APA - People at Creighton University
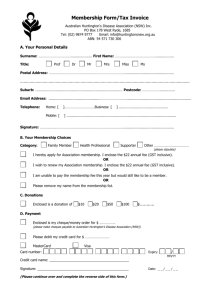
advertisement
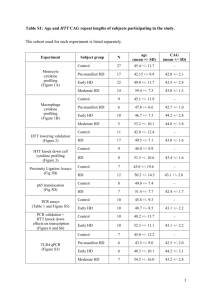
Huntington’s Disease Running head: REVIEW AND PROPOSAL Huntington’s Disease: Past, Present, and Potential Future Analyses Nicholas E. Glass Creighton University 1 Huntington’s Disease 2 Huntington’s Disease: Past, Present, and Potential Future Analyses To date, research efforts have produced substantial information regarding the causes of Huntington’s Disease (HD). But despite this proliferation of knowledge, the subcellular mediators of HD remain its most poorly understood causes. Consequently, our understanding of what leads to HD is still too rudimentary to proffer any kind of curative therapy. And given the devastating nature of HD, this inadequacy in our understanding is, though itself understandable, quite unacceptable. Therefore, this paper will first address the known features of HD. Explanation of the known causes of HD will follow. The paper will then define the HD problem and propose a course of investigation which may help to solve it. The State of the Science Regarding the Disease HD is perhaps most remarkable for the gradual but relentless debilitation and eventual death which it entails. Movement disturbances are usually the first manifestations of HD that carriers recognize (Blumenfeld, 2002). Among these is Huntington’s chorea, the motor hallmark of the disease. Banich (1997) characterizes HD chorea as “a variety of jerky movements that appear to be well coordinated but are performed involuntarily and ceaselessly in an irregular manner” (p. 151). During the early stages of HD, the choreiform movements may affect only parts of limbs, but eventually most of the body, including whole limbs, the head, face, and trunk will become involved and all movement will be uncontrollable (Banich, 1997). HD sufferers also have difficulty initiating and executing movements, especially voluntary eye movements (Banich, 1997; Blumenfeld, 2002). This motor difficulty is known as bradykinesia or akinesia depending on whether the intended movements are slowed or stopped, respectively. At later stages, HD patients become unable even to walk, speak, or swallow (Banich, 1997; Blumenfeld, 2002). The effects of HD are by no means restricted to body movement. With respect to mental processes, HD usually impairs memory first, then personality, mood, affect, and attention, eventually resulting in severe dementia marked by the virtually complete absence of emotional Huntington’s Disease 3 and intellectual functioning (*, *; Cotran, Kumar, & Collins, 1999). The severe memory loss coincident with late-stage HD can be categorized as temporally extensive flat retrograde amnesia, since memories for both the recent and remote past are affected to a similarly profound extent (Banich, 1997). Moreover, depression, anxiety, obsessive-compulsive disorder, impulsive or destructive manic behavior, and even psychosis have been among the psychiatric symptoms brought on by HD (Blumenfeld, 2002). Along with the vicious quality of the impairments inflicted by HD, the disease is also alarming from the standpoint of how many people it impairs. In America alone, HD afflicts approximately 30,000 individuals, with almost twice as many more people carrying the gene asymptomatically, i.e. without yet suffering from HD symptoms (Reiner, Dragatsis, Zeitlin, and Goldowitz, 2003). Of course, many thousands more people around the world also have HD in its latent and manifest forms. Unfortunately, accurate estimates as to the number of HD sufferers and carriers worldwide have been unfeasible for several reasons, the foremost being that data for Africa and Eastern Asia are lacking (Harper, 1992). A second major reason is that the numbers of people affected by HD can fluctuate rapidly and significantly due to global immigration and travel, and to the mode of transmission of HD (Harper, 1992). Nonetheless, the newest data affirm that populations of European descent have an unusually high prevalence of HD (4-8 per 100,000) and that HD frequency is high in India and parts of central Asia but surprisingly low in Finland and Japan (Harper, 1992). A standard estimate of worldwide HD incidence independent of demography is 5 to 10 victims for every 100,000 people (*, *; Li et al., 2003). Other sources propose much lower frequencies, such as 1.6 cases per million (Banich, 1997) or 4 to 5 cases per million (Blumenfeld, 2002). By all accounts, though, HD is a relatively rare condition. Granted the scarcity of HD, epidemiological statistics are negligible consolation to people who have received the veritable death sentence that is a HD diagnosis. No matter how rare the condition may be, it still occurs. And when it does, it amounts to an inexorable loss of control, identity, and life. Not surprisingly, then, patients who grasp this reality are significantly more likely to commit suicide, attempt suicide, or be hospitalized for psychiatric reasons. Factors Huntington’s Disease 4 associated with suicide, suicide attempts, and psychiatric hospitalization include unemployment and a psychiatric history ≤5 years before being diagnosed. Out of all possible factors, though, the strongest impetus for despair seems to be the actual onset of symptoms (Almqvist et al., 1999). With regard to onset of symptoms, the precise age at which this occurs in HD is a matter of moderate disagreement, since certain reports conflict as to when HD symptoms normally appear. The general consensus is that onset is most common in the fourth and fifth decades of life (Cotran et al., 1999). However, Klug and Cummings (2002) state that “symptoms usually appear in the fifth decade of life” (p.624). It is unclear, though, whether they are referring to initial symptoms or the more progressive symptoms. Much less ambiguously, Li et al. (2003) claim the mean age of onset to be 38 years. Importantly, a number of sources point out that HD symptoms can appear at any age (*, *; Glass, Van Dellen, Blakemore, Hannan, & Faull, 2004). Considering all of the aforementioned accounts, the reported age of onset for HD seems to be dropping as time passes. Possible causes for the apparent decrease in reported age of onset include increased awareness and vigilance on the part of medical practitioners dealing with initial HD symptoms. Advances in and greater utilization of, diagnostic technologies such as CT and MRI might have contributed as well. Inconsistency is even more appreciable among reports of life expectancy following diagnosis. According to older literature, the majority of HD victims die within 10 to 15 years after the onset of symptoms (Banich, 1997; Klug & Cummings, 2002). Blumenfeld (2002) similarly puts the median survival after the onset of initial symptoms at 15 years. The most recent literature, however, sets typical life expectancy closer to 20 years (Li et al., 2003; Reiner et al., 2003). Treatment for symptoms (as there is no treatment for the condition per se) may play a marginal role in the apparent increase in reported life expectancy. Additionally, similar to the discrepancy in reported age of onset, the variation in reported life expectancy might be traceable to the attainment of timelier diagnoses. With the HD gene having been identified, the potential for timely and accurate diagnosis is unprecedented. In fact, it is now possible to diagnose a predisposition to HD in utero. (This Huntington’s Disease 5 possibility raises immense concerns about whether people should undergo genetic testing for presently incurable diseases. These concerns, however, are the topic of another paper.) This possibility exists because HD is inherited in an autosomal dominant fashion and has complete penetrance (Blumenfeld, 2002; Sugars & Rubinsztein, 2003). In other words, an individual with the HD mutation will predictably develop HD regardless of (1) his or her sex, (2) the sex of the parent from whom a mutant allele was inherited, and (3) whether one or both inherited alleles are of the mutant form (Klug & Cummings, 2002). The specific autosome on which the gene responsible for HD resides is chromosome 4. More precisely, it was located at 4p16.3 through the use of restriction fragment length polymorphisms (The Huntington’s Disease Collaborative Research Group, 1993). Transmission of HD, while adhering to the classical model of complete autosomal dominance, is not without some idiosyncrasies. Specifically, with respect to HD being autosomally rather than sex chromosomally linked, it is notable that children of fathers bearing the HD mutation are prone to developing symptoms earlier. This susceptibility is due to the phenomenon of genetic anticipation, which will be discussed later (Cotran, Kumar, & Collins, 1999; Klug & Cummings, 2002). Another interesting idiosyncrasy pertains to homozygous individuals, both of whose alleles are of the mutant form and so predispose them to HD. (Such individuals are exceedingly rare in any given population, since they can only be born to two parents who both have the gene for HD.) The expected clinical course of these individuals is the subject of pointed disagreement. Squitieri et al. (2003) demonstrated that once the characteristic HD degeneration began, it was more severe in a sample of eight homozygotes as compared to a group of 75 unrelated heterozygotes. On the other hand, Alonso et al. (2002) observed a single sibling pair consisting of one hetero- and one homozygote. In their study, the age and type of symptoms at onset were the same for both siblings, but the disease had a more severe progression in the heterozygote. If a statistically significant difference between hetero- versus homozygous disease severity can be firmly established, it will have considerable mechanistic implications. Huntington’s Disease 6 Regarding the Mechanisms of the Disease Even when speaking only of what is already verifiably known about the processes that give rise to HD, the means by which HD takes its effects are rather complicated. The nature and number of interacting levels can be daunting. But they are also comprehensible, provided the appropriate systematic inspection. In attempting to guide such an inspection, I will present findings and theories in order of ascending material magnitude. That is, the causes of HD will be presented first at the level of the involved genes, then at the levels of involved proteins, organelles, and, lastly, cells and tissues. Genes The genetic mutation associated with HD is only responsible for the disease insofar as the gene encodes an abnormal form of a protein. The protein in question is known as huntingtin (Htt) and will be discussed at length in the next section. The gene of interest encodes abnormal Htt because of its own abnormality. Specifically, the problematic HD gene contains an excessive number of repeats of the trinucleotide sequence CAG (cytosine-adenine-guanine) (Bolivar, Manley, & Messer, 2003; Squitieri et al. 2003). Normal Htt-encoding genes have fewer CAG repeats along a particular stretch of exon 1—the first segment of DNA expressed in protein form following translation of mRNA (Sugars & Rubinsztein, 2003). There is approximate agreement as to the number of repeats that counts as excessive. The most seminal studies on the topic assert that people with fewer than 35 repeats do not develop HD, while those with 35-39 repeats have a heightened risk of developing the disease, and that people with 40 or more repeats will develop HD within a normal lifetime (Bates, 2003; Huntington’s Disease Collaborative Research Group, 1993). Some later sources truncate this assessment, stipulating that possession of any more than 35 CAG repeats is sufficient for HD (Li et al., 2003; Reiner et al., 2003; Sugars & Rubinsztein, 2003). However long a pathological repeat expansion may be, it is a result of genetic anticipation, as noted previously. Anticipation, in the somewhat peculiar genetic sense, is “the phenomenon of a progressively earlier age of onset and increasing severity of symptoms for a Huntington’s Disease 7 genetic disorder in a successive generation” (Klug & Cummings, 2002, p. A-18). In the particular case of HD, the anticipation stems from erroneous DNA replication during spermatogenesis, the process whereby male gametes are produced (Cotran et al., 1999). This conclusion can be made because HD-positive sons sometimes have twice or three times as many CAG repeats as their HD-positive fathers, while other HD-positive sons exhibit a CAG complement very similar to, if not congruent with, that of their HD-positive mothers (*, *). On the topic of anticipation, it bears mentioning that HD is one of a dozen genetic disorders that affect the nervous system by means of mutant expansion of normal trinucleotide repeats (Campbell, Reece, & Mitchell, 1999). Other disorders of this kind include Fragile X syndrome and Myotonic dystrophy, the most common adult form of muscular dystrophy (Klug & Cummings, 2002). As with these other triplet-expansion-based disorders, the severity of HD is related to the extent of the expansion. Basically, age of onset and life expectancy, the cardinal measures of HD severity, can be thought of as functions of the trinucleotide expansion. Both of these quantities vary inversely with the degree of expansion. This relationship would imply that a greater number of repeats induces a younger age of onset and a shorter life expectancy. And indeed, this prediction has been borne out repeatedly in human HD patients (*, *; Blumenfeld, 2002; Squitieri et al., 2003) as well as in mouse models (Bolivar et al., 2003; Klug & Cummings, 2002). Proteins To reiterate, the protein of primary concern in HD is huntingtin (Htt). The fact that its presence (in either normal or mutant form) is necessary for extraembryonic membrane function and hence embryonic development has been demonstrated by numerous studies with knockout and transgenic mice (Cotran et al., 1999; Reiner, 2003). Furthermore, instrumental roles for Htt have been discovered in several other crucial functions, namely both the morphogenesis (i.e. arrangement) and survival of neurons in the adult forebrain (i.e. cerebrum, thalamus, and hypothalamus) (Reiner et al., 2003). Studies are currently underway to more fully elucidate patterns of Htt’s ordinary action in both neuronal and nonneuronal signal transduction Huntington’s Disease 8 (MacDonald, 2003). It seems we may only be realizing a fraction of the entire range of functions performed by Htt in its normal capacity. In its abnormal capacity, when at least one Htt gene is sufficiently expanded, there are even more intricacies to consider. Chief among these are the CAG repeats discussed above. The CAG repeats are translated into repeats of the amino acid glutamine (Q) (*, *; Glass et al., 2004). The resultant polyQ segment is what wreaks cellular havoc in HD (Glass et al., 2004; Klug & Cummings, 2002). And, like the trinucleotide repeats from which they arise, the lengths of these polyQ tracts can reliably predict the severity of HD that will be experienced by the individuals possessing them (*, *; Bolivar et al., 2003; Cotran et al., 1999). Exactly how the polyQ region generates the phenotypic symptoms of HD is not entirely known, although we do have evidence to support several ideas about what transpires. For instance, there are many credible assertions that mutant Htt, normal Htt, and fragments of either type of Htt tend to group together and form aggregations (Cotran et al., 1999; Li et al., 2003; Zhou et al., 2003). The significance of these aggregations can best be seen in light of their actions relative to the subcellular structures which make up their environment. Organelles The nucleus was the first organelle to be included in hypotheses about the pathogenesis of HD. It attained this status because the Htt aggregations described above have shown a propensity for being transported into the nucleus (Saudau, Finkbeiner, Devys, & Greenberg, 1998; Zhou et al., 2003). Htt and/or Htt fragments containing the polyQ repeat are transported into the nucleus as part of so-called intranuclear inclusions (Cotran et al., 1999). These inclusions, in turn, were found to coincide with increased apoptosis, i.e. programmed cell suicide, the eventual precipitant of HD (Saudou et al., 1998). This observation suggested that the inclusions might be critically interfering with transcription within the nucleus (Trushina et al., 2003). However, by using cultured neurons of the kind involved in HD, it was determined that preventing nuclear importation of the inclusions did not prevent apoptosis (Saudou et al., 1998). On the contrary, mutant-Htt-induced cell death increased with suppression of nuclear Htt inclusions (Saudou et Huntington’s Disease 9 al., 1998). Hence there must be other at least one other subcellular structure besides the nucleus that interacts with Htt. And in fact the mitochondria do interact heavily with Htt. As the headquarters of essential apoptotic enzymes, the mitochondria have necessarily intimate biochemical exchanges with mutant Htt aggregations (Li et al., 2003; Zhou et al., 2003). The precise natures of all of these interactions remain undetermined, although a significant amount of insight has been compiled. This insight is partially reflected in Figure 1, which tabulates a variety of molecules according to how they are believed to interact with Htt (Sugars & Rubinsztein, 2003). Another collection of subcellular structures with some at least hypothetical connection with Htt are microtubules. Trushina et al. (2003) recently made a convincing case that destabilization of microtubules (a component of the cellular frame, in effect) is a necessary condition for mutant Htt to exert its toxic effects. This study was the first to invoke such a central role for microtubules in the molecular pathology of HD. So naturally, many new questions arise from it, not the least of which is whether the results will be replicated. The replicability has to be questioned because the conclusions of the study rely pivotally on data obtained from cultured cells, which are widely acknowledged as exhibiting erratic behavior in response to even minute alterations to the culture medium. Cells and Tissues The types of cells that undergo apoptosis and are thus implicated in HD are of course neurons. The principally involved neurons, however, are located in the caudate nucleus and putamen, which jointly comprise the striatum of the basal ganglia (Banich, 1997). The initial symptoms of HD correspond to a circumscribed kind of cerebral atrophy, wherein the caudate nucleus is especially affected (Coltran et al., 1999). Within the striatum and, to a lesser extent, the adjacent globus pallidus, the medium-sized spiny neurons that use GABA or acetylcholine are especially vulnerable to Htt-induced apoptosis (Banich, 1997; Coltran, 1999). Due to the apoptosis of these neurons, a particular neural pathway is interrupted. The indirect pathway (which synapses on the external globus pallidus from the striatum as part of a circuit connecting Huntington’s Disease 10 the cortex, basal ganglia, and thalamus) becomes underactive (Banich, 1997). This underactivity subsequently allows the direct pathway to overstimulate the internal globus pallidus (Banich, 1997). The overstimulated internal globus pallidus in turn allows the thalamus to overstimulate physical activity, thus yielding the chorea and other disturbances characteristic of HD (Blumenfeld, 2002). And as the cortex begins its own irreversible atrophic course, the disease progresses toward its usual culmination in global dementia (Banich, 1997). Research Proposal Questions in Need of Address Knowing the aforementioned mechanisms by which HD arises, we would do well to formulate some questions, the answers to which could complement what is known and thereby lead to more and better treatment options. The ultimate overarching question seems to be: Why, at the age of about 38 years, would GABA-ergic and cholinergic neurons in the striatum begin undergoing apoptosis as a result of polyQ aggregates that had been made there since before birth? This question can be subdivided into the following: (1) Why would GABA-ergic and cholinergic neurons ever undergo apoptosis? (2) Under what conditions can polyQ aggregates trigger apoptosis? (3) Why do the GABA-ergic and cholinergic neurons die off before the other types of neurons? (4) Might normal Htt have some properties that are more pronounced or enhanced due to the polyQ extension? (5) What biochemical events typically occur at the age of about 38 years that might make a cell more prone to apoptosis? (6) Is there a way to disassemble or deactivate polyQ aggregates in vivo? (7) Could there be a way to safely prevent the initial aggregation of polyQ segments? (8) What is/are the means of disposal of polyQ aggregates? (9) What are the effects of polyQ aggregates on other cellular proteins? (10) Is there a way to locally inhibit apoptosis in the striatum? Approaches to Answering the Above Questions A myriad of tools and strategies could prove useful in enabling response to the above queries. In any case, I would approach them as follows. (Due to length restrictions not all questions are addressed.) Huntington’s Disease 1. 11 This question would be best addressed in a separate and thorough literature review, where due consideration can be given to caspases and their regulation. 2. This question could be answered by setting up a cell culture assay. An optimal cell line would have a known number of CAG or polyQ repeats, and controllable transcription of the Htt gene. One could then administer variable quantities and combinations of other chemical factors endogenous to the intra- or extracellular environment of the striatum. If this method were less than practical in terms of introducing foreign factors into the cells, other genetic vectors or engineered endosomes could be utilized. Alternatively, DNA microarray analysis could probe differences between the genes expressed by apoptotic and surviving cells. 3. Given enough documented knowledge of the upstream precursors and downstream metabolites of GABA and acetylcholine, one could proceed as described for (2) above, with the modification that the chemical factors being introduced are a controlled set of precursors and/or metabolites of GABA and/or acetylcholine. 5 & 8. An answer to these questions may already have been very fortuitously provided. Zhou et al. (2003) report that toxic polyQ fragments accumulate and aggregate more readily when proteasomes (protein-degrading bodies within cells) become inactive the way they normally do when organisms and their constituent cells get older. In conjunction with this study, the findings of Squitieri et al. (2003) strongly suggest that until a certain age, the proteasomes are responsible for staving off HD. It would seem that prior to the critical age, proteasomal resources of cells are capable of degrading the polyQ aggregations produced by either the hetero- or homozygous HD genotype. But after the proteasomal decline that marks a particular age, the two-fold greater production of mutant Htt by homozygous cells could induce the more rapid degeneration of homozygous HD patients reported by Squitieri et al. This line of research should be especially beneficial because it invites plausible theories of how to boost neural proteasome activity, possibly with a pill or an injection. And in the event that such a prophylactic breakthrough is made, HD could conceivably become a thing of the past. On top of that, there might be some poetic justice in successfully countering genetic anticipation with clinical anticipation. Huntington’s Disease 9. 12 As indicated before, Sugars and Rubinsztein (2003) offer a synopsis of the effects of polyQ aggregates on a variety of other important proteins (See Figure 1). Likewise, Figure 2 shows a currently valid (though almost certainly incomplete) reckoning of certain events that are likely to mediate HD presentation (Bates, 2003). So essentially, this question amounts to an appeal for the continuation of polyQ interaction research. But regardless of the exact methods used and avenues of inquiry followed, it is only in answering the kinds of questions posed above that hope exists for finding the elusive knowledge required for curing illness. Huntington’s Disease 13 References *. (*). [The textbook that had the “Chapter 3: What are the units of brain function?” excerpt in our first set of readings.] Alonso, M. E., Yescas, P., Rasmussen, A., Ochoa, A., Macias, R., Ruiz, I., & Suastegui, R. (2002). Homozygosity in Huntington’s disease: New ethical dilemma caused by molecular diagnosis. Clinical Genetics, 61, 437-432. Banich, M. T. (1997). Neuropsychology: The neural bases of mental function. New York: Houghton Mifflin Company. Bates, G. (2003). Huntingtin aggregation and toxicity in Huntington’s disease. The Lancet, 361, 1642-1644. Blumenfeld, H. (2002). Neuroanatomy through clinical cases. Sunderland, MA: Sinauer Associates, Inc. Bolivar, V. J., Manley, K., & Messer, A. (2003). Exploratory activity and fear conditioning abnormalities develop early in R6/2 Huntington’s disease transgenic mice. Behavioral Neuroscience, 117, 1233-1242. Campbell, N. A., Reece, J. B., & Mitchell, L. G. (1999). Biology (5th ed.). Menlo Park, CA: Addison Wesley Longman, Inc. Cotran, R. S., Kumar, V., & Collins, T. (1999). Robbins pathologic basis of disease. Philadelphia, PA: W. B. Saunders Company. Glass, M., Van Dellen, A., Blakemore, C., Hannan, A. J., & Faull, R. L. M. (2004). Delayed onset of Huntington’s disease in mice in an enriched environment correlates with delayed loss of cannabinoid DB1 receptos. Neuroscience, 123, 207-212. Klug, W. S. & Cummings, M. R. (2002). Concepts of Genetics (7th ed.). Upper Saddle River, NJ: Prentice Hall. Huntington’s Disease 14 Li, L., Fan, M., Icton, C. D., Chen, N., Leavitt, B. R., Hayden, M. R., Murphy, T. H., & Raymond, L. A. (2003). Role of NR2B-type NMDA receptors in selective neurodegeneration in Huntington Disease. Neurobiology of Aging, 24, 1113-1121. MacDonald, M. E. (2003). Huntingtin: Alive and well and working in middle management. Science STKE, 2003, 48. Reiner, A., Dragatsis, I., Zeitlin, S., & Goldowitz, D. (2003). Wild-type huntingtin plays a role in brain development and neuronal survival. Molecular Neurobiology, 28, 259-276. Saudau, F., Finkbeiner, S., Devys, D., & Greenberg, M. E. (1998). Huntingtin acts in the nucleus to induce apoptosis but death does not correlate with the formation of intranuclear inclusions. Cell, 95, 55-66. Squitieri, F., Gellera, C., Cannella, M., Mariotti, C., Cislaghi, G., Rubinsztein, D. C., Almqvist, E. W., Turner, D., Bachoud-Levi, A. C., Simpson, S. A., Delatycki, M., Maglione, V., Hayden, M. R., & Donato, S. D. (2003). Homozygosity for CAG mutation in Huntington disease is associated with a more severe clinical course. Brain, 126, 946-955. The Huntington's Disease Collaborative Research Group. (1993). A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington's disease chromosomes. Cell, 72, 971–83. Trushina, E., Heldebrant, M. P., Perez-Terzic, C. M., Bortolon, R., Kovtun, I. V., Badger, J. D., Terzic, A., Estevez, A., Windebank, A. J., Dyer, R. B., Yao, J., & McMurry, C. T. (2003). Microtubule destabilization and nuclear entry are sequential steps leading to toxicity in Huntington’s disease. Proceedings of the National Academy of Science, 100, 1217112176. Huntington’s Disease 15 Zhou, H., Cao, F., Wang, Z., Yu, Z. X., Nguyen, H. P., Evans, J., Li, S. H., & Li, X. J. (2003). Huntingtin forms toxic NH2-terminal fragment complexes that are promoted by the agedependent decrease in proteasome activity. Journal of Cell Biology, 163, 109-118. Huntington’s Disease Figure 1. Taken from Sugars and Rubinsztein, 2003. 16 Huntington’s Disease Figure 2. Taken from Bates, 2003. 17