. Appreciate the timing of referral for liver transplant evaluation by assessing severity of liver disease and short term prognosis in patients with cirrhosis. (MK, PC)
4. Observe the comprehensive evaluation required of patients undergoing consideration for liver transplantation. (MK, PC)
5. Become familiar with immunosuppressive agents post-transplant. (MK)
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Students will participate in the General Hepatology Clinics. In each clinic, students will be specifically responsible for assessing and formulating a management plan for the patients seen as an Initial Clinic Visit (ICV) in the respective clinics.
2. Students will round with the Liver Attending on the inpatient service & evaluate patients on the consult service.
3. Students will observe outpatient endoscopy, to learn the management of patients with esophageal varices.
4. Students will attend the following Hepatology (and Gastroenterology) didactic conferences: GI Fellows Conference, Liver Biopsy Conference, Liver Imaging and
Tumor Board, and Liver Transplant Selection Committee.
PATIENT ENCOUNTERS: Students will be expected to work-up patients with these specified conditions:
1. Complications of cirrhosis/portal hypertension: ascites, encephalopathy, variceal bleeding, and spontaneous bacterial peritonitis
2. Complications that occur after Liver Transplantation: biliary stricture, rejection,
3
VA Pulmonary
Selective
General Internal Med
Ambulatory
Experience opportunistic infections, and complications of immune suppressing meds.
3. Complications of Alcoholic Liver Disease, including alcoholic hepatitis
4. Chronic Hepatitis C
5. Chronic hepatitis of unclear etiology – namely the evaluation of these patients, including the role of liver biopsy.
LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Demonstrate proper techniques for interviewing a patient, performing a physical examination, analyze, synthesize, and integrate pertinent patient data, and finally the formulation of a comprehensive ordered differential diagnosis in the inpatient setting
(PC).
2. Present and document patient data gathered from patient interviews, physical examinations, and laboratory sources, including progress notes on patients, in standardized format (PC, CS).
3. Perform diagnostic and lab test interpretation skills used in Pulmonary Medicine
(e.g. interpret chest radiographs and pulmonary function tests) and identify issues related to the cost-effectiveness of diagnostic evaluations and patient care (MK, PC,
PBL)
4. Apply knowledge of the pathophysiology, epidemiology, and natural history of diseases to the diagnosis and management of common patient conditions in Pulmonary
Medicine (MK, PC).
5. Demonstrate effective and professional interpersonal and communication skills in interactions with patients, including an awareness of psychosocial factors related to patients’ problems (CS, PR)
INSTRUCTIONAL METHODOLOGIES AND ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Students will participate in the pulmonary consult service, the VAICU and evaluate patients under attending/fellow supervision.
2. Presentation and discussion of patients with the consult attending.
3. Selected reading material on topics pertinent to critical care and pulmonary medicine.
4. Attendance at Pulmonary Clinical Conferences at noon on Thurdays and education sessions as provided.
PATIENT ENCOUNTERS: Students will be expected to work-up patients with these specified conditions:
1. Chronic hypoxic respiratory failure in addition to Acute hypoxic/hypercarbic respiratory failure
2. Chronic Obstructive Lung Disease and Interstitial Lung Disease
3. Pneumothorax
4. Sarcoidosis
5. Solitary Pulmonary Nodule
LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Demonstrate proper techniques for interviewing a patient to obtain a medical history and performing a physical examination in the ambulatory clinical setting. (PK, CS)
2. Formulate a comprehensive, ordered differential diagnosis. (PC)
3. Present and document patient data gathered from patient interviews, physical
4
Subspecialty
Consults/Clinics examinations, and laboratory sources in standardized format. (CS, PC)
4. Apply knowledge of the pathophysiology, epidemiology, and natural history of diseases to the diagnosis and management of common patient conditions in Internal
Medicine. (MK, PC)
5. Identify basic concepts of preventive health care, including patient education, immunization, and appropriate age-specific screening recommendations. (PL, PC)
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Participation in ambulatory clinic activities in a variety of local locations.
2. Participation in patient care as supervised by the attending and residents in clinics, including work up of a minimum of 1 new patient per ½ day clinic session.
PATIENT ENCOUNTERS: Students will be expected to work-up patients with conditions from all organ systems. For example (but not limited to), patients with acute or chronic medical conditions in the following areas:
1. Cardiology: hypertension, atrial fibrillation, hyperlipidemia
2. Endocrinology: diabetes
3. Infectious Disease: upper respiratory infection, pneumonia, cellulitis
4. Nephrology: chronic kidney disease
5. Pulmonary: COPD, asthma
LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Demonstrate proper techniques for interviewing a patient to obtain a medical history and performing a physical examination in the inpatient setting. (PC)
2. Demonstrate analysis, synthesis, and integration of pertinent patient data.(PC)
3. Formulate a comprehensive, ordered differential diagnosis. (MK, PC)
4. Present and document patient data gathered from patient interviews, physical examinations, and laboratory sources, including progress notes on patients, in standardized format. (CS)
5. Apply knowledge of the pathophysiology, epidemiology, and natural history of diseases to the diagnosis and management of common patient conditions in Internal
Medicine. (MK)
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Attendance at in-hospital consult rounds, clinics, and other clinical activities.
2. Participation in patient care as supervised by the attending and residents on the service, including work up of a minimum of 2 new patients and following a minimum of 3 patients on the service each week.
3. Attendance at noon conferences and/or any conference supplied by the division.
PATIENT ENCOUNTERS:
Students will be assigned to one of the following areas of Internal Medicine: cardiology, endocrinology, gastroenterology, general internal medicine, hematology/oncology, infectious disease, nephrology, pulmonary or rheumatology.
The type of patients seen depends upon the division to which they are assigned. They will be in clinic or on consults (or a combination of the two) based upon the area and the specific diseases the students see depends on their assignment.
5
Cardiology Outpatient
Clinic
LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Take a good cardiac history and understand cardiac risk factors. (MK, PC, CS)
2. Perform a complete cardiovascular examination. (PC)
3. Define and analyze EKGs, ECHO and stress testing with supervision to evaluate cardiac disorders. (MK, PC)
4. Get familiar and comfortable with basic cardiac oral medications. (MK)
5. Evaluate cardiac risk factors and modify them appropriately- as per guidelines.
(MK, PC)
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Students will evaluate clinic patients under attending supervision. They will take a detailed history of new patients. Cardiovascular examination skills will be imparted to the students at the bedside. Return visit patients will be followed along with the attending. Any interesting findings or EKGs will be brought to their attention.
2. Students will assist the nurses in obtaining vitals thereby learning how to assess pulse, BP, respiration and temperature.
3. Students will also assist with performing an EKG and in its interpretation on their own patients, accompany and observe Echocardiography and Exercise stress testing on their patients, and learn how to hook up Holter and Event Monitors.
4. Students will attend all morning reports. They will also be expected to attend all cardiology AM conferences during the rotation. After the morning conferences they will report to their clinic.
5. Students will be exposed to the cardiac cath lab on Wed mornings.
PATIENT ENCOUNTERS: Students will be expected to work-up patients with these specified conditions:
1. Coronary artery disease
2. Congestive heart failure
3. Arrythmia
4. Valvular heart disease
5. Risk Factor Modification (DM, HTN, hyperlipidemia, smoking)
Inpatient Cardiology LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Take a good cardiac history, understand and modify cardiac risk factors, complete cardiovascular system examination and get familiar and comfortable with cardiac medications. (MK, PC, CS)
2. Understand the use of lab tests, EKGs, ECHO, stress testing and cardiac invasive procedures in working up cardiac disorders.(MK)
3. Understand basic cardiac, coronary and electrophysiological anatomy along with basic cardiac hemodynamics and improve EKG interpretation skills. (MK)
4. Present new cases confidently, follow-up cases allotted and learn to work efficiently as a team member. (CS, PC)
5. Develop skills in patient and family interaction. (CS)
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Students will evaluate inpatients under the Attending or Resident/Fellow
6
Electrocardiography
(EKG) supervision.
2. Students will obtain vital signs and also learn how to do and interpret an EKG on their patients.
3. Students will accompany their patients and observe Echocardiography and Exercise stress testing, cardiac catheterization /EP on their patients. They will also learn how to hook up Holter event monitors. They will also review Telemetry records daily and get confident with rhythm assessment.
4. Students will attend morning report and (if time permits) briefly present an interesting inpatient case at the morning report. They will also be expected to attend all cardiology AM conferences during the rotation.
5. They will participate in patient counseling and advise about risk factor modifications. They will participate with assessment of patients other social needs with the social workers and discharge planners.
PATIENT ENCOUNTERS: Students will be expected to work-up patients with these specified conditions:
1. Coronary artery disease
2. Congestive heart failure
3. Arrythmia
4. Valvular heart disease
5. Risk factor modification (DM, HTN, hyperlipidemia, smoking)
LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Position leads and do an EKG. (MK)
2. Appreciate waves and intervals on an EKG. (MK)
3. Appreciate basics rhythms on EKG and have a general idea about treating common rhythm disorders. (MK)
4. Identify ST segment alterations on an EKG and know the differential diagnosis for the abnormality. (MK)
5. Know the basic treatments for ST segment elevation MI (STEMI) and non ST segment elevation MI (NSTEMI). (MK)
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Students will do a few elective EKGs daily with the technician. They will position leads appropriately and do EKGs and troubleshoot the EKG machine. They will also be taught to identify EKG waves and intervals.
2. EKG didactic teaching will be done daily at the VA. They will be advised about self-learning EKG modules.
3. Students will attend all VA morning reports. They will also be expected to attend all cardiology AM conferences during the rotation.
4. They will attend the VA cardiology clinic on Tuesdays (half day) and evaluate patients and their EKGs in an ambulatory setting.
5. They will learn about the basic pharmacology and applications of Adenosine,
Digoxin, beta blockers, calcium channel blockers and Class1-4 Antiarrythmic drugs.
PATIENT ENCOUNTERS: Students will be expected to work-up patients with these specified conditions:
1. Cardiac chest pain
2. Atrial Fibrillation/Atrial Flutter
7
Diabetology
Endocrinology
Neoplasia
3. Other arrhythmias
4. Valvular heart disease
LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Understand basic classification of diabetes: Type 1, Type 2, Latent autoimmune adult onset, gestational, etc. (MK).
2. Take and present diabetes-focused histories and physical exams (PC, CS).
3. Understand pharmacology and use of oral diabetic medicines and insulin (MK).
4. Understand the essentials of intensive insulin therapy, including insulin pump therapy and glycemic monitoring (fingerstick blood sugars, A1c, fructosamine) (MK,
PC).
5. Understand and assess for common diabetes complications: microvascular, macrovascular and hypoglycemia (MK, PC, CS).
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Rotate with Diabetes Management Service (DMS) and assist in assessing patients and participate in DMS rounds.
2. Participate in endocrine attending, IDEAL clinic, including interactions with diabetic educators and dietician.
3. Under attending supervision, participate in private endocrine clinics and assist in the assessment of patients with diabetes
4. Attend endocrine conferences (grand rounds, research conference and Journal club).
5. Students may tailor the consult/clinic ratio to their liking.
PATIENT ENCOUNTERS: Students will be expected to work-up patients with these specified conditions:
1. Type 1 diabetes
2. Type 2 diabetes
3. Inpatient glycemic management
4. Insulin pump therapy
LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Demonstrate understanding of pathophysiology of common neoplastic disorders of the endocrine system (i.e. thyroid cancer, including post-surgical hypothyroidism and hypoparathyroidism and benign thyroid nodules; pituitary tumors and pituitary hypersecretory and deficiency syndromes; hyperparathyroidism; MEN syndromes)
(MK).
2. Take and present endocrine-focused histories and physical exams regarding above disorders with special focus given to learning proficiency in exam of thyroid (PC, CS).
3. Learn and discuss the basics of treatment and prognosis for more common endocrine tumors (MK, PC).
4. Learn the appropriate use and interpretation diagnostic technologies commonly used in the care of patients with endocrine tumors: thyroid ultrasound, thyroid scan and uptake, 131-iodine whole body scans and therapy for thyroid cancer; CT and MRI imaging of adrenals and pituitary; nuclear imaging for pheochromocytoma and other endocrine tumors (MK, PC).
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
8
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Participation in Endocrine Tumor Clinic.
2. Participation in Thyroid Clinic.
3. Observation of thyroid ultrasounds and biopsies.
4. With supervision of inpatient endocrine fellow and attending, students will follow hospitalized patients with endocrine neoplasia as primary consult diagnosis.
5. Attendance at endocrine conferences (grand rounds, research conference and
Journal club).
PATIENT ENCOUNTERS: Students will be expected to work-up patients with these specified conditions:
1. Thyroid cancer, thyroid nodule
2. Hyperparathyroidism
3. Adrenal nodule/cancer
4. Pituitary tumor
5. Thyroid ultrasound/biopsy
Inpatient Hematology LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Demonstrate proper techniques across for interviewing a patient to obtain a hematology-focused medical history and performing a hematology-focused physical examination in the inpatient setting (PC).
2. Demonstrate an understanding, through presentations on daily rounds, of the patient’s primary disease process, how complications relate to causative factors, and how diagnostic test results should be interpreted and applied to the decision-making process (PC, MK).
3. Understand the standard approach for obtaining marrow aspirate/biopsy and peripheral blood smears, assessing their adequacy, and interpreting the specimens, including distinguishing normal from abnormal erythrocytes, leukocytes, and platelets
(MK, PC).
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Participation in the full range of inpatient activities of the MUH Hematology
Service.
2. The student will (A) perform admission work-ups of new patients assigned by supervising physicians; (B) continue to evaluate assigned patients (through follow-on histories and physicals on a daily basis (or more often as appropriate) plus reviewing all diagnostic testing results); (C) present his findings and interpretations on rounds;
(D) perform all appropriate clinical documentation including admission H&P forms, daily progress notes in standard SOAP format, and orders and test requisition forms
(for co-signature by a supervising physician in accordance with hospital policy); and
(E) perform necessary procedures suitable for his level of skill such as marrow aspiration/biopsy and lumbar puncture (LP) as proctored by supervising physicians within hospital policy limits (e.g., a student may perform an LP, but only a hem/onc fellow or attending may administer intrathecal chemotherapy).
3. The student also will participate in all of the division’s standing educational conferences.
PATIENT ENCOUNTERS: Students will be expected to work-up patients with these
9
Heme/Coagulation
Disorders
Nephrology
Consultation specified conditions:
1. The student will carry at least 2 Hematology Service inpatients at all times during the selective.
2. No more than 1 new patient (admission) work-up per day will be required of the student.
(a) Leukemia patients: acute lymphoblastic, acute myelogenous, (b) Bone marrow transplant patients, (c) Lymphoma
LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Understand, discuss, diagnose, and treat common congenital and acquired bleeding disorders; common thrombotic disorders including VTE and arterial thrombosis (MK,
PC).
2. Provide safe and effective anti-thrombotic therapy using heparin, low molecular weight heparin, warfarin, dabigatran, direct thrombin inhibitors, and novel oral anticoagulants (MK, PC)
3. Use peripheral blood smears and clinical lab tests to diagnose common disorders of red blood cells, platelets, & white blood cells (MK, PC)
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Attend 2 half-day clinics and complete outpatient evaluation of one new patient and one follow-up patient in each clinic.
2. Attend afternoon rounds with Coagulation Consult Service. Perform at least 3 new consult evaluations per week and 5 follow-up evaluations of patients referred to this service.
3. Attend weekly coagulation consult service. Complete one case presentation and evidence-based approach to diagnosis and treatment of a patient case seen every two weeks.
4. Attend monthly coagulation/pharmacy rounds.
5. Review peripheral blood smears during the consult service rounds in the heme lab or with hematopathology.
PATIENT ENCOUNTERS: Students will be expected to work-up patients with these specified conditions:
1. 2 new and 2 return outpatient evaluations each week
2. 3 new inpatient evaluations per week
3. 5 follow-up evaluations of inpatient consults per week
4. Congenital & acquired bleeding disorders, VTE, and arterial thrombosis
LEARNING GOALS & OBJECTIVES: At the completion of this clinical rotation students should be able to do the following:
1. Complete an evaluation for Acute Kidney Injury, interpret lab, radiological studies,
& synthesize a differential diagnosis. (MK, PC)
2. Learn & understand the steps involved in urine microscopy & interpretation of urine microscopy in patients with AKI. (MK)
3. Understand the indications for dialysis therapy and the mechanics of different modes of dialysis. (MK)
4. Evaluate and treat hypo/hypernatremia, hypo/hyperkalemia, acidosis and alkalosis.
(MK, PC)
5. Understand the treatment and public health significance of Chronic Kidney Disease
10
and Hypertension. (MK, PC, PL)
6. Learn the correct technique of urine analysis and understand its clinical importance.
(MK, PC)
INSTRUCTIONAL METHODOLOGIES & ROTATION ACTIVITIES:
Students on this rotation will be expected to learn and achieve the educational goals and objectives through the following methodologies and activities:
1. Students will evaluate patients both in hospital and in clinic and present patients orally to the attending physician to attain feedback on presenting cohesively and on ability to synthesize information and provide a well thought out plan.
2. Students will be expected to continue independent scholarly activity by reading journal articles and textbooks pertinent to their specific patients.
3. The nephrology faculty and fellows on service will be actively involved in team based teaching during the rounds.
4. The faculty and fellows on service dedicate time outside patient care activities to provide didactic sessions involving but not restricted to AKI, electrolyte and acid base problems and dialysis.
PATIENT ENCOUNTERS: Students will be expected to work-up patients with these specified conditions:
1. Acute Kidney Injury
2. Acute Glomerulonephritis
3. Electrolyte Disorders – hyponatremia, hypernatremia, hyperkalemia
4. Proteinuria and microscopic hematuria
5. Acid Base Disturbances
6. End stage renal disease – management of medical problems associated with ESRD
ACTIVITIES
STUDENT RESPONSIBILITIES
1.
All Internal Medicine courses adhere to the “Medical Student Supervision and Teaching Policy” approved by the MUSC COM UCC on June 15, 2012.
2.
Students are allowed to see and perform non-invasive exams on patients that have been assigned to them by their attendings or residents unsupervised. For invasive exams (breast, genital, rectal), a resident or attending physician must be present.
3.
Students are allowed to participate in ANY procedure that is common to internal medicine with approval and supervision by the certified healthcare provider (this includes but is not limited to: the nurse, respiratory therapist, resident or attending physician) performing that procedure. This includes but is not limited to IV or central line placement, ABGs, lumbar punctures, arthrocentesis, thoracentesis, or paracentesis.
4.
You may use EPIC in the outpatient and consult setting . For instructions on how to use EPIC go to
“EPIC instructions” on clerkship website.
5.
Please see course specific instructions for a further delineation of expectations.
11
EPIC INSTRUCTIONS
Instructions for EPIC can be found on the Internal Medicine Student Website at the following link: http://clinicaldepartments.musc.edu/medicine/education/medstudents/EPIC
ACTIVITIES
Your exact schedule, including attending rounds, will be at the discretion of the division to which you have been assigned.
The Department of Medicine has a full schedule of conferences, which you are strongly encouraged to attend, in addition to any assigned clinics and conferences mandated by your division.
OTHER ACTIVITIES
**** Please note: You are required to do SIMPLE cases in their entirety. The course coordinator will periodically audit all online cases. If an insufficient amount of time is being put into your cases you will be asked to repeat the cases not completed appropriately and your grade in this course will
be marked incomplete until they are completed. Please complete 10 of the 16 the assigned cases.
SIMPLE CASES
1) Objectives for each case are embedded into the cases online. We will not list them here because it will diminish the benefits of these cases if you are aware of the diagnoses in advance.
2) Instructions: a.
To log in go to: http://www.med-u.org
b.
For first time users: i.
Click on “Login to Cases” up in the right margin ii.
Choose First time user c.
Complete all the questions d.
Click the “Accept” button e.
Click “Send”
3) For returning users: a.
Just login using the account you have already created on another rotation. b.
Follow directions given on site.
4) You must complete 10 out of 16 of the following cases a.
Case1: Mr. Monson b.
Case 2: Ms. Johnston c.
Case 3. Mrs. Koda d.
Case 4: Mrs. Rivers e.
Case 12: Mr. Wilson f.
Case 17: Mr. Moeller g.
Case 18: Mr. Caldwell h.
Case 20: Ms. Hunt i.
Case 21: Mr. Ramirez j.
Case 24: Mrs. Cole
12
k.
Case 25: Mrs. Kohn l.
Case 26: Mr. Johnson m.
Case 28: Mr. Honig n.
Case 30 Ms. Bond o.
Case 33: Mrs. Baxter p.
Case 34: Mr. Farber
INTERPROFESSIONAL ACTIVITY:
There is no formal, prearranged interprofessional activity for these courses. However, you will be exposed to case managers, PharmDs, PT, OT and many other types of medical professionals. Feel free to create your own activity that would satisfy your requirement. Activities need to be logged in E-value.
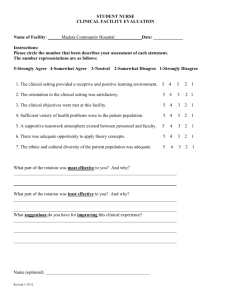
GRADING POLICY
FEEDBACK:
1.
Midpoint cards: you will be given 2 of these cards to be completed by 1 attending and 1 resident or 2 attending physicians. These should be completed and turned in mid-week 2 of the rotation.
EVALUATION:
1.
Medicine Selectives are graded on a Pass-Fail basis. Your attending physician, the fellow and/or resident assigned to your team will evaluate your clinical performance.
2.
Criteria for Passing: a.
Clinical Evaluations: must obtain a minimum average of 9
“Frequently” marks.
3.
Criteria for Failing: A student will FAIL the clerkship or selective if any one of the following conditions is met: A Clinical Performance Evaluation average grade of 40 out of 64 or less
(GPA of 2.5 or lower) , or at the discretion of the course director if the following occurs, one (1) or more ratings of “rarely, if ever”, or four (4) or more ratings of “inconsistently”. Additionally, a student is eligible for failure at the discretion of the Clerkship Director for unprofessional behavior.
4.
In order to receive a grade in the selective courses the SIMPLE cases must be completed. If the student does not complete these cases, their grade will marked “Incomplete” until they do.
5.
Students may ask Dr. Richards (Associate Clerkship Director) to have the Internal Medicine
Education Committee review their grade. If the grade is upheld, the student may appeal their grade to the Clinical Sciences Planning and Evaluation Committee. If the matter is not resolved to the satisfaction of the student and the student continues to feel that a wrong has occurred, the student may petition in writing Dr. Donna Kern and Dr. Debra Hazen-Martin for a final appeal.
We follow the COM Clinical Course Assessment and Grading Policy
“ 3 rd Year Clerkship & Selectives Failure (Approved on May 1 st , 2015)
Each clerkship, selective, and required course, sets criteria for failure, pass, and honors for the course prior to the start of each academic year. These criteria will be made available to students at the beginning of each clerkship/course in written form.
All clinical faculty and rotations will assess the clinical performance of students using the standardized
COM Clinical Performance Evaluation (CPE).
A student will FAIL the clerkship or selective if any one of the following conditions is met:
13
A Clinical Performance Evaluation grade of 2.5 or lower , or at the discretion of the course director if the following occurs, one (1) or more ratings of “rarely, if ever”, or four (4) or more ratings of “inconsistently”.
A written exam grade at a minimum of at least two (2) standard deviations below the national norm for that exam.
A failing grade on any secondary component (of the grade).
Additionally, a student is eligible for failure at the discretion of the Clerkship Director for unprofessional behavior.
What if a student fails some component of the grade?
If a student fails the clinical component of the grade (CPE), the student must repeat the course. The
Medical Student Performance Evaluation (MSPE) and the academic transcript will reflect the failure and repeating of the course.
B. Policy: 3 rd Year Clerkship Honors (Approved on November 18, 2011)
The criteria for the designation of Honors will be determined by each clerkship and approved by the appropriate academic committees. Each clerkship will publish Honors criteria prior to the start of the academic year and will make this information available to students at the beginning of the clerkship in written form. NOTE: Selectives are not eligible for Honors.
”
STUDENT CONDUCT
Students should exhibit professional and ethical behavior at all times. Among other things, this includes appropriate dress, demeanor, attendance, promptness, and appropriate interactions with health care providers.
Code of Conduct
MUSC and the College of Medicine are invested in maintaining an academic and clinical environment in which students, faculty, fellows, residents, nurses and staff can work together freely without threat of mistreatment or bias with regard to their race, color, religion, sex, sexual orientation, national or ethnic origin, age, disability or any other factor irrelevant to participation in the activities of the College.
Students are responsible for reading and understanding the Code of Conduct Policy. https://www.musc.edu/medcenter/policy/stds_of_conduct.pdf
ATTENDENCE
1.
We adhere to the MUSC College of Medicine 3 rd
Year Student Absence Policy. See link on the
IM Student Website Welcome page for details.
2.
No make-up necessary for up to 1 day: death, illness (MD note), wedding (immediate family).
Any other absences, must be made up in a timely manner.
3.
You have a daily commitment to be on work rounds led by the team resident/attending physician.
You must receive prior approval from Dr. Richards and your course director, in order to be absent from rounds. For absences that are requested in advance, an absence form must be filled out and
14
emailed to Mary Ann Snell.
4.
For emergency situations (illness, death in family etc), an email needs to be sent to Dr. Richards
( richarje@musc.edu
) and the coordinator ( snellma@musc.edu
) for any absence. Once that approval has been received it will then be your responsibility to let your team know you will be gone. A student schedule is included in this syllabus. We follow the MUSC College of Medicine
Absence and Away Policy (please see website link for details).
5.
Attendance at all scheduled student activities as delineated by the specific selective is required.
6.
All inpatient ward students work 6 days per week. All outpatient students work 5 days per week.
Dress Code: You are expected to dress professionally. Patients will recognize you as a concerned member of the medical team, and will expect (and deserve) appropriate attire on your part. Attendings and residents reserve the right to comment on the appropriateness of dress. Name tags must be worn at all times.
Policies and Procedures: This clerkship follows all COM and MUSC policies and procedures regarding students. Please contact the Associate Clerkship Director if any are violated so that the situation can be rectified. Links to pertinent policies can be found on our website. If you cannot find a particular policy please contact Mary Ann Snell.
COURSE EVALUATION
In order to continue to improve the Internal Medicine Core Rotation, you will be required to critique the course, the attendings, residents, and fellows with whom you worked. These comments are kept totally anonymous. These evaluations need to be completed no later than the Monday immediately following the rotation .
PROBLEMS
If you have any questions or problems during your rotation, please call the student coordinator at 792-
7282 (807 E CSB). If you have any problems on the service during the rotation, please contact the student coordinator, or Associate Clerkship director. If you would like to meet with the Associate Clerkship director during or after the rotation, you may schedule an appointment by contacting your student coordinator.
Associate Clerkship Director: Jeremy Richards, M.D., richarje@musc.edu
Pager #
Associate Vice Chair for Education: Deborah DeWaay, M.D., dewaay@musc.edu
Pager #14523
MEDICINE SELECTIVE CONTACTS
Most of the time you will meet with the division coordinator immediately following orientation. S/he will answer any questions you might have and may supply you with some additional information. At that time they will put you in touch with your team members.
15
Subspecialty:
Allergy:
Cardiology:
MED 894 J
MED 896 J
MED 897 J
MED 900 J
MED 849 J
MED 894 J
Rheumatology:
MED 894 J
Contact:
EKG
Dr. John Ramey
Glenda Oltmann
Subspecialty C/C/C
Cardiology Clinics
Cardiology Wards
Phone:
843-729-2374
876-4788
Location:
7 th
Fl. ART
Dr. Valerian Fernandes
Dr. Valerian Fernandes
Dr. Valerian Fernandes
Dr. Valerian Fernandes
Endocrinology:
MED 894 J
MED 898 J
MED 899 J
Beth Gunnells
Subspecialty C/C/C
Diabetology
Endocrine Neoplasia
Gastroenterology: Cindy Peeples
MED 858 J
MED 891 J
GI
Hepatology
Subspecialty C/C/C MED 894 J
Hem/Onc: Fatima Frierson
792-4747
Dr. Beatrice Hull
Dr. Beatrice Hull
Dr. Beatrice Hull
Drs. Dantzler, Elias, Koch
Drs. Dantzler, Elias, Koch
Drs. Dantzler, Elias, Koch
792-1298 104 BSB
MED 823J
MED 894 J
MED 901 J
Infectious Disease: Shawn Prioleau
MED 894 J
Heme/Coagulation Disorders Dr. Charles Greenberg
Subspecialty C/C/C Dr. Lindsay Peterson
Hematology Wards Dr. Lindsay Peterson
Subspecialty C/C/C
792-4542 12 th
Dr. Lauren Richey
Fl. RT
Tammy Hill 792-9188 829 CSB Nephrology:
MED 894 J
MED 995 J
Pulmonary:
Subspecialty C/C/C
Nephrology Consults
Kimberly Miller
876-0298 2 nd
Fl Gazes
Dr. Nithan Karakala
Dr. Nithan Karakala
792-7199
816 CSB
812 CSB
VA Pulmonary Selective Dr. Richard Rissmiller
Subpecialty C/C/C Dr. Richard Rissmiller
Terri Hayes
Subspecialty C/C/C
792-3484 912 CSB
Drs. Faye Hant & Diane Kamen
16