Huntington’s Disease
For any condition...
•
•
•
•
•
•
•
•
•
Pathophysiology
Epidemiology
Symptoms
Signs
Diagnosis
Prognosis
Complications
Treatment
Prevention
Pathophysiology
• Huntington's Disease (HD) is an inherited neurological
condition.
• HD is caused by a faulty gene on chromosome 4 (IT-15).
• People with HD have a "molecular stutter" of three
nucleotides (CAG) located in exon 1
• This results in an uninterrupted polyglutamine stretch
within the N-terminus of the huntingtin molecule.
• The "normal" number of CAG repeats is between 9 and
30.
• Between 30 and 39 repeats is a grey area, where people
may or may not go on to develop HD.
• Over 39 is considered defective, and some patients may
have as many as 100 CAG repeats.
• The CAG repeat length is estimated to account for
approximately 70% of the variance in age of onset.
• Extremely large CAG repeats of 80 or greater are often
associated with a disease onset during childhood or
adolescence (juvenile HD).
• There is a tendency for greater repeat expansion when the
father, rather than the mother, transmits the disease causing
mutations.
• These mutations in the gene result in the huntingtin protein
being longer in length. This longer protein then accumulates
abnormally in the brain cells and eventually leads to brain cell
death.
• HD has previously been thought to have 100% penetrance,
however it is now known that the penetrance is dependant on
CAG repeat length.
Normal Male Karyotype
Huntington’s Disease Karyotype
Normal Female Karyotype
Epidemeology
• The altered gene is passed from parent to child without regard for sex.
• If a person does not inherit the altered gene for HD then his or her
children are not at risk of developing HD.
• HD affects approximately 1 in 20,000 people of European descent, and
usually manifests itself between the ages of 30 and 50 years.
• Being an autosomal dominant disorder, children of a person with a
defective HD gene have a 50:50 chance of inheriting the gene from their
affected parent.
• Juvenile Huntington’s occurs in approximately 16% of all cases of
Huntington's.
• 80% of cases with onset before 20 years of age (juvenile HD) are due to
paternal transmission.
• Huntington's disease is about 10 times more prevalent in Western
European populations compared to African and Asian populations.
• Huntington's occurs about twice as often in Tasmania compared to the
rest of Australia due to an individual with Huntington's settling in
Tasmania many years ago and passing the mutation on.
Signs & Symptoms
•
•
•
•
•
•
The most common symptom of the condition is chorea; that is dance-like or jerky
movement of the arms and legs. These movements begin as twitches and gradually
increase over a period of years to larger movements.
Physical Symptoms
In the early stages of HD a person is likely to experience some mild twitching of the
fingers and toes, and perhaps the face or limbs. He or she may feel a little less coordinated, fumbling or knocking things over. As the disease progresses, walking may
become more challenging and, as coordination decreases.
Cognitive Symptoms
“Cognitive" - referring to tasks of the brain concerned with knowing, thinking,
planning, judging and remembering.
Short term memory may be reduced
Over time concentration for activities such as reading and demanding conversation
may be affected.
HD does not affect a person's orientation.
Personality or Emotional Symptoms
Changes to personality will begin subtly. In the early stages of HD, a person may be
more irritable or moody than previously.
Depression is common to about a third of all people affected by the condition.
Some persons affected by HD laugh or smile at inappropriate times or may feel like
crying for no apparent reason.
Diagnosis
• Pre-symptomatic genetic testing is for individuals at risk for HD who
do not have symptoms. Pre-symptomatic genetic testing involves
genetic counselling.
• The requirements for the diagnosis of HD include:
-Medical history
-Family history
-Brain imaging test (MRI, CT, PET)
-Genetic test (if necessary)
-Neurological examination
-Laboratory tests
• During such testing, blood samples are taken from patients and DNA
is directly analysed for HD mutations. The DNA is studied through a
series of tests known as Polymerase chain reactions or PCR testing.
• During this testing, the number of CAG repeats within the IT15 gene
region is estimated. Additional blood samples may be obtained from
close or first-degree relatives with HD to help confirm the results.
• If between 35-40 CAG’s may or may not develop the disease .
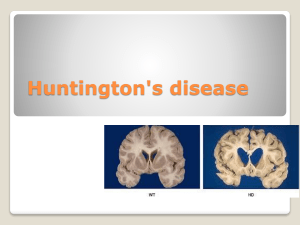
• The area most noticeably damaged is the corpus striatum.
• In some patients, the disease leads to a loss of 25% or more of total
brain weight.
Prognosis
• Once symptoms begin, there is progressive cognitive, motor and
psychiatric impairment; with death occurring an average of 18 years after
onset of symptoms.
• Death for most people with Huntington's disease is usually a result of
infection, pneumonia, heart failure or choking.
• The most common cause of death is pneumonia due to the individual not
being able to clear their lungs properly and having problems with
swallowing, which results in food and liquid entering their lungs.
• The second most common cause of death is heart failure.
• The suicide rate among HD patients is 5-10 times higher than in the
general population.
• Eventually the person is unable to care for themselves and requires total
nursing care.
Complications
• With regard to screening: between 35-40 CAG’s – grey area
• Though the signs and symptoms vary from person to person, vital
functions, such as swallowing, eating, speaking and walking, usually
degenerate over time.
• Depression is common in Huntington's disease, and some people are at
risk of suicide. However, death generally occurs as a result of
complications of the disease, such as a fall or an infection like pneumonia.
• Weight loss and eating difficulties due to swallowing difficulties and lack of
other muscle coordination make management of nutrition important.
• Thickening agents can be added to liquids to make the fluids easier and
safer to swallow and reduce the chance of fluids entering the lungs. If
eating becomes too dangerous or uncomfortable, a feeding tube can be
used.
Treatment
•
•
•
•
•
•
Two Eurepoean scientists made the breakthrough discovery that dopamine
pathways between neurons are destroyed in Parkinson’s disease patients. Since
the symptoms of Parkinson’s disease are nearly the opposite of those with HD, the
scientists hypothesise that decreasing HD patient’s dopamine levels may be a key
step in treating the disease (Late 1950s)
Tetrabenazine (Xenazine) was developed specifically to reduce the severity of the
jerky/involuntary movements occurring in Huntington's disease.
Other drugs are also used to help reduce involuntary movements – these include
neuroleptics and benzodiazepines. The rigidity experienced by some patients can
be treated with antiparkinsonian drugs.
There are drugs which can be used to treat depression.
Physical Therapy is very important as well as speech therapy to help the patient
lead a more normal life.
There is no effective treatment for HD, although some symptomatic relief may be
obtained.
Prevention
• People at risk of passing the genetic defect that causes Huntington's
disease to your children, may wish to consider adoption or certain
forms of assisted reproduction. One possibility is in vitro fertilization
with pre-implantation screening. In this procedure, embryos are
screened for the Huntington's disease gene mutation, and those that
don't have the mutation are then implanted in the woman's uterus.
• A number of compounds that have shown promise in animal studies
and in pilot clinical trials are currently under investigation for the
treatment of Huntington's disease.
• Gene therapies to reduce the amount of mutant Huntington protein in
the brain have shown great promise in the laboratory setting
Caring for people with HD
• People with HD can improve their quality of life by attempting
to remain active physically, mentally and socially. Walking,
reading and maintaining friendships are some examples.
• The person with HD should attempt to live as fulfilling a life as
possible.
• At this point there is no cure for HD, but some symptomatic
treatments and support services are available to individuals
and families affected by HD.
Presymptomatic Testing
• Presymptomatic Testing
The gene responsible for HD was identified in
1993 making it possible for those people who are
at risk to the condition to take a test to determine
whether or not they have inherited the gene.
Candidates for testing must be a minimum of
eighteen years of age, and must want to know
their gene status in order to be accepted for
testing. Extensive support, information and
counselling are available.