SEROLOGY MANUAL - Mount Sinai Hospital
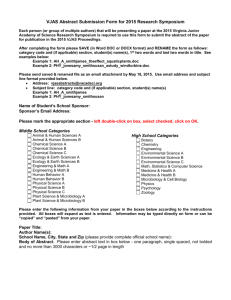
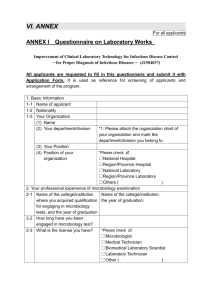
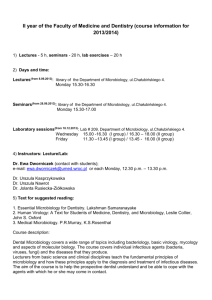
advertisement

Page 1 of Policy # MI/SER/v48 Microbiology Department 116 Policy & Procedure Manual Section: Serology Manual Issued by: LABORATORY MANAGER Original Date: March 14, 2001 Approved by: Laboratory Director Revision Date: October 29, 2015 Annual Review October 15, 2015 SEROLOGY MANUAL TABLE OF CONTENTS Immucor Capture-CMV ........................................................................................................................ 3 Architect System for HBsAb, HBcAb-IgM, HBcAbTotal, HAV-IgM, HCVAb, CMV IgG, CMV IgM, CMV Avidity, HIV-1/2, HTLV I/II, EBV VCA IgG, EBV EBNA-1 IgG, Rubella IgG, Syphilis TP Ab, HBsAg Qualitative and HBsAg Qualitative Confirmatory .................................... 6 Daily Procedure .................................................................................................................................. 8 To add new control lot in LIS ............................................................................................................ 9 To enter NEW Control Lot# onto Architect: ..................................................................................... 9 To order Controls for specific lot #: ................................................................................................ 10 To order reagent Calibration ............................................................................................................ 10 Verify QC results in LIS .................................................................................................................. 11 To manually add an order ................................................................................................................ 12 Cut-off Values.................................................................................................................................. 14 Reflex testing and resulting ............................................................................................................. 15 HBsAg Qualitative Confirmatory: ................................................................................................... 1 To order HBsAg Qulitative Confirmatory Calibration ...................................................................... 1 To order HBsAg Qualitative confirmatory Control: .......................................................................... 1 To order HBsAg Qualitative Confirmatory test for patient ............................................................... 2 STAT Testing: .................................................................................................................................... 3 For needle stick incident: ................................................................................................................... 3 For Case room patients that have no previous prenatal testing done: ................................................ 3 Donor/Recipient Serology reporting: ................................................................................................. 5 Trillium Gift of Life Network Procedure ............................................................................................ 8 Weekly Duties ..................................................................................................................................... 9 Trouble shooting .............................................................................................................................. 11 Quality Control ................................................................................................................................ 15 George Washington Serology Study................................................................................................... 17 Specimen Management for George Washington samples ............................................................ 20 Procedure .......................................................................................................................................... 21 CMV Avidity Trouble Shooting ..................................................................................................... 24 GW CMV Avidity algorithm: ......................................................................................................... 25 GW Hepatitis C antibodies Algorithm: ......................................................................................... 26 CMV Avidity result reporting: ....................................................................................................... 27 Anit-HCV result reporting for Architect: ..................................................................................... 28 HCV Ab EIA Serology for George Washington ............................................................................... 30 Hepatitis Virus Serology ....................................................................................................................... 41 UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 2 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Aspergillus Galactomannan Antigen Detection Assay ...................................................................... 43 Infectious Mononucleosis Heterophile Antibodies .............................................................................. 55 Pneumocystis jiroveci (previously known as P. carinii) DFA TEST ................................................ 57 Syphilis Screening ................................................................................................................................ 61 Varicella-Zoster Virus IgG ................................................................................................................. 64 Appendix I - Serology Test Schedule ................................................................................................... 70 Appendix II - List of Tests Referred Out to Other Laboratories ...................................................... 71 Appendix III - Daily Work-Up for Architect Bench ........................................................................... 74 Appendix IV - Entering and Verifying Serology Refer-Out Results.................................................. 76 Refer-out Reporting Bench Workflow and Notes: ....................................................................... 76 Entering and Verifying Verbal Reports ........................................................................................ 77 Entering and Verifying Serology Refer-Out Results Procedure ................................................. 78 Appendix V - Autoverification Process................................................................................................ 82 Appendix VI - Shipment of Samples to HSC....................................................................................... 85 Appendix VII - Looking Up Previous Hepatitis Results in EPR ..................................................... 86 Appendix VIII - Printing of Pending List............................................................................................ 87 Appendix IX – Donor Serology and Molecular Tests List.................................................................. 88 Appendix X – Movement Throughout Containment Zones ............................................................... 89 Record of Edited Revisions ................................................................................................................. 91 UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 3 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Immucor Capture-CMV 1. Introduction The Immucor Capture-CMV is an in vitro qualitative solid phase red cell adherence test system for the detection of antibodies (IgG plus IgM) to Cytomegalovirus (CMV) in human serum or plasma. Capture-CMV is intended to be used in screening of donors or patients for serological evidence of previous infection by CMV. 2. Specimen Collection Serum or plasma can be separated from red cells and stored at 1-10oC for up to 1 week, or frozen at -20oC freezer. Sample should not be repeatedly frozen and thawed. Gel separation tube for serum collection is not recommended. 3. Procedure a. Reagent preparation: i. Working Wash solution: Add 4mL pHix to 400 mL of Isotonic Saline. Check the pH using litmus paper with range of 6.0-8.0-pH should be 6.5-7.2. Good for 30 days when stored at room temperature. Mark ‘ Date Made’ on Working Wash Solution bottle. ii. Capture-CMV Microtitration wells: Rigid U-bottom microtitration well coated with glycine-extracted and purified CMV antigen obtained from CMV 169 grown in human foreskin fibroblast cells. The wells are enclosed in a foil pouch to which a desiccant and moisture indicator has been added. Store the pouch at 130oC. Remove the number of strips needed and carefully re-seal pouch to prevent the uptake of moisture. Once pouch is opened, the microtitration wells should be used within 2 weeks if the moisture indicator stays blue. The Microtitration wells should not be used if the moisture indicator turns pink. Microtitration wells removed from the pouch should be used within one (1) hour. iii. Capture-CMV Positive Control Serum(weak), store at 1-10oC. iv. Capture-CMV Negative Control serum, store at 1-10oC. v. Capture LISS: a low ionic strength solution containing Glycine-bromcresol purple dye and sodium azide. Store at 1-10oC. vi. Capture-CMV indicator Red-Cells, store at 1-10oC. b. Assay Method: 1. Bring reagents to room temperature. 2. Remove Capture-CMV Microtitration wells from the pouch. 3. Add 2 drops (100 uL ± 10 uL) of Capture-LISS to all test wells. The color will change from purple to blue once the control/specimen has been added. 4. Add 1 drop (50 uL ± 5 uL) of Capture-CMV Positive Control Serum (weak) to a designated well. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 4 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 5. Add 1 drop (50 uL ± 5 uL) of Capture-CMV Negative Control Serum to a designated well. 6. Add 1 drop (50 uL ± 5 uL) of the first specimen to the third well, continue adding to the designated wells for the rest of the specimens. 7. Incubate at 18-30oC for a minimum of 5 minutes, but no more than 30 minutes. 8. Manually wash strips, gently 6 times, with Working Wash Solution. 9. Re-suspend Capture-CMV indicator Red-Cells by gently inverting the vial. Immediately add 1 drop (50 uL ± 5 uL) of Capture-CMV indicator Red-Cells to each well. 10. Load strips into ImmuSpin centrifuge. Centrifuge the microtitration wells using program 1 (350 RCF) for 2 minute. Then centrifuge again using program 2 (650 RCF) for 1 minute. Remove strip(s) from centrifuge immediately, and leave on a flat surface. 11. Place the microtitration wells on an illuminated surface and for adherence or the absence of indicator cells. 4. Interpretation of Result Negative test: A button of the Capture-CMV indicator Red-Cells at the bottom of the test well with no area of adherence indicates the test sample has no detection CMV antibody and the person has not yet been infected with CMV and is presumed to be susceptible to primary infection. Positive test: Adherence of Capture-CMV indicator Red-Cells to part or the entire reaction surface indicates a person with previous current infection and who is presumed to be at risk of transmitting CMV infection but who is not necessarily currently contagious. Indeterminate test: Undefined/rough edged button of Capture-CMV indicator Red-Cells at the bottom of the test well. Appearance of some adherence of the Capture-CMV Indicator RedCells as well as a button formation. Indeterminate CMV antibody status. All results are confirmed by another technologist before reporting. Notes for Donor Resulting: Live donor samples from Sick Children’s Hospital testing positive by the Immucor Capture method will be run on the architect for CMV IgG (8CMS) and CMV IgM (10CMM). UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 5 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 5. Assay Validation Test is valid when: Weak Positive Control shows adherence of Indicator Cells over part or all of reaction surface. Negative Control shows a button of Red Indicator cells at the bottom of the well with no area of adherence 6. Quality Control One Positive Control and one Negative Control must be included with each run. External controls are tested the first week of each month. Run ViroTorch/ ViroTorch-M.as Positive external control and Viroclear as Negative External Control. CAP provides external control testing. All QC is checked by senior technologist. 7. Reference Package insert from Capture-CMV kit by Immucor Gamma, Version 9/10 Capture Guide by Immucor Gamma, Version 200, Revision 7/05 UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 6 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Architect System for HBsAb, HBcAb-IgM, HBcAbTotal, HAV-IgM, HCVAb, CMV IgG, CMV IgM, CMV Avidity, HIV-1/2, HTLV I/II, EBV VCA IgG, EBV EBNA-1 IgG, Rubella IgG, Syphilis TP Ab, HBsAg Qualitative and HBsAg Qualitative Confirmatory I. Introduction The Abbott Architect System is a fully automated random access analyser that utilizes a chemiluminescent microparticle immunoassay (CMIA) technology with flexible assay protocols, refer to as Chemflex®. At first, sample containing either Antigen or Antibody is combined with Antigen or Antibody coated paramagnet particles. Antigen or Antibody present in the sample binds to the Antibody or Antigen coated paramagnet particles. After washing, acridinium-labeled Antigen conjugate or Antibody conjugate is added in the second step. Following another wash cycler, Pre-trigger and Trigger Solutions are added to the reaction mixture. The resulting chemiluminescent reaction is measured as relative light unit (RLU).A direct relationship exists between the amount of Antigen or Antibody in the sample and the RLUs detected by the Architect System optics. Assays run in Architect are as follows: Anti-HBs, Anti-HBc II, Anti-HBc IgM, Anti-HCV, HIV Ag/Ab Combo, HAVAb-IgG, HAVAbIgM, rHTLV I/II , CMV IgG, CMV IgG Avidity, CMV IgM, EBV VCA IgG, EBV EBNA-1 IgG, Rubella IgG, Syphilis TP, HBsAg Qualitaitve II, and HBsAg Qualitative confirmatory. Note: HAVM, HBCM and CMV Avidity are NOT validated on iSR53877 (module 2). II. Specimen Type, Preparation and Storage Specimen type Specimen collected (5mL for adult and 1mL for neonates) in serum separator tube or potassium EDTA tubes may be tested on Architect. For other specimen type refer to each assay package insert. Proficiency testing specimens must follow the accompanying guidelines for processing and storage. Specimen preparation Follow the tube manufacture’s processing instructions for serum and plasma collection tubes. Gravity separation is not sufficient for specimen preparation. Previously frozen specimens must be thaw thoroughly. Mix thawed specimens by low speed vortexing or by inverting 10 times. Visually inspect the specimens. If layering or stratification is observed, continue mixing until specimens are visibly homogeneous. To ensure consistency in results, specimens must be transferred to a centrifuge tube and centrifuged at ≥10,000 RCF (Relative Centrifugal Force) for 10 minutes before testing if UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 7 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual o They contain fibrin, red blood cells, or other particulate matter, o They require repeat testing, or o They were frozen and thawed Transfer clarified specimen to a sample cup or secondary tube for testing. Centrifuged specimens with a lipid layer on the top must be transferred to a sample cup or secondary tube. Care must be taken to transfer only the clarified specimen without the lipemic material. Specimen storage Specimens may be stored on or off the clot, red blood cells, or separator gel for up to 14 days refrigerated at 2-8 oC. If testing will be delayed more than 14 days, remove serum or plasma from the clot, red blood cells, or separator gel. Store serum or plasma at frozen temperature (-10 oC or colder) III. Reagents and bulk solutions REAGENT KIT, CONTROL KIT, CALIBRATOR KIT: Instructions must be carefully followed in each assay package insert. Stored at 4 oC. CONCENTRATED WASH BUFFER: Must be diluted prior to use. Contains 1.5M phosphate buffered saline with antimicrobial agents. Stored at room temperature. PRE-TRIGGER SOLUTION: Contains 1.32 %( w/v) hydrogen peroxide. Once opened, placed on board the system no longer than 28 days, then discards. Stored at 4 oC. TRIGGER SOLUTION: Contains 0.35N sodium hydroxide. Once opened, placed on board the systems no longer than 28days, then discard. Stored at room temperature. PROBE CONDITIONING SOLUTION: Contains recalcified human plasma; has infection risk. Preservatives: Antimicrobial Agent and ProClin 300. Stored at 4 oC. IV. Equipment and Materials ARCHITECT i System ARCHITECT i System Assay CD-ROM ARCHITECT i reaction vessels ARCHITECT i sample cups ARCHITECT i septum ARCHITECT i replacement caps Pipettes For information on materials required for maintenance procedures, refer to the ARCHITECT System Operation Manual. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 8 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual V. Daily Procedure At snapshot screen: 1. Touch ‘Log Off’ to log-on with your initials 2. Touch SCC (system control center) and RSH (Robotic sample handler) and ‘Pause’. The status will change from ‘Running’ to ‘Ready’. (The opening of Reagent Carousel lid and turning of the carousel can only be done when Architect is in ‘Ready’ mode.) 3. Check ‘Supplies’ to ensure adequate consumables on board. A yellow caution symbol will appear when reagents or reaction cells are less than 20%. This consumable should be loaded immediately or the next time the machine is on pause. 4. View Reagent Load List to determine which kits need to be loaded. You may print the Load list if needed. (Touch Reagent Icon on Snapshot, ‘View All’, Touch ‘ASSAY’ to group same reagents together) 5. Performing daily maintenance: a. Touch ‘System’ and ‘Maintenance’ Highlight ‘6041 Daily Maintenance’ ‘Perform’ at the bottom of the screen b. Fill WZ probe maintenance bottle with 25-30 ml of 0.5% Hypochloride (Javex) ( 2.0 ml of Javex with 400 ml of tap water, is good for one month) c. Place a clean septum on probe conditioning solution bottle if a new bottle is opened d. Follow the online instructions. Maintenance will take approximately 21 minutes. e. When completed, empty 0.5% Hypochloride bottle and rinse it with tap water. 6. Load reagents : a. Take out adequate reagents according to the Reagent Load List replacing cap with a clean septum. ! Invert the microparticle bottle (pink label) 30 times for the first time loading on the ARCHITECT system ! If the microparticles do not resuspend, DO NOT USE. Contact senior/charge technologist b. On the reagent package, write down the SN# from the MICROPARTICLE (pink) bottle c. Load the reagent bottles onto architect according to the color of the labels and the colour on the rings. d. All Anti-HCV Reagents already on board should be inverted 3 times. 7. Check reagent controls to ensure there is adequate volume in each sample cup to run QC. (If the level reaches the first mark, then it is still good for one more run). a. Change each sample cup when volume is too low, and fill up to about 1/3 full. Do NOT overfill. Label the top with name of each control; write down lot number, expiration date, and date-in-use on the side. b. If new controls are used, updates in Architect and LIS must be done at the same time. Architect must be paused to change control lots. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 9 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual To add new control lot in LIS: a. Log in to Soft QC b. Press “F1” on the keyboard to exit the EMAILs c. Select #4-Maintenance i) Select “Add new level” Enter old lot # with N/P/P1/P2 or P3 at the end; Enter New lot # with N/P/P1/P2 or P3 at the end; Press 'F12' 3 times ; Press 'Y' Enter expiration date; Repeat with each level; Once all levels are added, press 'F1' to exit. ii) Select “Deactivate old Lot”: Enter old lot# with N/P/P1/P2/ or P3 at the end; Press 'F12' twice; Press 'Y'; Press 'F1' to exit Repeat with each level; Once all levels are deactivated, press 'F1' to exit iii) Activate new lot: Enter new lot# with N/P/P1/P2 or P3 at the end; Press 'F12' twice; Press 'Y'; Press 'F1' to exit Repeat with each level; Once all levels are activated, press 'F1' to exit. To enter NEW Control Lot# onto Architect: a. Change control lot number for the single analyte Log on as ‘ADMIN’, pass word’ ADM’ Architect must be in pause mode. Touch ‘System’, ‘Configuration’, ‘QC Cal Setting’ In the QC-categories panel, ‘QC single analyte’ is highlighted as default. In the Assays panel, choose the assay needs to be updated e.g. HBsAg. Select ‘Configure’. A new screen will come up showing lot #, touch box with bar: Select ‘New lot-copy data’ from the drop down menu Highlight lot #, enter new lot #, Highlight exp date, enter new exp date. Check ‘Default’, then ‘Done’. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 10 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual b. Change control lot number for the multiconstituent controls :CMV avidity and HBsAgQ2+(HBsAg confirmatory) i. Log on as ‘ADMIN’, pass word’ ADM’ ii. Architect must be in pause mode. iii. Touch ‘System’, ‘Configuration’, ‘QC Cal Setting’ iv. In the QC-categories panel , select QC-Multiconstituents v. In the Assays panel, choose the assay needs to be updated: CMV Avidity or HBsAgQ2+. vi. Select ‘Configure’. vii. Press Ctrl+Alt+Print Scrn, configuration summary sheet will be printed viii. Touch box with bar beside Level, select and print out each level configuration summary sheet by pressing Ctrl+Alt+Print Scrn ix. Touch box with bar beside lot number . x. Select ‘New Lot’ from the drop down menu xi. Type now lot# and expiration date xii. Highlight the 1st test in the assay panel xiii. Touch ‘Define data’ xiv. Type the data in the proper place according to the configuration summary sheet for each level. Touch “Add Level”. Then proceed to enter Level 2. xv. Touch ‘Done’ xvi. Repeat from xiii to xvi for all the assays xvii. Review the screen against the print out summary to make sure everything is correct xviii. Check ‘Default’. xix. Touch ‘Done’. 8. Load controls 1) Bar-coded controls: Load bar-coded controls showing barcode directly onto architect 2) Non bar-coded controls: To order Controls for specific lot #: a. Touch ‘Order’, ‘ Control Order’. Select ‘Single Analyte’ b. Scan in Carrier #, type in position #. c. Select the assay, e.g. ‘HBsAg auto’ d. Select the control (P1, P2, Negative) e. Touch ‘Add order’. f. Do this for EACH positive and negative control. To order reagent Calibration (for reagent with new lot number): a. Touch ‘Order’ from snapshot screen, select ‘Calibration’. b. Scan in Carrier #, type in position #. c. Select the assay, e.g. ‘HBsAg auto’ d. Touch ‘Assay option…’ to check the in-use calibrator lot number 1) If the in-use calibrator has new lot number Highlight lot# UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 11 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Enter new calibrator lot# Enter new calibrator expiration date Touch ‘Done’ button; Touch ‘Add Order’ 2) If the in-use calibrator has same lot number Touch ‘Cancel’ button, Touch ‘Add Order’ 9. Once controls are finished, the ‘QC-Cal’ will be flashing. Print out the QC results: Touch ‘QC-Cal’, select ‘QC result review’ Touch ‘C/P’ to group same QCs together Touch ‘Select All’ Touch ‘Print’ Touch ‘Unselect All’ Highlight the assay that have new reagent loaded earlier Touch ‘Details’ to find the reagent which SN matches the one on the reagent package. Write down both reagent and control lot numbers, record new reagent control results into Architect Lot-Cal-QC chart 10. Check the QC results. If there is no flags appeared on the QC print-out sheets: If there is no flags appeared on the QC print-out sheets: Touch ‘Select All’, Touch ‘Release’ to transmit all QC results to LIS 1-2sd flag: - Touch ‘QC-Cal’, select ‘Levey-Jennings graph’ - From Assay panel, select the assay which has 2S flag, touch ‘Done’ If the 1-2sd flag is the first time, write ‘1st time’ on the QC print-out beside the flag. If the 1-2sd flag is the second time, change the control aliquot and repeat QC If there are more than one level has 2S flag for the same reagent, check the control aliquots: - If the control aliquots are old, change the control aliquots and repeat QC - If the control aliquots are new, recalibrate the reagent and repeat the whole set of the controls 1-3sd flag: If the control aliquots are old, change the control aliquots and repeat QC If the control aliquots are new, recalibrate the reagent and repeat the whole set of the controls 11. Verify QC results in LIS - In ‘Softlab’, select ‘Interfaces’ - Double click ‘Instrument Menu’, Double click the ‘ ARCHI Abbott Architect’ - Press ‘Shift’ and ‘+’ keys together to verify each QC result. 12. Finish Architect daily QC in LIS - Go to SoftMic, Click Results, Click virology Worklist, Double click Architect - Click ‘Yes’ in the following window to go to SoftQC. - Complete designed QC . UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 12 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 13. Load patients’ specimen 1) Ensure each label has a “96” extension. A sample cup can be placed inside the blood tube if serum/plasma level is low or sample comes aliquoted. Once samples are loaded, the Orange light will light up. Carriers can be unloaded if there is solid green lights or flashing green/yellow lights. Carriers can NOT be unloaded if there is solid yellow lights. Stat samples can be loaded in individual carrier’s slots at any time. 2) To manually add an order: - Touch ‘Order’, select ‘Patient Order’. - Scan in Carrier #. type in position #. - Touch ID field, scan in order# - Select all the tests required in Assay panel. - Touch ‘Sample details’. - Type in ‘Last name’ and ‘First name’. - Touch ‘Done’, Touch ‘Add Order’ 14. Update supplies A yellow caution symbol ! will appear when reagents or reaction cells are less than 20% under the appropriate module. 1) Wash buffer: - 2 bulk boxes of 10L concentrated wash buffer are on board ALL THE TIME - Working buffer will automatically be filled by ARM system. 2) Trigger/Pre-trigger solution: Change at the beginning of your shift if less than 20%. If the caution symbol appears midway through testing, change the solution the next time the architect is paused. 3) Add reaction cells: i. Monitor the supplies caution symbol, however, ensure there are enough RVs in the hopper so the red sensor light is always on. 1. At snapshot screen, touch ‘Supplies’ 2. Touch ‘Supply status’ 3. Select ‘module 1’ or ‘module 2’ 4. Touch ‘update supplies’ 5. Select ‘RVs added 500/1000’ or enter estimated number (1 bag has 500 RVs) 6. Touch ‘Done’ and ‘Exit’ to go back snapshot screen ! Do NOT overfill RVs to prevent RV jam 4) Liquid waste is drained directly from Architect into the floor drain. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 13 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 15. Once all tests are finished, the ‘Result’ field will be flashing. a. Touch ‘Result’, Select ‘Result review’, b. Highlight the results to be printed. c. Touch ‘Print’, Select ‘Result LIS Report’ and once printed, release highlighted results. (For HBsAg confirmatory result, select ‘Sample Report’) 16. Underline Positive result or anything requiring reflex testing including: HBsAg Qualitative, Positive HCA, Positive HBcAb, Positive HBcAb IgM, Positive HIV, Positive VD, Negative and low Positive Rubella, low Positive CMS, follow reporting chart to report each result - Initial anything you have verified manually - Indicate where reflex testing is being done - Highlight and mark all NEW Hep B Ag or Hep C ab results Leave completed testing printouts on the senior bench for revision. 17. Architect must be on ‘running’ mode overnight, so that all the solutions will be flushed regularly 18. Log the quantity of the buffer bottles used the day before onto Architect consumable log UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 14 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual VI. Cut-off Values Assay LIS code HBsAg (Qualitative) HBsAb HbcAbII HbcII IgM 8HAGX Equivocal/ Gray Zone Neg Pos <1.00 S/CO ≥ 1.00 S/CO Refer to reflex testing details 8HAB 8HBC 8HBCM <10.00 mIU/ml <1.00 S/CO <1.00 S/CO ≥ 10.00 IU/L ≥ 1.00 S/CO ≥ 1.00 S/CO 1.00-5.00 S/CO HCV Ab 8HCA <1.00 S/CO ≥1.00 S/CO Refer to reflex testing details HIV 1&2 8TSC <1.00 S/CO HAV IgM 8HAVG <0.08 S/CO ≥1.00 S/CO* >1.20 S/CO HAV IgG 8HAV <1.00 S/CO ≥1.00 S/CO EBV VCA IgG 8EBVG <0.75 S/CO > or = 1.00 S/CO EBV EBNA-1 IgG 8EBNA <0.5 S/CO > or = 1.00 S/CO Rubella IgG 8RUB 0.00-4.9 IU/mL CMV IgGR 8CMS <6.0 AU/mL CMV IgM CMV Avidity SyphilisTP Ab HTLV I/II HBsAg Confirmatory 10CMM 10CMA 8VD 8HTLA <10 Index <50%(Low avidity) <1.00 S/CO <1.00 S/CO <50% (Not confirmed) 8CON ≥10.00 IU/mL 10.0-15.0 IU/mL (Low Level) ≥6.0 AU/mL 6.00-15.00 AU/mL(Low Level) ≥1.00 Index >50%(High Avidity) ≥1.00 S/CO ≥1.00 S/CO* Reflex Range 0.08-1.20 S/CO (Gray Zone) 0.75-1.00 S/CO (Equivocal) 0.5-1.00 S/CO (Equivocal) 5.00-9.90 IU/mL (Gray Zone) 0.00-9.9 IU/mL >50% (Confirmed) UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 15 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Result Reporting Result reporting includes auto verification by LIS and manually verification by operator. For auto verification process, refer to auto verification process. For manually verification, refer to Reflex testing and resulting VII. Reflex testing and resulting: UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Page 16 of 116 Policy # MI/SER/v48 Microbiology Department Policy & Procedure Manual Section: Serology Manual 8HAGX (HBsAg Qualitative) 8HAGX Patient History 8CHK 8HBC 8HBC2 Positive (>5.0 S/CO) Not Done (Hag+) 8CON both positive (≥1.0 S/CO) Confirmed ≥50% one Positive (≥1.0 S/CO) Positive (>1.00 S/O) New Positive (>1.00S/CO Enter "New Positive" and verify Positive 1.0 ≤HBC<5.0 S/CO one Negative (<1.0S/CO) Both Negative (<1.0S/CO) Negative (<1.0S/C) POSITIVE (>1.00 S/O) Previous Positive Enter "Previous +ve" and verify N/A Comment 1) Report 8HBC and 8HBC2 as per HBC reporting table 2) Do not verify 8HAGX result 3) Order 8CON. 4) Result as “.Conf” (ensure there is a dot before) and verify 5) Highlight 8HAGX new positive on print out and give to Senior for CD Yes Not Confirmed <50% 1) Report 8HBC and 8HBC2 as per HBC reporting table 2) Do not verify 8HAGX result 3) Order 8CON. 4) Result as “.NotConf” (ensure there is a dot before) and verify 5) Consult with Senior or Charge tech. N/A N/A N/A 1) Verify Negative 8HAGX result in LIS 2) Report 8HBC as "Not done Hag+" and verify 3) Delete HBcII in pending list on Architect UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 17 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 8HBC ordered only or HBsAg is ‘Negative’ 8HBC 8HBC2 Positive (>5.0 S/CO) Result ‘Not Need’ and verify both positive (≥1.0 S/CO) one Positive (≥1.0 S/CO) Positive 1.0 ≤HBC<5.0 S/CO one Negative (<1.0S/CO) Both Negative (<1.0S/CO) Comment 1) Report 8HBC as "Positive" and verify 1) 2) 3) 4) 5) 6) 1) 2) 3) 4) 5) 6) 7) 1) 2) 3) 4) 5) 6) There are 2 8HBC reflexes in the pending list on Architect Do not release HBC result before both 8HBC2 complete Print all 3 8HBC results Release all 3 positive results Take off keypad and report 8HBC2 as "Positive" in LIS and verify Report 8HBC as "Positive" and verify There are 2 8HBC reflexes in the pending list on Architect Do not release HBC result before both 8HBC2 complete Print all 3 8HBC results Release both two positive results Take off keypad and report 8HBC2 as "Positive" in LIS and verify Report 8HBC as "Positive" and verify Release negative 8HBC2 from Architect There are 2 8HBC reflexes in the pending list on Architect Do not release HBC result before both 8HBC2 complete Print all 3 8HBC results Release both negative results FIRST, 8HBC will be reported as negative and auto verified Then release positive result Take off keypad and report 8HBC2 as "Negative" in LIS and verify UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 18 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual HCA 8HCA Patient History 8HCA2 >10.00 S/CO Comment 1) 2) 3) 1) 2) New Positive Positive (>10.00 S/CO) <10.00 S/CO Previous Positive 3) N/A <10.00 S/CO 1) 2) 3) 4) 1) 2) New Positive Positive 1.0 ≤HCA<10.00 S/CO >10.00 S/CO Previous Positive N/A 3) 1) 2) 3) Result reflex 8HCA2 as "Positive" and verify Result 8HCA as “Positive”---Do not verify Highlight new positive HCA on print out and give to senior for CD Repeat one more 8HCA If 2 results out of 3 are >10.00S/CO: i) Result reflex 8HCA2 as “Positive” and verify ii) Result 8HCA as “Positive”---Do not verify iii) Highlight new positive HCA on print out and give to senior for CD If 2 results out of 3 are < 10.00S/CO: i) Result reflex 8HCA2 as “Positive” and verify ii) Result 8HCA as “To PHL@MOH+” and verify iii) Order 9HCA and print out send-out form using “RLRF5, RR13” iv) Send specimen to PHL for confirmation 1) Result 8HCA as “Positive” and verify 2) Result reflex 8HCA2 as “Prev. conf” and verify 3) Delete reflex order from pending list on Architect Result reflex 8HCA2 as "Positive" and verify Result 8HCA as “ To PHL@MOH+” and verify Order 9HCA and print out send-out form using “RLRF5, RR13” Send specimen to PHL for confirmation Repeat one more 8HCA If 2 results out of 3 are >10.00S/CO: i) Result reflex 8HCA2 as “Positive” and verify ii) Result 8HCA as “Positive”---Do not verify iii) Highlight new positive HCA on print out and give to senior for CD If 2 results out of 3 are < 10.00S/CO: i) Result reflex 8HCA2 as “Positive” and verify ii) Result 8HCA as “To PHL@MOH+” and verify iii) Order 9HCA and print out send-out form using “RLRF5, RR13” iv) Send specimen to PHL for confirmation Result 8HCA as “Positive” and verify Result reflex 8HCA2 as “Prev. conf” and verify Delete reflex order from pending list on Architect UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 19 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 8RUB 8RUB Negative 0.0-4.9IU/mL 8RUB2 Negative 0.0-4.9 IU/mL Or Gray zone 5.00-9.9IU/mL Negative 0.0-4.9 IU/mL Or Gray zone 5.00-9.9IU/mL Gray zone 5.00-9.9IU/mL Low Positive 10-15IU/mL Low Positive 10-15 IU/mL N/A Comment 1) Result 8RUB2 as “Negative” and verify 2) Result 8RUB as “Negative” and verify 1) Result 8RUB2 as “Negative” and verify 2) Result 8RUB as “Negative” and verify 1) Repeat one more reflex 2) If 2/3 results are negative or grayzone i) Result 8RUB2 as “Negative” and verify ii) Result 8RUB as “Negative” and verify 3) If 2/3 results are low positive i) Result 8RUB2 as “Low Positive” and verify ii) Result 8RUB as “Low Positive” and verify 1) 8RUB will be auto verified 2) Manually change 8RUB result to “Positive@low level” and verify UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 20 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 8CMS 8CMS Comment 6-15Au/mL 1) 8CMS will be auto verified 2) Manually change 8CMS result to “Positive@low level” and verify 8TSC 8TSC ≥1.00S/CO Comment 1) Result 8TSC as “To PHL@MOH+” and verify 2) Order 9TSC and print send -out form using “RL10H, RR10” 3) Send specimen to PHL 8HTLA 8HTLA ≥1.00S/CO Comment 1) Result 8HTLA as “To PHL@MOH+” and verify 2) Order 9HTL and print send -out form using “RL10H, RR10” 3) Send specimen to PHL UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 21 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 8VD 8VD ≥1.00S/CO Comment 1) Result 8VD as “To PHL@MOH+” and verify 2) Order 9VD and print send -out form using “RLRF5, RR13” 3) Send specimen to PHL 8HAV 8HAV >1.20S/CO Comment 1) Result 8HAV as “POSITIVE” and verify 2) Call ward regarding positive HAV IgM result 3) Check report and fax the report (RL15, RL10) to MOH :416-392-0047 on regular hours(8:30-16:30) 4) phone MOH on after-hours(416-392-CITY (2489) 5) Check the link of Reportable Diseases to the Medical Officer of Health 8HBCM 8HBCM ≥1.00S/CO Comment 1) Verify 8HBCM result in LIS 2) No reflex needed UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 1 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual VIII. HBsAg Qualitative Confirmatory: ! Only order 8CON in LIS AFTER the confirmatory results are completed and released Set Architect in Ready Mode, and load the HBsAg confirmatory reagents. To order HBsAg Qulitative Confirmatory Calibration: 1. At snapshot screen, touch ‘Order’, Select ‘Calibration order’. 2. Scan in Carrier #, type in position #. 3. In assays panel, select ‘HBsAg Q2 C2’. 4. Touch ‘Assay option…’ to check the calibrator lot number 1. If the in-use calibrator has new lot number Highlight lot# Enter new calibrator lot# Enter new calibrator expiration date Touch ‘Done’ button; Touch ‘Add Order’ 2. If the in-use calibrator has same lot number Touch ‘Cancel’ button Touch ‘Add Order’ a. Load a carrier with 2 sample cups b. Add Cal1 to position 1 & add Cal 2 to position 2. ! ALWAYS RUN CONFIRMATORY CONTROL BEFORE SPECIMEN To order HBsAg Qualitative confirmatory Control: (Only run HBsAg Qualitaitve II Positive Control): 1. At snapshot screen, touch ‘Order’, Touch ‘Control Order’, Select ‘Multiconstiuent’ 2. Touch box with bars beside ‘Control:’, highlight HBsAgQ2+ 3. In the ‘Panel:’ highlight HBsAgQ2Pa 4. Touch ‘Assay options…’ to check the lot number of control 5. If control lot number changes, follow instruction of Change control lot number for the multicoustituent controls 6. Touch ‘Add Order’ UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Page 2 of 116 Policy # MI/SER/v48 Microbiology Department Policy & Procedure Manual Section: Serology Manual ! Load Control first (Do not show barcode), then patient’s sample To order HBsAg Qualitative Confirmatory test for patient: 1. At snapshot screen, touch ‘Order’, Touch ‘Patient Order’. 2. Scan in Carrier #., Type in position # 3. At SID, Scan in specimen SID# 4. In ‘Panel’, highlight ‘HBsAgQ2Pa’- HBsAg Q2% N, HBsAg Q2 C1 and HBsAg Q2 C2 will be highlighted. 5. Touch ‘Sample Details’ and type in patient’s last name and first name, 6. Touch ‘Done’. Touch ‘Add order’. !Record How Many Tests Left on the Reagent Bottle To Pint HBsAg Qualitative Confirmatory test 1) Highlight all three assays:HBsAgQ2C1, HBsAgQ2C2, HBsAgQ2%N 2) Touch ‘Print’ 3) Select ‘Sample Report’ 4) Touch ‘Done’ Interpretation of Results HBsAgQ2 C2 (S/CO) UNDILUTED HBsAgQ2 %N HBsAg Qualitative Confirmatory Interpretation LIS <0.7 Nonreactive N/A HBsAg : Negative 8CON: Not Confirmed Verify 8CON <10.00 <50% HBsAg: Negative 8CON: Not Confirmed Verify 8CON ≥0.7 Reactive ≥50% confirmed positive for HBsAg ≥10.00 Reactive <50% *Manually dilute 1:500 and Repeat HBsAg Confirmatory Testing . . . 8CON: CONF POS Verify 8CON *Dilute sample 1:20 first: 25uL patient sample + 475uL Architect HBsAg QII Confirmatory Manual Diluent with this use 20uL (1:20) + 480uL of Architect HBsAg QII Confirmatory Manual Diluent for final 1:500 dilution UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 3 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual IX. STAT Testing: !!! Turn Around Time for STAT Testing is 2-hours For needle stick incident: 1) Source Blood: 8HAGX, 8HCA, 8TSC should always be ordered – tested in house 2) Staff Blood: 8HAB, 8HCA should always be tested - tested in house Staff HIV Ag/Ab is sent out to PHL for testing. 3) In order entry, make sure in the ‘Reported to ’ is the respective occupational health department: OHS-MSH occupational health 4) All results must be informed to occupational health department by phoned or email MSH needle stick results: email results to Occ. Health Clinical Nurses (ohcn@mtsinai.on.ca) 5) Follow the Architect SOPs regarding any reactive results. For regular hours (Monday to Friday from 7:45 to 16:00), contact occupational health department to find out patient’s history regarding any reactive results. For after hours (Monday to Friday from 16:00 to7:00), email microbiologist-on-call with result value, patient’s information, and name of attending physician. 6) All sera are stored in 10 years storage boxes. For Case room patients that have no previous prenatal testing done: Case Room Laboratory Contact Information 1) Do all the tests in house. If HIV requested, also order 9HIV and send out unopened specimen or minimum 0.5ml serum to PHL for HIV confirmation testing. 2) All results must be phoned to the ward. 3) Follow the Architect SOPs regarding any reactive result. Microbiologist on-call must be informed with all reactive syphilis S/CO values. For after hours (Monday to Friday from 16:00 to7:00), any reactive HIV screening result must be emailed to microbiologist-on-call with result value, patient’s information and name of attending physician. 4) All sera are stored in 10 years storage boxes UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 4 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual X. Transplant Donor/Recipient Serology Testing 1. STAT serology testing may include the following tests: Test Name Hep B Surface Antigen(Donor Screening Only) Hep B surface Antibody Hep B Core Antibody LIS code 8HAGX Hep C Antibody 8HCA HIV 1&2 Antibody/p24 Antigen HTLV 1&2 Antibody 8TSC 8HTLA CMV Total Antibody Syphilis Screening 8CMSE 8VD EBV VCA IgG 8EBVG 8HAB 8HBC Testing Assay Architect HBsAg Qualitative II, Device#2G22, Abbott Diagnostics Architect Anti-HBC II, Device#8L4425, Abbott Diagnostics Architect Anti-HCV, Device#6C37, Abbott Diagnostics Architect HIV Ag/Ab, Device#4J27, Abbott Diagnostics Architect HBsAg Qualitative II, Device#2G22, Abbott Diagnostics CAPTURE-CMV Kit,Immucor Inc. Architect Syphilis TP Assay [donor screen and cadaveric], Device Identifier 8D06, Abbott Diagnostics Architect EBV VCA IgG assay, Device# 3P65, Abbott Diagnostics Donor Serology and Molecular Testing for at MSH Living Donors Donor Serology and Molecular Testing at Mount Sinai Hospital 2. Testing of cadaveric blood specimens: After initial centrifugation, transfer the supernatant to a centrifuge tube and centrifuge at ≥10,000RCF for 10 minutes prior to testing. 3. NON-STAT test requests e.g. Toxoplasma IgG, VZV IgG, aliquot separate tubes of serum. All initial reactive samples (except 8CMSE) MUST be centrifuged at 10,000 rcf for 10 minutes before repeating in duplicate UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 5 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Donor/Recipient Serology reporting: Test 8HAGX (S/CO) Initial Result Retest In Duplicate LIS Report <1.00 (Nonreactive) N/A 8HAGX:Negati ve@x1 Both results<1.00 (Nonreactive) 8HAGX:Negati ve@x1 Living Donor 8HAGX:Positiv e@x1 ≥1.00 (Reactive) One or both results≥1.00 (Reactive) Cadaveric Donor 8HAGX:Positiv e@x1 <1.00 (Nonreactive) N/A Both results<1.0 8HBC (S/CO) 8HBC:Negative @c1 8HBC:Negative @c1 8HBC2:Negativ e ≥1.00 (Reactive) Negative Indeterminate One or Both results≥1.00 (Reactive) 8HBC:Positive @c1 8HBC2:Positive N/A 8CMSE:Negativ e@cm1 N/A 8CMSE: Indeterminate @cm1 8CMSE 8EBVG S/CO Positive N/A 8CMSE:Positive @cm1 <0.75 (Nonreactive) No Duplicate Retesting Needed Add 8EBNA test 8EBVG: Negative@a1 8EBNA:Based on EBNA result 0.75≤8EBV<1.00 (Grayzone) No Duplicate Retesting Needed Add 8EBNA test 8EBVG:Equivo ca@a1 8EBNA:Based on EBNA result ≥1.00 (Reactive) N/A 8EBV: Positive Comment Auto-verified Verify 8HAGX Order 8COM, recorder all values in the comment under 8COM , verify 8COM Type ‘Repeatedly Reactive’ in the comment under 8HAGX and verify 8HAGX Order 8COM, recorder all HAGX values in the comment under 8COM , verify 8COM FOR ONTARIO LIVING DONOR ONLY, order 9HAG and send specimen to PHL for confirmation. Type ‘Repeatedly Reactive’ in the comment under 8HAGX and verify 8HAGX Order 8COM, recorder all HAGX values in the comment under 8COM , verify 8COM Auto-verified Verify 8HBC &8HBC2 Record all values in the comment under 8HBC2 Type ‘Repeatedly Reactive’ in the comment under 8HBC and verify 8HBC Record all values in the comment under 8HBC2 Manually verify Manually verify For sick kids ONLY Run CMV IgG (8CMS) and CMV IgM (10CMM) on Architect Manually verify Positive 8CMSE result for sick kids needs to run CMV IgG (8CMS) and CMV IgM (10CMM) on Architect Both results are auto-verified Both results are auto-verified Auto-verified UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 6 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Test Initial Result Retest In Duplicate <1.00 (Nonreactive) N/A Both results<1.00 (Nonreactive) 8HCA (S/CO) One or Both results≥1.00 (Reactive) N/A Both results<1.00 (Nonreactive) 8TSC (S/CO) Cadaveric Donor 8HCA:Positive @y1 8HCA2: Positive 8TSC:Negative @z1 8TSC:Negative @z1 Living Donor 8TSC:Positive @z1 ≥1.00 (Reactive) One or both results≥1.00 (Reactive) <1.00 (Nonreactive) N/A Both results<1.00 (Nonreactive) 8HTLA (S/CO) 8HCA:Negative @y1 8HCA:Negative @y1 8HCA2:Negativ e Living Donor 8HCA:Posiitve @y1 8HCA2:Positive ≥1.00 (Reactive) <1.00 (Nonreactive) LIS Report Cadaveric Donor 8TSC:Positive @z1 8HTLA:Negativ e@i1 8HTLA:Negativ e@i1 Living Donor 8HTLA:Positive @i1 ≥1.00 (Reactive) One or bother results≥1.00 (Reactive) Cadaveric Donor 8HTLA:Positive @i1 Comment Auto-verified Verify 8HCA&8HCA2 Record all values in the comment under 8HCA2 Type ‘Repeatedly Reactive’ in the comment under 8HCA and verify 8HCA Record all values in the comment under 8HCA2 & verify 8HCA2 FOR ONTARIO LIVING DONOR ONLY, order 9HCA and send specimen to PHL for confirmation. Type ‘Repeated Reactive’ in the comment under 8HCA and verify 8HCA Verify 8HCA2 Record all values in the comment under 8HCA2 Auto-verified Order 8COM, recorder all values in the comment under 8COM Verify 8TSC. Result as: “Repeatedly reactive” Order 8COM, recorder all values in the comment under 8COM , verify 8COM FOR ONTARIO LIVING DONOR ONLY, Order 9TSC and send specimen to PHL for confirmation. Type ‘Repeated Reactive’ in the comment under 8TSC and verify 8TSC Order 8COM, recorder all values in the comment under 8COM , verify 8COM Auto-verified Order 8COM, recorder all values in the comment under 8COM, verify 8COM Type ‘Repeated Reactive’ in the comment under 8HTLA and verify 8HTLA Order 8COM, recorder all values in the comment under 8COM , verify 8COM FOR ONTARIO LIVING DONOR ONLY, Order 9HTLA and send specimen to PHL for confirmation. Type ‘ Repeated Reactive’ in the comment under 8HTLA and verify 8HTLA Order 8COM, recorder all values in the comment under 8COM , verify 8COM UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 7 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Test 8VD (S/CO) Initial Result Retest In Duplicate LIS Report <1.00 (Nonreactive) N/A 8VD:Negative @V3 Both results <1.00 (Nonreactive) 8VD:Negative @V3 Living Donor 8VD:Positive @V3 ≥1.00 (Reactive) One or Both results: ≥1.00 (Reactive) Cadaveric Donor 8VD:Positive @V3 Comment Auto-verified Verify 8HVD Manually order 8COM, record all values in the comment under 8COM , verify 8COM Type ‘Repeatedly Reactive’ in the comment under 8VD and verify 8VD Order 8COM, record all values in the comment under 8COM , verify 8COM FOR ONTARIO LIVING DONOR ONLY, Order 9VD and send specimen to PHL for confirmation Type “Repeatedly Reactive’ in the comment under 8VD and verify 8VD. Order 8COM, record all values in the comment under 8COM , verify 8COM Donor Specimen Storage: Freeze all serum and plasma donor specimens to DONOR storage box. For specimen storage information refer to Specimen Retention Times manual. For specimen storage location refer to “Equipment Floor Plan” and “Freezer Room Maps” UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 8 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Trillium Gift of Life Network Procedure Refer to Study Manual: Trillium Gift of Life Network Procedure Donor Serology and Molecular Testing at Mount Sinai Hospital for TGLN UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 9 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual XI. Weekly Duties Architect MUST be on Ready mode and log on as ‘ADMIN’ for weekly maintenance and back-ups! 1. Weekly Maintenance a. These procedures appear on the maintenance TO DO list automatically: 6012 Air Filter Cleaning 6014 Pipettor Probe Cleaning 6015 WZ Probe cleaning-Manual b. Select each procedure and touch Perform ! DO NOT FORGET TO REPLACE AND CLEAN THE FILTER UNDER THE ARCHITECT c. Follow onboard instruction to finish each procedure 2. Back up weekly-Every Monday a. Back up files to Architect Set architect on the ‘Ready’ mode From snapshot screen, touch ‘System’, Touch ‘Utilities’ Select ‘F4-create back up’ Touch ‘Done’ b. Back up test results to CD From the snapshot screen, touch ‘Results’ Touch ‘Stored Results’, Touch ‘Select all’, Touch ‘Archive’ Uncheck ‘delete records after archive before next step’(make sure the Touch ‘Done’ Follow the onboard instruction Touch ‘Done’ when test results back-up is finished Write the back-up date on the CD cover c. Back up QC results to CD From the snapshot screen, touch ‘QC-Cal’ Touch ‘Stored QC’, Touch ‘Select all’, Touch ‘Archive’ Uncheck ‘delete records after archive before next step’(make sure the Touch ‘Done’ Follow the onboard instruction Touch ‘Done’ when results back-up is finished Write the back-up date on the CD cover is blank) is blank) 3. Weekly QC in LIS UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 10 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual a. Login to SoftMic, b. Click Results, click virology Worklist, double click Architect c. Click ‘Yes’ in the following window d. Press F12 key when the following window pops up e. Finish the corresponding Architect-Weekly QC 4. Do architect inventory every Friday UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 11 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual XII. Trouble shooting Error LIS is not responding Action 1) At snapshot screen, touch ‘System’ 2) Select ‘Configuration’ 3) Select ‘Host release Mode’ 4) Configure- click on' ON with Query' under 'Bidirectional Host' 5) LIS Icon should appear on Snap Shot Screen. 6) If problem persists, contact Ed Cudek. 1005/Result cannot be calculated, final RLU read is outside the specification of the lowest calibrator. 1) Spin sample at 10,000g(rcf) for 10 minutes and repeat the test; 2) If the same error code persist, enter “PHL@MOH+” in the LIS result. 3) Order send out test(e.g. 9VD) and send the specimen to PHL for testing 1) Check connection of Dlink modem (little white box) 2) Check connection between instrument and LIS (purple plug) 3) Turn off and restart the whole system in proper sequence. i. To turn off the system: a. Turn off computer first by touching ‘F3 shutdown’ b. Follow instruction till monitor screen goes black c. Press computer power switch d. Turn off the architect ii. To turn on the system a. Press computer power switch b. Wait the computer starting up until the snapshot screen comes up c. Turn on the architect instrument 4) If problem persists, call architect hotline Both SCC (system control center) and RSH (Robotic sample handler) are ‘Offline’ Negative query received for Sample ID (######) 1) Check if the tests are done in LIS 2) If the tests are not done: Order manually on Architect Download test through LIS 1) Log into Softlab 2) Click interfaces UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 12 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Cancel architect order from LIS 1. 2. 3. 4. 3) Double click instruments 4) Double click #6 ARCHI 5) Click loadlist on the top menu bar 6) Select ‘Build….’ 7) Click ‘More>>’ 8) Type the order twice at ‘Range of orders’ 9) Click’OK’ 10) Instrument Menu window pops up saying ‘# orders and # tests were added or updated in the loadlist’ Click Interfaces Double click Instrument Menu Double click ARCHI Click Loadlist at the top 5. Click Filter at the bottom 6. Change How to Display to: ‘By Order’ 7. Type the order# at Starting From field only UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 13 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 8. Click OK 9. The specific order will appear at the very bottom of the list 10. Highlight the order, all tests belong to this order appear on the right panel 11. Click the test to be cancelled (e.g. 8HAG) 12. Click the Toggle Cancel Status x 13. Click Save symbol to save the cancellation Save Cancel Status Test to be cancelled UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 14 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Instrument failure 1. Write down error code(s) in Architect Analyser History Log book, call Abbott Technical Help Line@ 1-877422-2688 for instruction to solve the problem(s).Instrument serial # is iSR06299. 2. If problem cannot be solved by the operator(s), Abbott will send technical service specialist on site(Except weekends and holidays). 3. If technical service specialist comes and replaces parts, all Abbott controls have to be re-run before testing patient samples. 4. Also run external control Virotrol for HBsAg. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 15 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual XIII. Quality Control Abbott Controls: Positive and negative controls must be run for all assays once per 24 hour shift. Always run the positive control followed by the negative control. Control results are verified by a senior technologist and filed in Architect printout log. Run external control Virotrol for HBsAg after any service. External Controls: Select Packaging Product VIROTROL I 1 x 5ml Cat # 00101 10 x 4 ml VIROTROL II 1 x 5 ml Class F HBsAg, Abbott Architect Anti-HIV-1, Abbott Architect HIV ½ Ag/Ab combo1/2 Anti-HTLV-I, Abbott Architect Anti-HBcore, Abbott Architect Anti-HCV, Abbott Architect Anti-CMV Total EIA, Abbott Architect B+ Anti-HBs, Abbott Architect AUSAB (preferred) Anti-HAV, Abbott Architect HAVAB 2.0 (preferred) B Anti-HBc IgM, Abbott Architect CORE-M Anti-HAV IgM, Abbott Architect C HIV-2 N/A HIV-1 (P24) Ag N/A All(except Rubella IgG) N/A CMV IgG N/A CMV IgM N/A Syphilis TP Ab Cat # 00104 VIROTROL III 1 x 5 ml VIROTROL HIV-2 Cat # 00105 1 x 5 ml VIROTROL HIV-1 Ag Cat # 00108 1 x 5 ml Analyte, Test Method VIROCLEAR Cat # 00112 1 0x 4 ml VIROToRCH 1 x 5 ml Cat# 000109 VIROToRCH-M 1 x 5 ml Cat# 000117 VIROTROL SYPHILIS 1 x 5 ml Cat# 00071X UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 16 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 1. External Controls are entered in Architect External QC. All QC controls are verified by a senior technologist. 2. If any external control result is out of range, withhold test results. Repeat with a new aliquot and consult with Charge/senior technologists for review. 3. CAP, IQMH, and NML provide external proficiency testing 4. Calibrations: Run calibration for each new reagent lot or when control(s) fail. 5. Failed QC (Abbott controls and external controls): Test is invalid without satisfactory QC results. Do not release reagent for use pending resolution. XIV. Reference Abbott Operation Manual (201837-106). Assay Packages inserts. For Health Canada approved donor test licence numbers for non-TGLN donors Donor Serology and Molecular Testing at Mount Sinai Hospital UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 17 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual George Washington Serology Study I. Introduction George Washington serology study includes CMV IgG Avidity and Anti-HCV. Infections with Cytomegalovirus (CMV), a member of the herpesvirus family, are common in men and are usually mild and asymptomatic. However, in pregnant women, newborns, and immunocompromised individuals CMV infections may pose a significant medical risk. CMV infection remains difficult to diagnose on symptoms alone since a high percentage of infections remains asymptomatic. In utero infection may result in sequelae of varying degrees including mental retardation, chorioretinitis, hearing loss and neurologic problems. Since the risk of in utero virus transmission and CMV related damage of the fetus is markedly increased during primary infection, reliable recognition of primary CMV infection is of high importance for pregnant women. Although presence of anti-CMV IgG reduces the likelihood of CMV related complications, it does not assure complete protection from disease. The functional binding affinity or avidity of IgG antibodies increases progressively over time after immunization, also known as maturation of the humoral immune response. High percentage of low avidity IgG antibodies may indicate a primary infection whereas high percentage of high avidity IgG antibodies may indicate a recurrent infection. The ARCHITECT CMV IgG Avidity assay is a qualitative method of the chemiluminescent microparticle immunoassay (CMIA) for the determination of the avidity of IgG antibodies to Cytomegalovirus in human serum and plasma. It is used as an aid in the differentiation between primary and non-primary infection. If primary infection needs to be excluded, CMV IgG reactive samples should be tested for CMV IgM and CMV IgG Avidity. A positive CMV IgM result in combination with a low avidity result is a strong indicator for a primary CMV infection within the last 4 months. HCV is a bloodborne virus. The presence of anti-HCV indicates that an individual may have been infected with HCV, may harbor infectious HCV, and/or may be capable of transmitting HCV infection. The ARCHITECT Anti-HCV assay is a qualitative method of the chemiluminescent microparticle immunoassay (CMIA) for the detection of antibody to hepatitis C virus in human serum and plasma. II. Specimen Type , Preparation and Storage Specimen type Specimen collected (5mL for adult and 1mL for neonates) in serum separator tube potassium EDTA tubed may be tested on Architect . Other specimen type refers to each assay package insert. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 18 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Proficiency testing specimens must follow the accompanying guidelines for processing and storage Specimen preparation Follow the tube manufacture’s processing instructions for serum and plasma collection tubes. Gravity separation is not sufficient for specimen preparation. Previously frozen specimens must be thaw thoroughly. Mix thawed specimens by low speed vortexing or by inverting 10 times. Visually inspect the specimens. If layering or stratification is observed, continue mixing until specimens are visibly homogeneous. To ensure consistency in results, specimens must be transferred to a centrifuge tube and centrifuged at ≥10,000 RCF (Relative Centrifugal Force) for 10 minutes before testing if - They contain fibrin, red blood cells, or other particulate matter, - They require repeat testing, or - They were frozen and thawed Transfer clarified specimen to a sample cup or secondary tube for testing Centrifuged specimens with a lipid layer on the top must be transferred to a sample cup or secondary tube. Care must be taken to transfer only the clarified specimen without the lipemic material. III. Reagents and Bulk solutions Abbott REAGENT KIT, CONTROL KIT, CALIBRATOR KIT : Must be carefully followed the instruction in each assay package insert. Stored at 4 oC. Abbot CONCENTRATED WASH BUFFER: Must be diluted prior to use. Contains 1.5M phosphate buffered saline with antimicrobial agents. Stored at room temperature. Abbott PRE-TRIGGER SOLUTION: Contains 1.32 %( w/v) hydrogen peroxide. Once opened, placed on board the system no longer than 28 days, then discards. Stored at 4 oC. Abbott TRIGGER SOLUTION: Contains 0.35N sodium hydroxide. Once opened, placed on board the systems no longer than 28days, then discard. Stored at room temperature. Abbott PROBE CONDITIONING SOLUTION: Contains recalcified human plasma; has infection risk. Preservatives: Antimicrobial Agent and ProClin 300. Stored at 4 oC. Ortho REAGENT KIT, CONTROL KIT: Must be carefully followed the instruction in package insert. Stored at 4 oC. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 19 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual IV. Materials and Equipment ARCHITECT i System ARCHITECT i System Assay CD-ROM ARCHITECT i reaction vessels ARCHITECT i sample cups ARCHITECT i septum ARCHITECT i replacement caps Pipettes or pipette tips (optional) EVOLIS ™ Analyzer For information on materials required for maintenance procedures, refer to the ARCHITECT System and Evolis analyser Operation Manuals. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 20 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual V. Specimen Management for George Washington samples Open box at specimen receiving assigned area for George Washington samples Remove icepacks and dry ice, break down boxes for recycling and discard styrofoam Open one canister at a time, remove samples from packaging materials Count the quantity of the sample per canister and record on the manifest Place the samples into a green plastic bin. Each manifest order should have a separate bin Discard canisters for plastic recycling Move green bins to serology accessioning area Compare the recorded samples number to the number on the manifest Do the numbers match? NO Inform senior technologist YES UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 21 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Accession samples using the barcode on the tubes DO NOT MANULLY ENTER Place large LIS barcode label on tube, do not covering original barcode and leaving sample number visible Place small LIS barcode label on manifest Scan each tube into the excel manifest. Verify proper tests were ordered. Take special care with highlighted orders; those that do not have the standard testing panel: CMV IgG/CMV IgM/HCA Centrifuge all samples Bring all centrifuged samples to Architect bench VI. Procedure 1. Refer to Architect SOP and Evolis SOP for maintenance. 2. Place Architect Anti-HCV, CMV-IgG R , CMV-IgM, and CMV Avidity reagents on the system. 3. Make sure all reagents has been calibrated. Refer to Architect calibration procedure for new lot calibration 4. Refer to Architect control procedure for Anti-HCV, CMV-IgG R, and CMV-IgM for controls ordering 5. Load George Washington specimen onto architect system 6. Once all tests are finished, the ‘Result’ field will be flashing. Print: ‘Result lis Report’ UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 22 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 7. Touch ‘Reruns’ from snapshot screen and delete all CMV-IgG reruns 8. Place all negative specimens in the aliquot rack. These specimens will be stored at -70 oC for 6 months 9. Aliquot any specimen with the value of Anti-HCV is less than 5.00 S/CO and store them in the positive CMV avidity + box (Freezer MIFTW beside the dark room). 10. For Anti-HCV ≥5.00S/CO, repeat Anti-HCV in duplicate on Architect: 1) Both results <5.00S/CO , Anti-HCV is Negative, make an aliquot and put in positive CMV avidity + box (Freezer MIFTW beside the dark room) 2) One result<5.00S/CO and one result ≥5.00S/CO, Anti-HCV is Positive, place an aliquot in the Evolis rack (MIRT8) 3) Both results≥5.00S/CO, Anti-HCV is Positive, place an aliquot in the Evolis rack (Fridge MIRT8) 11. Refer Evolis SOP to run Anti-HCV 12. For CMV IgM≥1.00 Index & CMV IgG Reactive: Order CMV Avidity control(Control L= Level 1, Control H= Level 2): 1) Touch ‘Order’, Touch ‘Control order’ 2) Scan in Carrier #. Type in position # 3) Touch box with bar beside ‘Control’, highlight CMV Avidity 4) Make sure Level 1 is selected 5) In Assay panel, touch CMVAvidity 6) Touch ‘Add order’ 7) Touch box with bar beside ‘Control’, highlight CMV Avidity 8) Select ‘Level 2’ 9) In the Assay panel, touch ‘CMVAvidity’ 10) Touch ‘Add order’ 11) Touch ‘Exit’ to go back snapshot screen Order CMV Avidity for patient’s specimen: 1) Touch ‘Order’, Touch ‘Patient order’ 2) Scan in Carrier #. Type in position # 3) At SID field, scan in specimen order# 4) In panel field, touch CMV G>AV (CMV IgG R and zz-3009 are selected in Assay panel) 5) Touch ‘Sample details’, type in Last name and First name 6) Touch ‘Done’, Touch ‘Add order’, Touch ‘Exit’ Load CMV Avidity controls and patient’s specimen When CMV Avidity controls complete, print out the control list and release results Check patient specimen order status 1) Touch ‘Order’ 2) Touch ‘Order Status’ 3) Touch ‘C/P’ UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 23 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 4) Check the specimen order status Proceed the following steps ONLY when both CMV IgG R and zz-3009 complete ! DO NOT RELEASE ANY RESULT YET Check CMV IgG R result 1) If CMV IgG R≥250 i. Reload patient’s specimen onto Architect ii. Once CMV IgG R completes with an end-point value, Reload specimen onto Architect to get final CMV avidity result 2) If CMV IgG R<250, i. Reload specimen onto Architect to get final CMV avidity result Check patient’s CMV Avidity result 1) If CMV Avidity ≥50% i. Print and release related results: CMVAvidity, CMVvi2, CMVAvi1, zz_3009, CMV IgG R 2) If CMV Avidity<50% i) Print and release all related results: CMVAvidity, CMVvi2, CMVAvi1, zz_3009 , CMV IgG R ii) CMV Avidity and CMV IgM must be repeated. iii) Order CMV Avidity AND order CMV IgM at same time iv) Load patient specimen onto Architect v) Check patient specimen order status a. Look for the specimen order status vi) Proceed the following steps ONLY when both CMV IgG R and zz-3009 complete ! DO NOT RELEASE ANY RESULT YET vii) Check CMV IgG R result a. If CMV IgG R≥250 • Reload patient’s specimen onto Architect • Once CMV IgG R complete, which has end-point value, Reload specimen onto Architect to get final CMV avidity result b. If CMV IgG R<250 Reload specimen onto Architect to get the final CMV avidity result viii) Check the 2nd CMV avidity result a. If CMV avidity result<50% (Matches the 1st avidity result) Pritn and release related results: CMVAvidity, CMVvi2, CMVAvi1, zz_3009, CMV IgG R, CMV IgM b. If CMV avidity result ≥50% (Does not match the 1st avidity result) UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 24 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Print and Release related results: CMVAvidity, CMVvi2, CMVAvi1, zz_3009 , CMV IgG R, CMV IgM Repeat one more CMV Avidity test to get 2/3 results CMV Avidity Trouble Shooting Unable to calculate CMV avidity due to high value of CMV IgG Perform 1:50 dilution on the specimen: 10µL specimen + 490 µL Architect Multi-Assay manual Diluent Repeat CMV avidity ONLY on architect (order CMV G>AV on Architect) Note: If CMV IgM must be repeated, use neat specimen. 13. Aliquot any CMV avidity positive specimen and store in CMV Avidity+ box (Freezer MIFTW beside the dark room) UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Page 25 of 116 Policy # MI/SER/v48 Microbiology Department Policy & Procedure Manual Section: Serology Manual VII. GW CMV Avidity algorithm: Load sample on to Architect CMV IgM : Greyzone Or CMV IgM: Nonreactive Or CMV IgM Positive but CMV IgG Negative CMV IgM : Reactive & CMV IgG Reactive Manually Order CMV avidity on Architect and load sample CMV IgG R≥250AU/mL CMV IgG R<250AU/mL Reload sample back on architect to do CMV IgG R dilution Check if zz_3009 is completed before proceed next steps Reload sample back on architect to do CMV avidity Avidity ≥50% Avidity<50% Manually Order CMV avidity and CMV IgM on Architect Load sample on to Architect CMV IgG R≥250AU/mL CMV IgG R<250AU/mL Reload sample back on architect to do CMV IgG R dilution Check if zz_3009 is completed before proceed next steps Reload sample back on architect to do CMV avidity Avidity<50% Avidity ≥50% Manually Order CMV avidity only on Architect Load sample on to Architect CMV IgG R<250AU/mL CMV IgG R≥250AU/mL Reload sample back on architect to do CMV IgG R dilution Check if zz_3009 is completed before proceed next steps UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT Reload sample back to do avidity NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form areon notarchitect controlled andCMV should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Print and release results Policy # MI/SER/v48 Page 26 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual VIII. GW Hepatitis C antibodies Algorithm: UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 27 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual IX. CMV Avidity result reporting: 1) CMV Avidity≥50%, every results are autoverified except the following: LIS order Result Comment 10CMR Not Needed Verify Result 2) CMV Avidity<50%, 2nd CMV AVIDITY <50%, *Manually order 10CA2 in LIS LIS order Result 10CMA 1st CMV Avidity result 10CMR Repeated CMV IgM result 10CA2 2nd CMV Avidity result Comment Verify Result Verify Result Verify Result 3) CMV Avidity<50%, 2nd CMV AVIDITY >50%, RUN ONE MORE CMV AVIDITY. 10CA2 and 10CA3 must be manually ordered in lis 3RD CMV Avidity <50% LIS order Result Comment 10CMA 1st CMV Avidity result Verify Result 10CMR Repeated CMV IgM result Verify Result 10CA2 2nd CMV Avidity result Verify Result 10CA3 3RD CMV Avidity 3RD CMV Avidity≥ 50% LIS order Result 10CMA 1st High CMV Avidity result 10CMR Repeated CMV IgM result 10CA2 Low CMV Avidity result 10CA3 Last high CMV Avidity Verify Result Comment Verify Result Verify Result Verify Result Verify Result 4) Leave all CMV Avidity results print-out papers on Senior bench UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 28 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual X. Anit-HCV result reporting for Architect: 1) Initial Anti-HCV Reactive<5.00 S/CO LIS Code Result 8HCA Negative 8HCA2 Architect value 8HCAE Not processed Comment Verify result Verify Result In the comment , type ‘Test not requested’ and Verify 2) Initial Anti-HCV≥5.00 S/CO Both duplicated Anti-HCV <5.00S/CO LIS Code Result Comment 8HCA Negative Verify result 8HCA2 Negative In the comment, type all 3HCA , Verify Result 8HCAE Not processed In the comment , type ‘Test not requested’ and Verify One Anti-HCV<5.00 S/CO and one Anti-HCV≥5.00 S/CO LIS Code Result Comment 8HCA Check# Do NOT Verify In the comment, type all 3 HCA results separated by / (e.g.:### / ### / ###) 8HCA2 Type two repeated Verify Result HCA results 8HCAE Leave blank Do NOT Verify Both duplicated Anti-HCV ≥5.00 S/CO LIS Code Result Comment 8HCA Check# Do NOT Verify In the comment, type all 3 HCA results separated by / (e.g.:### / ### / ###) 8HCA2 Type two repeated Verify Result HCA results 8HCAE Leave blank Do NOT Verify 14. Final reporting after 8HCAE results available from Evolis 8COM must be ordered after initial 8HCAE result is available UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 29 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual XI. Reference Abbott Operation Manual (201837-106). Assay Packages inserts. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 30 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual HCV Ab EIA Serology for George Washington I. Introduction ORTHO HCV 3.0 ELISA Test System with Enhanced SAVe is a qualitative, enzyme-linked immunosorbent assay for the detection of antibody to hepatitis C virus (anti-HCV) in human serum or plasma. II. Specimen Collection and Processing a. Blood, serum or plasma collected by clients. b. If blood tube received, centrifuge at 3000 rpm for 10 minutes. III. Instrument EVOLIS ™ Analyzer IV. Reagents 1. Hepatitis C Virus(HCV) encoded Antigen coated Microwell plates (5) 2. Conjugate-Antibody to Human IgG(Murine Monoclonal)-anti-human IgG heavy chain(murine monoclonal) conjugated to horseradish peroxidase with stabilizers 3. Specimen Diluent 4. OPD tablets(30) contains o-phenylenediamine∙2HCL 5. Substrate Buffer-citrate-phosphate buffer with 0.02% hydrogen peroxide 6. Positive Control(Human) 7. Negative control(Human) V. Preparation 1. Before beginning EIA assay, fill up Ortho wash buffer container (yellow tubing) when necessary: *Working Orthodiagnostic Wash buffer: Add 100ml of 20X Ortho wash solution to 1900 ml of distilled water 2. De-ionized Water: Fill up Evolis containers (blue and red tubing) with de-ionized water 3. Transfer the ORTHO (4N sulfuric acid) Stop Solution into a 60ml EVOLIS container, 4. Aliquot HCV Ab and controls into separate 2ml sample containers, *When transferring solutions, use new containers for each new Lot #. Always have name, lot number, expiration date and date transferred. 5. Bring microwell plates and the above mentioned reagents to room temperature before use. 6. Empty the waste tank and check the system liquid container (refill if necessary). System Liquid Preparation: 2 ml of Tween 20 to 10L of de-ionized water. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 31 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual VI. Procedure 1 Turn “ON” the EVOLIS analyzer first and then the computer at the beginning of the day. 2 Double click on the EVOLIS icon located on the computer desk-top. 3 Log onto the system by clicking on “OK”, no password is required. 4 A self-test of the system is automatically initialized each time the EVOLIS software is run. The self-test is considered satisfactory if the word “PASSED” appears beside each instrument module. Print a copy of the self-test report and combine it with the worklist and result sheets. 5 Make specimen tasklist. Prepare specimens by removing the lids and loading all sample tubes with the barcode visible (facing out) on the sample rack (rack code T). 6 Check the quality of the samples by ensuring all clots, foam and bubbles have been removed. 7 Open the door to the sample and reagent unit. Load the sample rack with the bar-codes facing the bar-code reader onto the track marked by the solid red LED light. 8 The ‘Patient Editor’ dialog box will appear with the specimen numbers from the loaded rack. Double check that the specimen numbers and test are correct. If there is a blank space under the patient ID column, click on the space and enter the specimen number manually. All specimen numbers entered manually will be flagged with the code “ManID” on the results report. 9 Choose the assay from the drop down menu which appears along the top of the Patient Editor dialog box, use the scroll bar at the bottom of the dialog box to select additional assays : HCV_Ab assay= ACHCV_ORTHO 10 A check mark is shown for a sample where the HCV Ab assay has been selected. 11 Once HCV Ab assay has been selected for each sample click ‘Close’ to save. A solid LED light will show up for the next available track in the sample and reagent unit which indicates where the next sample rack can be loaded. Repeat steps 6 to 11 for each new sample rack that is loaded on to the analyzer. 12 A total of four sample racks need to be loaded on to the analyzer even if all the sample racks are not required, in order for the reagent template to be used in a later step. When an empty UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 32 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual sample rack is loaded on to the analyzer just click ‘Close’ when the Patient Editor dialog box appears. 13 To check and validate the worklist click on the ‘New Worklist’ icon located on the upper toolbar and the Set-Up dialog box will appear. 14 Click on the “+” next to each plate to see which assay is programmed for which plate. Click on “+” beside the assay file name that is associated with each plate. The plate layout will appear at the right hand side of the dialog box and will show the total number of controls and specimens to be tested, their assigned wells and the number of strips required for each assay. Print plate layout. 15 If duplicate samples need to be tested : a) From the Patient Editor dialog box select the assay folder in which the duplicate sample needs to be run and click ‘Add Patient’. b) The Select Patient(s) dialog box will appear. c) Check the Allow multiple determinations box which appears at the bottom of the Select Patient|(s) dialog box. d) The patient sample IDs will appear. Click on the sample ID in which multiple testing is required and click OK. e) In the Set-up Panel dialog box, a (x2) will appear beside the patient ID under the assay folder in which it was selected. 16 If all the information is correct click ‘OK’ to validate the worklist. 17 A separate dialog box asking for the reagent lot numbers will appear d. Double check the lot numbers and expiry dates and click ‘OK’ if everything is correct. 18 Click on the “+” to expand the Work folder and click on ‘Plate Layout’, the number of microwell strips required for each assay can be reviewed. Click the ‘Print’ button located along the top of the toolbar to print the plate layout if desired. 19 Click ‘START’ (green button) located on the upper tool bar to open the Load dialog box. 20 The Load dialog box appears and shows where to load all the required resources 21 Load all required resources from left to right: a) HCV Sample Diluents b) Pipette tips: Grey = 1100 ul tips (full rack) Brown= 300 ul tips (full rack) Red = Incomplete tip rack *The pipette tips have to be loaded in the exact position as shown in the layout c) Load the reagents on the reagent racks according to the following templates UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 33 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual (Figure 1-3). d) Ensure all caps on the reagent/control containers have been removed before loading them onto the analyzer. 22 Manually Assigning Reagent Locations—Only if Necessary a) Load the reagents and controls into the desired positions on the reagent racks and load the racks onto the analyzer. The reagent racks will appear blank when loaded. b) Different coloured circles representing the reagents/controls will be found at the right hand column of the Load dialog box under the section ‘Unallocated Resources’. Moving the mouse over each circle tells you which reagent/control it represents. c) Click on the circle and drag it over to the correct position in which the reagent/control has been placed on the reagent rack. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 34 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual d) The position of bar-coded reagent/control containers do not have to be manually assigned, their location would be read by the bar code reader. 23 Once all the reagents and controls have been added to the racks, load the reagent racks into the sample and reagent unit in the following order: a) 1st ‘0’- Large reagent rack b) 2nd ‘1’- Medium reagent rack c) 3rd ‘3’- Small reagent rack 24 In the Load dialog box, click the ‘Open Reagent Layout’ button. Select the file name HCV only and click ‘Open’. All reagents and controls will be automatically allocated to their assign position. 25 Once all the required resources have been loaded onto the analyzer click ‘OK’ and the Load dialog box will disappear. The analyzer will begin to check the resources to ensure their amounts are sufficient. 26 The Load Plate dialog box will then appear. Rename the plate ID with HCV and check the lot and expiration date. 27 Insert the microplate making sure that the A1 position of the plate and holder match each other. 28 Click ‘OK’. 29 After the microplate is loaded, the analyzer will start to run automatically. 30 From the Work folder click on ‘Schedule’ to view the chorological order and completion time of the run. Take note of the amount of time required before operator intervention is needed (for OPD preparation and loading). Prepare the required OPD substrate in a 30ml Evolis vial before operation intervention is necessary and store the OPD in a dark location before loading is required. 31 While the samples are being pipetted click on ‘Active Event Log’ to ensure that all samples were pipetted successfully. Look for any red flags that may appear in the “Dispense Sample” section which indicates that an error has occurred. The analyzer will pause and flag with an error message if a clot or low sample volume is encountered, allowing for operator intervention. It will specify position on rack and where and how much of the sample to transfer on the microplate. 32 Prepare orthodiagnostic HCV Ab OPD Substrate within 1 hour before the intervention is requied 1 OPD tablet + 6 ml of Substrate Buffer for 1 – 3 strips 2 OPD tablet + 12 ml of Substrate Buffer for 4 – 7 strips 33 There are 2 alarms requiring operator intervention. After the second alarm and the Load dialog box will appear with the message: ‘Please load the requested items as soon as possible as the system is paused’. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 35 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 34 Open the door to the sample and reagent unit and place the OPD substrate to the correct location without removing the reagent rack from the analyzer. Close the door to the sample reagent unit and click ‘OK’ in the computer. 35 Once the HCV Ab assays is finished a dialog box prompting the removal of the plate and carrier from the analyzer will appear. 36 Remove the microplate and click ‘OK’. 37 A blinking red LED light in the sample and reagent unit indicates that the reagent or sample racks can be unloaded from the analyzer. 38 Remove all samples and diluents from the dilution area. 39 Do not unload pipette tip racks from the analyzer unless they are completely empty. 40 The results report will automatically be printed after each assay is completed. 41 Close the EVOLIS software. Select File | Exit from the menu bar or click the X icon at the top right-hand corner of the Evolis software and shut down the computer. 42 Switch off the Evolis analyzer. 43 Open the instrument cover and wipe the tip adapter (pipettor head) with 70% Ethanol wipes. 44 Empty the liquid waste container. 45 Empty the bag for the tip waste container and replace if damaged. 46 Inspect the instruments (inner and outer surfaces) and racks for stains and spills. Clean if necessary. VII. Weekly Maintenance Procedure : a) Run the weekly washer maintenance: (Procedure takes approximately 20 min) i. Fill all wash buffer containers with de-ionized water ii. Click ‘New Worklist’ located in the upper toolbar iii. The Set-up panel dialog box will appear iv. In the Set-up Panel dialog box click ‘Add Plate’ v. In the Set-up Panel dialog box click ‘Add Assay’ and then select the file ‘WasherClean BR.asy’, click ‘Open File’. vi. Click ‘OK’ to validate the various dialog boxes until the worklist appears. vii. Click ‘Start’ (green button) viii. Load an empty washer microplate with the metal plate holder onto the analyzer when the Load Plate dialog box appears. Click ‘OK’ after the plate is loaded onto the analyzer. ix. When the run is complete, unload the washer plate and replace the de-ionized water with the appropriate wash buffers. *The weekly washer maintenance does not have to be completed during the week the monthly washer maintenance is being done. b) Decontaminate the pipettor wash station: UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 36 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual i. Pour 5 ml of decontamination solution consisting of 0.4% RIVASCOP (4ml of RIVASCOP into 1L of water) into the pipettor wash station and let it soak for a minimum of 15 minutes. ii. Do not empty, the liquid will drain automatically when the system is initialized. c) Decontaminate and wipe the tip ejection slide. d) Clean the instrument surfaces and work area. VIII. Monthly maintenance Procedure: a. Run the monthly washer maintenance: (Procedure takes approximately 1 hour) i. ii. iii. iv. v. Fill all the wash buffer containers with de-ionized water Click ‘New Worklist’ located in the upper toolbar The Set-up panel dialog box will appear In the Set-up Panel dialog box click ‘Add Plate’ In the Set-up Panel dialog box click ‘Add Assay’ and then select the file ‘WasherManifoldDisinfect BR.asy’, click ‘Open File’ vi. Click ‘OK’ to validate the various dialog boxes until the worklist appears. vii. Click ‘Start’ (green button) viii. The Load dialog box will appear. ix. Pour 50ml of 0.4 % RIVASCOP into two 60ml of container and load the reagents onto a ‘0’ reagent rack. Then load the rack onto the analyzer. x. In the Load dialog box, allocate the bottles to the corresponding rack position in which the container was loaded then click ‘OK’. xi. Load an empty washer microplate with the metal holder onto the analyzer when the Load Plate dialog box appears. Click ‘OK’ after the plate is loaded onto the analyzer. xii. A few minutes later a message saying to ‘open the drawer, unscrew waste bottle 1 and close the drawer’ will appear. xiii. Unscrew the cap to waste bottle 1, which is located behind the wash buffer bottles. Close the drawer when done and click ‘OK’. xiv. After 15 minutes a message prompts you to re-open the drawer and re-screw the cap to waste bottle 1, close the drawer when completed and click ‘OK’. xv. When the run is complete, unload the plate and the reagent rack and replace the de-ionized water with the appropriate wash buffers. b. Decontaminate the sample and reagent racks, plate carrier and tip ejection slide. c. Decontaminate the system liquid container i. Empty the system liquid container. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 37 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual ii. Empty the container and rinse thoroughly, twice with tap water and once with de-ionized water. iii. Inspect the filter (attached to the cap) to see if damaged or in need of replacing. iv. Refill the container with freshly prepared System Liquid. Preparation of System Liquid: 2 ml of Tween 20 to 10L of de-ionized water. d. Clean the washer buffer bottles only and NOT the caps & sensor devices. e. Backup System Files i. Click ‘Backup’ button found at the upper tool bar. ii. The System Backup dialog box will open up. iii. Click ‘Backup System Files’ iv. Once completed, click ‘Close’ from the System Backup dialog box. IX. Assay validation: 1. Substrate Blank Acceptance: The Substrate Blank (A1 well) > = -0.020 and < = 0.05 2. Negative Calibrator Acceptance: Each Negative Control must < = 0.120 and > = -0.005. Negative Calibrator with absorbances between 0.000 and –0.005 are rounded to 0.000 for calculations. If one of the three Negative Calibrators is outside the acceptable range, the calculations are made based on the two acceptable Negative Calibrators. The plate is invalid and should be repeated, if two or more of the Negative Calibrators are unacceptable. 3. Calculate the mean of the Negative Calibrators. 4. Positive Control Acceptance: Both Positive Controls must be > = 0.800. Both Positive Controls must not differ by more than 0.600 5. Cutoff Value Calculations: Cutoff = NCal mean + 0.600 X. Quality Control: All positive controls and negative controls should all within the range as mentioned in the Kit insert. If any control fails, withhold test results. Inform Charge/Senior technologists. Run Virotrol 1 & viroclear monthly/new lot for HBsAg,HIV ½,HBcAb and HCV Ab. Results entered in Non-AXSYM external Control Spreadsheet. Repeat with a new aliquot if Virotrol 1 fails. Inform Charge/Senior technologists. XI. Reporting: UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 38 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 1. Positive: >Cutoff Value 2. Negative: < Cutoff Value 3. All positive specimens will be repeated x 2 on the next run. Sample should be obtained from the original blood tube. 4. All repeats have to be recorded on the EVOLIS REPEATS WORKLIST, and given when complete to the chief LIS officer. 5. Reporting for George Washington 8HCAE 8COM must be ordered after initial 8HCAE result is available 8HCA must be resulted using the following format in the comment-3 architect values must be above the test comment: #.## / #.## / #.## (Test performed using the Architect Anti-HCV assay, device #6C37,Abbott Diagnostics) 1) Initial 8HCAE is Negative LIS Code Result 8HCA Inconclusive 8HCA2 8HCAE 8COM Type two repeated HCA results Negative Note Comment 3 architect values in the comment (e.g.:#.## / #.## / #.##) Verify 8HCA Verify Result Verify 8HCAE In the comment for 8COM, record O.D. results for HCAE and cut off O.D. from initial run Verify 8COM 2) Initial 8HCAE is Positive, both repeated 8HCAE2 are Positive, or Initial 8HCAE is Positive, one repeated 8HCAE2 is positive and on repeated 8HCAE2 is negative LIS Code Result Comment 8HCA Positive 3 architect values in the comment (### / ### / ###) Verify 8HCA 8HCA2 Type two repeated HCA results Verify Result UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 39 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 8HCAE Positive 8HCE2 8COM Positive Note Enter 3 Evolis results as pos/pos/neg Verify 8HCAE Verify 8HCE2 In the comment for 8COM, record 3 O.D. results for HCAE and cut off O.D. from initial and repeat runs Verify 8COM 3) Initial 8HCAE is Positive, both repeated 8HCAE2 are Negative XII. LIS Code 8HCA Result Inconclusive 8HCA2 8HCAE Type two repeated HCA results Negative 8HCE2 8COM Negative Note Comment 3 architect values in the comment (e.g.:### / ### / ###) Verify 8HCA Verify Result Type 3 Evolis results as pos/neg/neg Verify 8HCAE Verify 8HCE2 In the comment for 8COM, record 3 O.D. results for HCAE and cut off O.D. from initial and repeat runs Verify 8COM Troubleshooting Procedures For Flags, Recalculate Results and other procedures please refer to Evolis Short User Manual (Quick guide) Chapter 3: Advanced Information. For more information please refer to Evolis User Manual 1.90 EN (Long Version) If service is needed: Call BioRad Service: 1-800-361-1808 for Evolis problems. Instrument SN: 9163740225 UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 40 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual XIII. Reference Package insert from Ortho®HCV 3.0 ELISA Test System, revised July 2003 EVOLIS™ Short User Manual software version 1.90, revised June 2008 EVOLIS™ User Manual software version 1.90, revised June 2007 UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 41 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Hepatitis Virus Serology Although there are many infectious causes of hepatitis, the majority are caused by hepatitis A, B and C viruses. Acute Hepatitis A is diagnosed by detection of IgM antibodies. Anti-HAV IgM becomes positive just before the development of clinical hepatitis and remains positive for at least 4 months after infection. There is no chronic carrier state for Hepatitis A. Detection of total antibodies to Hepatitis A indicates immunity due to either past infection or immunization. Hepatitis B is diagnosed by either detecting hepatitis B surface antigen (HBsAg) which indicates the presence of infectious virus, (HBcAb-IgM) or Anti-hepatitis B surface antibodies (HBsAb) which indicate immunity due to either past infection or immunization. Anti-hepatitis B core IgM antibodies indicate acute infection and HBcAb-Total indicates previous or current infection. HBsAg should be cleared within 6 months of acute infection. Persistence of HBsAg beyond 6 months is consistent with chronic hepatitis B infection. Some of these tests may occasionally be performed on a STAT basis because of concern regarding transmission of the virus to a susceptible individual following exposure (i.e. needlestick, newborn) to infected blood/body fluids and the need to prevent the disease by administering vaccine and/or immunoglobulin. Hepatitis due to the delta virus is rare in Canada. It only occurs in association with patients who are positive for hepatitis B surface antigen. Requests for this virus should be forwarded to the Public Health Laboratory. Hepatitis C (HCV) is a blood borne virus closely associated with blood transfusion and intravenous drug use. The presence of antibodies to HCV indicates that an individual may have been infected with HCV, may harbour infectious HCV and\or may be capable of transmitting HCV infection. The following requests will be handled in our laboratory: Hepatitis B surface antigen HBsAg Hepatitis B surface antibody HBsAb Hepatitis B core antibody HBcAb Hepatitis B e antigen HBeAg1 Hepatitis B e antibody HBeAb1 Hepatitis C antibody HCA Hepatitis A IgM antibody HAV-IgM2 Hepatitis A Total antibody HAV-IgG Note: 1) These tests will be performed on request only if the patient is HBsAg positive. 2) Perform only HAV-IgM if type of Hepatitis A test is not specified. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 42 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Table 1. Tests performed as per designated categories Clinical Category Hepatitis B Screen Hepatitis A Screen Hepatitis B Immune Status Needlestick - Patient (source) - Staff (exposed) Pre/postnatal - Mother Hepatitis Screen HBsAg X Test Performed HBsAb HAV-IgM HCVAb X X X X X X X X X X For additional requests within the above categories, consult with the charge technologist or medical microbiologist. In the absence of one of the above clinical categories, do the tests as requested. Table 2. Guidelines for STAT Testing Clinical setting Serum tested Time frame from exposure to report Days of week Callback Neonate Prenatal Needlestick/ mucosal exposure2 Renal dialysis Mother Mother See below < 12 hours < 12 hours < 72 hours All All All No1 No1 No1 Patient < 12 hours All No1 1) May require call back on weekends if time from exposure to reporting exceeds 12 hours. Must be approved by microbiologist on-call. 2) Perform HBsAg and HCVAb on the source. Test HBsAb and HCVAb on the employee. Whichever of these arrives first is to be tested STAT. If both arrive at the same time, test both simultaneously. If the source HBsAg is positive, test the employee STAT. If the source is negative, test employee in the next routine run. Labor Delivery Stat HIV HBsAg Instructions UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 43 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Aspergillus Galactomannan Antigen Detection Assay I. Introduction The PlateliaTM Aspergillus EIA is a qualitative enzyme immunoassay for the detection of Aspergillus galactomannan antigen in serum and Bronchoalveolar Lavage (BAL) samples. II. Specimen Collection and Processing The test is performed on serum and BAL samples. Blood is collected in a serum separator tube and separated by centrifugation at 3000 rpm for 10 minutes. After initial opening, samples may be stored at 2-8oC for up to 48 hours prior to testing. For longer storage, store the serum at -70oC. III. Instrument EVOLIS ™ Analyzer IV. Reagents BioRad Aspergillus Galactomannan kit: 1. Galactomannan monoclonal antibodies coated microwell plate 2. Concentrated wash solution (10X) 3. Negative control serum (Human) Cut-off control serum (Human) Positive control serum (Human) !The controls must be heat-treated with the Sample Treatment Solution as patient specimens, in order to also be a monitor of the treatment 4. Conjugate – Anti-galactomannan monoclonal antibody/ peroxidase labeled 5. Sample Treatment Solution (EDTA acid solution) 6. TMB substrate buffer 7. Chromogen TMB solution 8. Stopping solution – 1.5N sulphuric acid UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 44 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual V. Preparation for Procedure 7. Before beginning EIA assay, fill up Galactomannan BioRad Wash containers when necessary: *Working Galactomannan Wash buffer: Add 50 ml of 20x BioRad wash solution to 950 ml of distilled water. Fill up Galactomannan wash container with black tubing 8. De-ionized Water: Fill up Evolis blue, yellow and red tubing container with de-ionized water 9. Working TMB substrates are prepared fresh for each run in a 30ml EVOLIS vial. 10. The Aspergillus Galactomannan conjugate and stopping solution will be pipetted from their original containers and can be loaded onto the analyzer as is. 11. Bring all required microwell strips and the reagents mentioned above to room temperature before use. 12. Empty the waste tank and check the system liquid container (refill if necessary). System Liquid Preparation: 2ml of Tween 20 to 10L of de-ionized water. VI. Treatment of the serum/BAL Fluid Serum and BAL samples need to be heat-treated in the presence of EDTA prior to being tested on the analyzer. This pre-analytical procedure helps dissociate immune complexes and causes serum proteins to precipitate which can possibly interfere with the testing procedure. All control sera: negative, cut-off and positive must be processed at the same time and in the same manner as the patient samples: 1. Label 2 empty 2ml sample tubes. One tube must labelled with the patient barcode label. For the control samples label 2 empty tubes for each: Neg, Cut-Off & Pos, respectively. *The Cut-Off Control will be sampled twice by analyzer but only one sample tube needs to be prepared. 2. Pipette 390ul of each test serum/BAL or control into one of the 2 ml sample tubes. 3. Add 130ul of serum treatment solution into the sample tube. 4. Tightly close the caps of the tubes to prevent opening during heating. 5. Mix tubes thoroughly by vortexing each sample. 6. Heat the sample tubes by placing them in a heating block at 120oC for 6 minutes. Tubes must be placed in the block only when the prescribed temperature is reached. 7. Carefully remove the heated tubes from the heating block after 6 minutes and place them in the centrifuge. Centrifuge tubes at 10,000 x g for 10 minutes. The supernatant is used for the detection of the galactomannan antigen. 8. Transfer 300ul of supernatant into the second labeled 2ml sample tube which has patient’s bar code and will be placed on to the EvolisTM analyzer. 9. After preparation, the supernatant may be removed and stored at 2-8 oC for up to 48 hours prior to testing. If analysis of the results indicates that retesting of a sample is required, another aliquot of the serum or BAL must be heat treated for retesting. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 45 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual VII. Procedure 1. Log onto the system by clicking on “OK”, no password is required. 2. A self-test of the system is automatically initialized each time the EVOLIS software is run. The self-test is considered satisfactory if the word “PASSED” appears beside each instrument module. Print a copy of the self-test report and combine it with the work list and result sheets. 3. Prepare specimens by removing the lids off the heat-treated serum/BAL supernatant and load all sample tubes with the barcode facing right on to the sample rack (rack code T). Check the quality of the samples by ensuring all clots, foam and bubbles have been removed. 4. Open the door to the sample and reagent unit. Load the sample rack with the bar-codes facing the bar-code reader onto the track marked by the solid red LED light. 5. The ‘Patient Editor’ dialog box will appear with the specimen numbers from the loaded rack. Double check that the specimen numbers are correct. If there is a blank space under the patient ID column, click on the space and enter the specimen number manually. All specimen numbers entered manually will be flagged with the code “ManID” on the results report. 6. Choose the Galactomannan assay from the drop down menu which appears along the top of the Patient Editor dialog box: Galactomannan assay = “MT SINAI Aspergillus EIA New BR V1” 7. Click on the assay box corresponding to the sample number if you want that assay to be run for that sample. A check mark is shown for a sample where the assay has been selected. 8. Once the required assay has been selected for each sample click ‘Close’ to save. A solid LED light will show up for the next available track in the sample and reagent unit which indicates where the next sample rack can be loaded. Repeat steps 6 to 11 for each new sample rack that is loaded on to the analyzer. 9. A total of four sample racks need to be loaded on to the analyzer even if all the sample racks are not required in order for the reagent template to be used in a later step. When an empty sample rack is loaded on to the analyzer just click ‘Close’ when the Patient Editor dialog box appears. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 46 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 10. To check and validate the worklist click on the ‘New Worklist’ icon located on the upper toolbar and the Set-Up dialog box will appear. 11. Click on “+” beside the assay file name that is associated with the plate. The plate layout will appear at the right hand side of the dialog box and will show the total number of controls and specimens to be tested, their assigned wells and the number of strips required for the assay. 12. If duplicate samples need to be tested for a given assay in the same run: a) From the Patient Editor dialog box select the assay folder in which the duplicate sample needs to be run and click ‘Add Patient’. b) The Select Patient(s) dialog box will appear. c) Check the Allow multiple determinations box which appears at the bottom of the Select Patient|(s) dialog box. d) The patient sample IDs will appear. Click on the sample ID in which multiple testing is required and click OK. e) In the Set-up Panel dialog box, a (x2) will appear beside the patient ID under the assay folder in which it was selected. 13. If all the information is correct click ‘OK’ to validate the worklist. 14. A separate dialog box asking for the reagent lot number will appear for each assay that is ordered. Double check the lot number and expiry date and click ‘OK’ if everything is correct. 15. Click on the “+” to expand the Work folder and click on ‘Plate Layout’, the number of microwell strips required for the assay can be reviewed. Click the ‘Print’ button located along the top of the toolbar to print the plate layout if desired. 16. Click ‘START’ (green button) located on the upper tool bar to open the Load dialog box. 17. The Load dialog box appears and shows where to load all the required resources. 18. Load all required resources from left to right: i. Pipette tips: Grey = 1100 ul tips (full rack) Brown= 300 ul tips (full rack) Red = Incomplete tip rack *The pipette tips have to be loaded in the exact position as shown in the layout ii. Load the assay reagents on the reagent racks according to the following templates (Figure 1). The reagent template specific for the Aspergillus Galactomannan assay should be used. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 47 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual iii. Ensure all caps on the reagent/control containers have been removed before loading them onto the analyzer. TMB Substrate preparation for Aspergillus Galactomannan assay (prepare in 30ml coated vial): Prepare Fresh (Same Day) Working Chromogen as follows (always make 1 extra strip): Number of Strips Chromogen Reagent (uL) Chromogen Diluent (mL) 1 2 3 4 5 40 80 120 160 200 2.0 4.0 6.0 8.0 10.0 UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 48 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Figure 1 Once all the reagents and controls have been added to the racks, load the reagent racks onto the sample and reagent unit in the following order: 1st =‘0’- Large reagent rack 2nd=‘3’- Small reagent rack iv. In the Load dialog box, click the ‘Open Reagent Layout’ button. Select the file name ‘galactomannan.rea’ and click ‘Open’. All reagents and controls will be automatically allocated to their assign position. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 49 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 19. Once all the required resources have been loaded onto the analyzer click ‘OK’ and the Load dialog box will disappear. The analyzer will begin to check the resources to ensure their amounts are sufficient. 20. The Load Plate dialog box will then appear. Rename the plate ID with the corresponding assay name, for example Galactomannan. The test date will automatically be added to the plate ID by the analyzer. 21. Prepare the required number of microwell strips for the requested assay. The number of strips required is shown in the Plate Layout which is found on the right hand side of the Load Plate dialog box. 22. Insert the microplate into the metal frame microplate holder. Make sure that the A1 position of the plate and holder match. 23. Open the door to the microplate loading compartment and load the microplate and its holder onto the plate transport unit. Once loaded, close the door to the microplate loading compartment. 24. Once the plate is loaded click ‘OK’. After the microplate is loaded, the analyzer will start to run automatically. 25. From the Work folder click on ‘Schedule’ to view the chorological order and completion time of the run. 26. While the samples are being pipetted click on ‘Active Event Log’ to ensure that all samples were pipetted successfully. Look for any red flags that may appear in the “Dispense Sample” section which indicates that an error has occurred. The analyzer will pause and flag with an error message if a clot or low sample volume is encountered, allowing for operator intervention. 27. The results report will automatically print out after the assay is completed. 28. Once the assay is finished a dialog box prompting the removable of the test plate and carrier from the analyzer will appear. 29. Open the door to the microplate loading compartment and remove the microplate. After the microplate is unloaded close the door to the microplate loading compartment and click ‘OK’. 30. A blinking red LED light in the sample and reagent unit indicates that the reagent or sample racks can be unloaded from the analyzer. 31. Do not unload pipette tip racks from the analyzer unless they are completely empty. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 50 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 32. Close the EVOLIS software. Select File | Exit from the menu bar or click the X icon at the top right-hand corner of the Evolis software and shut down the computer. 33. Switch off the Evolis analyzer. 34. Open the instrument cover and wipe the tip adapter (pipettor head) with 70% Ethanol wipes. 35. Empty the liquid waste container. 36. Empty the bag for the tip waste container and replace if damaged. 37. Inspect the instruments (inner and outer surfaces) and racks for stains and spills. Clean if necessary. VIII. Weekly Maintenance Procedure : 1. Run the weekly washer maintenance: (Procedure takes approximately 20 min) Fill all wash buffer containers with de-ionized water Click ‘New Worklist’ located in the upper toolbar The Set-up panel dialog box will appear In the Set-up Panel dialog box click ‘Add Plate’ In the Set-up Panel dialog box click ‘Add Assay’ and then select the file ‘WasherClean BR.asy’, click ‘Open File’. Click ‘OK’ to validate the various dialog boxes until the worklist appears. Click ‘Start’ (green button) Load an empty washer microplate with the metal plate holder onto the analyzer when the Load Plate dialog box appears. Click ‘OK’ after the plate is loaded onto the analyzer. When the run is complete, unload the washer plate and replace the deionized water with the appropriate wash buffers. *The weekly washer maintenance does not have to be completed during the week the monthly washer maintenance is being done. 2. Decontaminate the pipettor wash station: Pour 5 ml of decontamination solution consisting of 0.4% RIVASCOP (4ml of RIVASCOP into 1L of water) into the pipettor wash station and let it soak for a minimum of 15 minutes. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 51 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Do not empty, the liquid will drain automatically when the system is initialized. 3. Decontaminate and wipe the tip ejection slide. 4. Clean the instrument surfaces and work area. IX. Monthly maintenance Procedure: 1. Run the monthly washer maintenance: (Procedure takes approximately 1 hour) Fill all the wash buffer containers with de-ionized water Click ‘New Worklist’ located in the upper toolbar The Set-up panel dialog box will appear In the Set-up Panel dialog box click ‘Add Plate’ In the Set-up Panel dialog box click ‘Add Assay’ and then select the file ‘WasherManifoldDisinfect BR.asy’, click ‘Open File’ Click ‘OK’ to validate the various dialog boxes until the worklist appears. Click ‘Start’ (green button) The Load dialog box will appear. Pour 50ml of 0.4 % RIVASCOP into a 60ml of container and load the reagent onto a ‘0’ reagent rack. Then load the rack onto the analyzer. In the Load dialog box, allocate the bottle to the corresponding rack position in which the container was loaded then click ‘OK’. Load an empty washer microplate with the metal holder onto the analyzer when the Load Plate dialog box appears. Click ‘OK’ after the plate is loaded onto the analyzer. A few minutes later a message saying to ‘open the drawer, unscrew waste bottle 1 and close the drawer’ will appear. Unscrew the cap to waste bottle 1, which is located behind the wash buffer bottles. Close the drawer when done and click ‘OK’. After 15 minutes a message prompts you to re-open the drawer and re-screw the cap to waste bottle 1, close the drawer when completed and click ‘OK’. When the run is complete, unload the plate and the reagent rack and replace the de-ionized water with the appropriate wash buffers. 2. Decontaminate the sample and reagent racks, plate carrier and tip ejection slide. 3. Decontaminate the system liquid container Empty the system liquid container. Empty the container and rinse thoroughly, twice with tap water and once with de-ionized water. Inspect the filter (attached to the cap) to see if damaged or in need of replacing. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 52 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Refill the container with freshly prepared System Liquid. Preparation of System Liquid: 2 ml of Tween 20 to 10L of de-ionized water. 4. Clean the washer buffer bottles only and NOT the caps & sensor devices. 5. Backup System Files Click ‘Backup’ button found at the upper tool bar. The System Backup dialog box will open up. Click ‘Backup System Files’ Once completed, click ‘Close’ from the System Backup dialog box. X. Quality Control Procedures 1. Calculate the mean absorbance of the Cut-Off Control (Cut-Off X): Sum of the O.D values for the two Cut-Off controls divided by 2. The O.D of each Cut-Off control must be ≥0.3000 and ≤0.8000 to be considered valid. 2. Calculate the Negative Control Index by dividing the O.D of the Negative Control by the mean absorbance of the Cut-Off Control. Negative Control Index = O.D Negative Control Mean Cut-off Control O.D The index of the Negative Control Serum must be less than 0.40 to be considered valid. 3. Calculate the Positive Control Index by dividing the O.D of the Positive Control by the mean absorbance of the Cut-Off Control. Positive Control Index= O.D Positive Control Mean Cut-off Control O.D The index of the Positive Control Serum must be greater than 2.00 to be considered valid. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 53 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual XI. Reporting: 1. The presence or absence of galactomannan antigen in the test sample is determined by the calculation of an index for each patient sample. To calculate the Index of a sample, divide the O.D of the patient sample by the mean O.D of the cut-off control. Patient Serum/BAL Index = Patient Sample O.D. Mean Cut-off Control O.D 2. Patient serums/BAL with an index < 0.50 is considered to be negative for galactomannan antigen. 3. Patient serums/BAL with an index ≥ 0.50 is considered to be positive for galactomannan antigen. 4. For patient serums/BAL O.D.=9.0000 [OD>3.50] a. calculate the index for OD=3.50 : 3.50 Mean Cut-off Control O.D b. Report patient’s index > the index of OD=3.50 See Evolis EIA Worksheet for calculations 6. All positive specimens will be heat-treated and repeated x2 on the next run. 7. All repeats have to be recorder in EVOLIS REPEATS WORKLIST, and give the filled-up worklist to ED 8. An absorbance value of less than 0.000 may indicate a procedure or instrument error and the result is considered invalid and the specimen should be re-run. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 54 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 9. Rules for reporting Index≥0.5 Facility Index 0.5≤Index≤1.0 Initial Reporting 1. Order 8COM 2. Result 8COM:type initial index value 3. Order 8GAL1 and verify 4. Order 8GAL2 and verify UHN Index>1.0 1. 8GAL:Positive Report index in the comment: (Index Values: #.##) *Preliminary testing POSITIVE, to be repeated. 2. Verify 8GAL result 3. Order 8GAL1 and verify 3. Order 8GAL2 and verify Non- UHN XII. Index ≥0.5 2 of 3 results are positive 8GAL:Positive Report 3 index in the comment: (Index Values: #.##/#.##/#.##) 2 of 3 results are Negative 8GAL:Negative Report 3 index in the comment: (Index Values: #.##/#.##/#.##) 2 of 3 results are positive 8GAL:Positive Report 3 index in the comment: (Index Values: #.##/#.##/#.##) 2 of 3 results are Negative 8GAL:Negative Report 3 index in the comment: (Index Values: #.##/#.##/#.##) 2 of 3 results are positive 8GAL:Positive Report 3 index in the comment: (Index Values: #.##/#.##/#.##) 2 of 3 results are Negative 8GAL:Negative Report 3 index in the comment: (Index Values: #.##/#.##/#.##) Trouble shooting: UHN/NON-UHN XIII. 1.Order 8COM 2.Result 8COM:type initial index value 3.Order 8GAL1 and verify 4.Order 8GAL2 and verify After repeat in duplicate No index, but has the following error: P_max_high P_min_low P_stop_high P_static_high P_static_high P_mean_low 1.Order 8COM 2.Result 8COM:type the error 3.Order 8GAL1 and verify Only needs to be repeat once Report according the result! Reference: Package insert from Platelia Aspergillus EIA Revised July 2007 EVOLIS™ Short User Manual software version 1.90, revised June 2008 EVOLIS™ User Manual software version 1.90, revised June 2000 UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 55 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Infectious Mononucleosis Heterophile Antibodies I. Introduction The MONOSPOT LATEX slide test is a latex particle agglutination test for in vitro qualitative detection of infectious mononucleosis heterophile antibodies (IgM) in serum or plasma. These antibodies appear in the sera of 85 to 90% of patients with infectious mononucleosis within 2 to 3 weeks after onset of illness. II. Specimen Collection and Processing 5 mL of blood is collected in a serum separator tube and separated by centrifugation. The tube is refrigerated until testing. Specimens are stored at -200C after testing and discarded after 3 months. III. Procedure i) Reagents: MONOSPOT LATEX Kit: Store refrigerated. Allow the reagent to warm up to RT. Mix well before use. ii) Other Materials: Supplied with kit: Test slides Paddle pipettes iii) Method: 1. Dispense 1 drop of the latex reagent onto a labelled oval ring of the test card. 2. Add 1 drop (50 L) of patients's serum or control to the same ring. 3. Mix the latex reagent and serum together and spread to cover the entire area of the ring with the blade end of the paddle pipette. 4. Immediately rotate the card on the serologic rotator at 100 rpm for 3 minutes. 5. Observe for agglutination using a light source to aid in visualization. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 56 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual iv) Interpretation of Results: IV. V. Negative: No agglutination Positive: Any degree of agglutination Reporting Positive Report: "Infectious mononucleosis heterophile antibody: POSITIVE" Negative Report: "Infectious mononucleosis heterophile antibody: NEGATIVE" Quality Control Negative and positive controls must be included with each run and results and kit lot number recorded on the tasklist. When opening a new kit, record the lot number in the reagent lot number binder. Refer to a senior technologist if control results are outside of limits or for any other problems with running or reporting the assay. Run external control ( Accurrun 31) with each new lot. Result filed in Reagent Lot Binder. . If result is negative, inform Charge/senior technologist for review. CAP provides external proficiency testing. VI. References Manufacturer's package insert: Meridian Diagnostics, Inc., 3471 River Hills Dr., Cincinnati, Ohio 45244 U.S.A. 1-513-271-3700. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 57 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Pneumocystis jiroveci (previously known as P. carinii) DFA TEST I. Introduction The Merifluor-Pneumocystis DFA test is an in vitro test for the direct detection of Pneumocystis carini cysts and trophozoites in bronchoalveolar lavage (BAL), bronchial wash (BW); sputum or biopsy specimen. II. Collection and Transport BAL, wash and sputum should be collected using standard procedures. Biopsy specimens e.g. transbronchial, open lung or others must not be fixed and are transported to the lab on a saline moistened piece of gauze in a sterile container. Tissue should not be allowed to dry or become immersed in saline. All specimens should be transported as soon as possible to the laboratory. PCP testing can be done on the day after receipt except specimens received Friday or the day before a holiday must be stained and read that day. III. Procedure Reagents FITC- P. carinii conjugate Control slides Distilled water FA mounting fluid Sputolysin: diluted 1:10 (i.e. 300 Ul sputolysin 3.0 mL distilled water) Materials Vortex Sterile pipettes 10 - 100 uL Eppendorf pipette Humidified chamber Coplin jars Fluorescent microscope UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 58 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Preparation of Slides BAL and BW: 1. Centrifuge the BAL or BW for 10 minutes at 1800 x g. 2. Remove and discard all but 0.5 mL of the supernatant. Thoroughly resuspend the pellet in the remaining 0.5 mL of fluid. 3. Make a thin smear twice the size of a cytospin spot and allow to air dry. 4. Fix in acetone for 5 minutes in a coplin jar, then air dry. 5. Slide must be stained within 8 hours or freeze at -200C. Sputum - See Sputolysin Procedure 1. Combine equal volumes (3 mL each) of sputum and diluted sputolysin. Vortex mixture. 2. Incubate for 3 minutes at 350C. 3. Vortex the mixture briefly and add an equal volume of PBS and entrifuge at 1300 x g for 5 minutes. 4. Remove the supernatant, leaving 0.5 mL to resuspend the pellet. 5. Make a smear twice the size of a cytospin spot. Allow to air dry. 6. Fix in acetone for 5 minutes in a coplin jar, then air dry. 7. Slide must be stained within 8 hours or freeze at -200C. Biopsy Specimen 1. Prepare a freshly cut surface on a fragment of tissue. 2. Touch the cut surface to a FA slide. Make several non-overlapping imprints within the well, avoiding smearing using several cuts. 3. While imprints are still moist on the slide, fix by adding 1 - 2 drops of acetone and allow to air dry. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 59 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 4. Slide must be stained within 8 hours or freeze at -200C. Staining - DFA 1. Cover the smear with 30 uL of P. carinii FITC-conjugate antibody. 2. Incubate in a humidified chamber for 30 minutes at 360C. 3. Wash slide twice with distilled water for 2 minutes in a coplin jar. 4. Allow the slide to dry. 5. Mount using coverslip and mounting fluid. 6. Read with fluorescence microscope with the FITC / Evans Blue filter and 40x objective. Interpretation of Results POSITIVE: Any specimen which contains two typical cysts exhibiting apple-green fluorescence of characteristic morphology. Generally cysts, 5 - 8 um diameter, are found together with trophozoites in clusters. Clusters can be variable in size and may appear with or without "honeycomb" like structure. Some cysts fluoresce evenly throughout their structure whereas other cysts may fluoresce mainly on their periphery and produce a "honeycomb" appearance within the clusters. NEGATIVE: Red fluorescence without any characteristic apple-green fluorescence as described above. IV. Reporting POSITIVE: "Pneumocystis jiroveci (previously known as P. carinii) positive by immunofluorescence". NEGATIVE: "Pneumocystis (previously known as P. carinii) negative by immunofluorescence". Telephone all positive results and document. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 60 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual V. Quality Controls Positive and negative control slides should be stained each time the staining procedure is performed. Refer to a senior technologist if controls do not work or for any other problems with staining, reading or reporting results. External QC (slides from a source other than the reagent supplier or the daily QC) should be done on new reagent lots and if the batch (daily) QC fails. Check Calcoflour stain result in the LIS for concordance and notify the Mycology section as well as Senior/Charge if their result is different. Appropriate actions should be taken to reconcile the difference. VI. Reference 1. Merifluor Pneumocystis, Meridian Diagnostics, Inc. 3471 River Hills Drive, Cincinnati, Ohio, 45244. Tel. 513-271-3700. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 61 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Syphilis Screening I. Introduction The Rapid Plasma Reagin (RPR) Card test is a macroscopic non-treponemal flocculation test used to detect reagin antibodies. II. Specimen Collection and Processing Blood is collected (5 mL for adult and 1 mL for neonate) in a serum separator tube and separated by centrifugation. The serum is removed to a tube and refrigerated until testing. Specimens are stored in the refrigerator for 3 months after testing. A request for VDRL on spinal fluid (CSF) or neonate blood will be sent to PHL for testing. Note: The RPR assay must be used for syphilis testing on cadaveric donor specimens. III. Procedure i) Reagents: RPR reagent kit (Pulse Scientific Inc.) ii) Other Materials: 3 mL dropper bottle Dispensing needle (17 L/drop) RPR test card 0.05 mL disposable stirrer pipettes Serological rotator at 100 rpm dH2O iii) Precaution: Refrigerate reagents until required. Warm to RT and mix well before use. To ensure stability, return the antigen suspension to the original glass bottle after testing. The dispenser and needle assembly must be thoroughly washed in dH2O and air dried after use. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 62 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual iv) Needle Accuracy Check - When New Kit Opened: This procedure is performed to check the needle delivering antigen each time before testing. Using a pipette, deliver 0.5 mL antigen to the dropper bottle. Attach the needle and, holding in a vertical position, count the number of drops delivered in 0.5 mL. The needle is considered satisfactory if 30 1 drops are obtained. If the needle is unsatisfactory, repeat the check. Record the lot number of the newly opened kit in the reagent lot number binder. v) Method: 1. Using the stirrer pipette held vertically, dispense one drop (50 L) of serum onto a circle on the test card. Use a fresh stirrer pipette for each sample. Repeat with the control sera. 2. Using the flat end of the stirrer pipette spread the sample over the entire area of the test circle. 3. Attach the needle to the dropper bottle. Mix the carbon antigen reagent well. Squeeze the dropper bottle and withdraw sufficient reagent into the bottle. Discard the first few drops into the reagent stock bottle and then dispense 1 drop into each circle in a vertical position. Do not mix the sample and the antigen. Rotate the card at 100 rpm for 8 minutes. 4. Observe for agglutination by two technologists independently. vi) Interpretation of Results: Positive Result: Any agglutination. Repeat test ---- see senior technologist for any discrepant results. Send all positive sera to PHL for VDRL and confirmatory tests. Write on PHL requisition: "RPR positive, please do confirmatory test"; DO NOT mark prenatal box for serum from prenatal patients. Negative Result: No agglutination. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 63 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual IV. V. Reporting Positive Result: Enter in LIS as "TO PHL". VDRL send-out test is ordered reflexively. Send to PHL next day. Negative Result: Negative Quality Control Strongly reactive, weakly reactive and non-reactive control sera are included in each run. If controls are not working or the antigen is not falling cleanly from the needle, perform a needle check as outlined in the method. Record control results and kit lot number on the task list. Run external control (Accurun 156) with each new lot. When opening a new kit, record the lot number, needle check and external control results in the reagent lot binder. Refer to a senior technologist if control results are outside of limits or for other problems with running or reporting the assay. CAP provides external proficiency testing. VI. Reference Manufacturer's package inserts (RPR Card Test, Pulse Scientific Inc., 18-5100 South Service Road, Burlington, ON L7L 5H4 (905) 333-8188). UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 64 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Varicella-Zoster Virus IgG I. Introduction Varicella-Zoster IgG assays is used for evaluating patient's immune status to Varicella-Zoster viruses infection. The VIDAS is an enzyme-linked fluorescent immunoassay (ELFA) utilizing a virus coated Solid-Phase-Receptacle (SPR) to which antibody in serum binds. Anti-Human IgG conjugated with Alkaline Phosphatase reacts with substrate, 4-Methylumbelliferyl Phosphate to form a fluorescent product. All necessary reagents and test serum are contained in the VZG reagent strips. II. Specimen Collection and Processing Blood (5 mL) is collected in a serum separator tube and separated by centrifugation. The serum is removed to a vial and refrigerated until testing. Specimens are stored at -20oC after testing. III. Procedure Reagents VIDAS Varicella-Zoster IgG test kit: VZG Reagent Strips VZG SPRs Standard Positive Control Negative Control Other materials: Pipettor 100 uL UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 65 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Method 1. Bring test kit and serum samples to room temperature. Check that lot number of kit matches lot currently in use (as posted on VIDAS instrument). If lot number does not match, ensure that all kits/test strips for the posted lot number have been used. Enter new lot data by inserting bar code card found in kit into tray, load tray into Section ‘A’. Press ‘Master Lot Menu’,’ Read Master Lot’ and section ‘A’. The machine will move the tray and read the card. At the end, press ‘Master Lot Menu’, use ↓ to ‘List Master Lot’. Press that button, and also ‘VZG’, will show three lots #. Check that one of these includes the new lot. Post card of new lot currently in use on VIDAS along with the date. 2. Label MSG/VZG strips as follows: s (Standard) s (Standard) C1 (Positive Control) C2 (Negative Control) 5 6 etc. up to 30 3. Pipette 100 uL of Standard, Control or serum into the specimen well of the corresponding VZG strips. Check for adequate sample level and remove any bubbles. 4. At VIDAS instrument, start at Main Menu. To program a run with Standards( Alarm will alert the expiration of standards): a. Load strips(containing 100 ul of each standards, controls, or samples) and tips into Mini Vidas. b. Press ‘Status Screen”- will show ‘A’ and ‘B’ available. c. Press ‘A’. d. Section ‘A’ appears with 1,2,3,4,5,6. e. Press’1’(Position 1), then press ‘S’ for Standard. f. Standard number (1-4) appears, press ‘1’,will show ‘S1’,’Enter’. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 66 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual g. Press ‘2’(position 2), then press ‘S’ for Standard. h. Standard number (1-4) appears, press ‘1’ (not 2) ,will show ‘S1’,’Enter’. i. .Press ‘3’ (position 3), then press ‘C’ for Control. j. Control number (1-4) will appear, press ‘1’, will show ‘C1’,’Enter’. k. Press ‘4’ (position 4), then press ‘C’ for Control. l. Control number (1-4) will appear, press ‘2’, will show ‘C2’,’Enter’. m. Press ‘5’ (position 5), then press ‘Sample ID’. n. Use arrow to move cursor to ‘D’, press button connected to that line (Last button).Then press # on the keyboard to enter all the numbers.’ Enter’. o. Press ‘6 (position 6), then press ‘Sample ID’. p. Use arrow to move cursor to ‘D’, press button connected to that line (Last button).Then press # on the keyboard to enter all the numbers.’ Enter’. q. Press ‘Start’. Once check has been completed and ‘OK’, green light will stay on, and screen will show the time the testing will be finished. r. Press ’B’ for next module. s. Press ‘1 (position 1), then press ‘Sample ID’. t. Use arrow to move cursor to ‘D’, press button connected to that line (Last button).Then press # on the keyboard to enter all the numbers.’ Enter’. u. Do the same for the rest of the positions. v. Press ‘Start’. Once check has been completed and ‘OK’, green light will stay on, and screen will show the time the testing will be finished. w. Once the testing is finished,’ Unload’ will appear. Unload strips and tips. Check strips that show ‘NEGATIVE’ for inoculums. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 67 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual To program a run with without Standard: a. Load strips (containing 100 ul of each controls, or samples) and tips into Mini Vidas. b. Press ‘Status Screen”- will show ‘A’ and ‘B’ available. c. Press ‘A’. d. Section ‘A’ appears with 1, 2, 3, 4, 5, 6. e. Press ‘1’(position 1), then press ‘C’ for Control. f. Control number (1-4) will appear, press ‘1’, will show ‘C1’,’Enter’. g. Press ‘2’ (position 2), then press ‘C’ for Control. h. Control number (1-4) will appear, press ‘2’, will show ‘C2’,’Enter’. i. Press ‘3’ (position 3), then press ‘Sample ID’. j. Use arrow to move cursor to ‘D’, press button connected to that line (Last button). Then press # on the keyboard to enter all the numbers.’ Enter’. k. Do the same for the rest of the positions. l. Press ‘Start’. Once check has been completed and ‘OK’, green light will stay on, and screen will show the time the testing will be finished. m. Press ’B’ for next module. n. Press ‘1 (position 1), then press ‘Sample ID’. o. Use arrow to move cursor to ‘D’, press button connected to that line (Last button).Then press # on the keyboard to enter all the numbers.’ Enter’. p. Do the same for the rest of the positions. q. Press ‘Start’. Once check has been completed and ‘OK’, green light will stay on, and screen will show the time the testing will be finished. r. Once the testing is finished,’ Unload’ will appear. Unload strips and tips. Check strips that show ‘NEGATIVE’ for inoculums. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 68 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Interpretation of Results Specimens with test values greater than 0.9 (MEA/VZ) are considered positive. Test values ranging from 0.6-0.9 are equivocal. Samples with test values less than 0.6 (MEA/VZ) are considered negative. IV. V. Reporting Positive: Varicella-Zoster antibody: Positive Equivocal: Varicella-Zoster antibody: Equivocal Negative: Varicella-Zoster antibody: Negative Quality Control Standard: RFV must be greater than or equal to RFV range posted on VIDAS instrument. Positive and Negative Control: Test Values must be within ranges posted on VIDAS. Quality Control ranges posted on VIDAS may change from lot to lot, therefore it is essential that the lot number of the test kit in use corresponds to that of the posted values. Refer to a senior technologist if control results are outside of limits or for any other problems with running or reporting the assay. Run external control (pooled positive sera) with each new lot. Results filed in Reagent Lot Binder. If result is negative, the run is invalid. Inform Charge/senior technologist, and repeat testing. CAP provides external proficiency testing. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 69 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Monthly: Run QCV : 1. Press ‘Status Screen’. 2. Press section‘A’. 3. Press position ‘1’. 4. Press ‘Assay’ and ‘Select Assay’. 5. Press ‘QCV’. 6. Press ‘Enter’. 7. Press position ‘2’, will show’QCV’ on screen, ‘Enter’. 8. Repeat step # 7 for positon 3-6. 9. Load 6 strips and tips from ‘QCV kit’. 10. Press ‘Start’. 11. Repeat step 1 to 9 for Section ‘B’. 12. Check values: TV1 >= value stated on box R3 >= 4100 RFU 13. Staple print out sheets and file in MiniVidas binder, initial ‘Monthly QC’. Clean Lens: 1. Open the left side of section A where tips are loaded all the way down. 2. Use device provided from Vidas to get rid of any dust on the lens by pumping air onto the lens. VI. Reference Manufacturer's Package Insert. MINI-VIDAS System Operational Manual. bioMerieux-Vitek, Inc. Missouri, USA 64042-2395 UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 70 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Appendix I - Serology Test Schedule EBV VCA IgG ............................................................................................................................ Daily EBV EBNA-1 ........................................................................................................................... Weekly Galactomanan ....... Set up Tuesday & Thursday evening; resulted Wednesday & Thursday morning HBsAg ........................................................................................................................................... daily HBsAg confirmation ........................................................................................................ when needed HBsAb ........................................................................................................................................... daily HBcAb-Total ................................................................................................................................. daily HBcAb-IgM ................................................................................................................................... daily HAV-IgG ....................................................................................................................................... daily HAV-IgM ...................................................................................................................................... daily HBeAg / HBeAb .......................................................................................................................... .daily Monospot IM heterophile Ab ........................................................................................................ daily Rubella Ab ..................................................................................................................................... daily Varicella-Zoster Ab .................................................................................................. STAT or Tuesday RPR for Syphilis ............................................................................................................. STAT or daily HCV Ab ......................................................................................................................................... daily CMV IgG Ab ................................................................................................................................ daily CMV Total Ab(Immucor) ............................................................................................................. daily HIV Ab .......................................................................................................................................... daily HTLV Ab....................................................................................................................................... daily Syphilis TP AB (cmia) .................................................................................................................. daily * Stat testing may be required where clinically justified. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Page 71 of 116 Policy # MI/SER/v48 Microbiology Department Policy & Procedure Manual Section: Serology Manual Appendix II - List of Tests Referred Out to Other Laboratories TEST REQUISITION PHL General DESTINATION 1. Amoebic serology Serology PHL 2. Aspergillus precipitins PHL General Serology PHL 3. Avian precipitins HICL label/requisition Specify bird in question Hospital In-Comm Lab 1 William Morgan Dr. Toronto, Ontario M4H 1N6 Tel. (416) 422-3000 4. Chlamydial culture* PHL General Virology PHL 5. Diphtheria antitoxin toxin Reference Bacteriology 6. Fungal antibodies PHL General Special Bacteriology PHL Serology PHL 7. Malaria PHL General Parasitology PHL 8. Mycoplasma PCR PHL General Bacteriology PHL 9. Genital Mycoplasma*/ Ureaplasma culture* PHL General Mycoplasma PHL 10. Legionella (tissue) Legionella urine antigen PHL General PHL General Bacteriology PHL Serology 11. Lyme disease Ab PHL General Serology PHL 12. PARASITIC SEROLOGY PHL General Serology PHL UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 72 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual TEST 13. REQUISITION DESTINATION PARASITIC SEROLOGY cont’d Only by special request from Topical Diseases' physicians: Cystercosis CDC 50.34 Rev.09/2002 Echinococcus (must be completed by Leishmania ref .physician) Schistosoma Strongyloides Toxocara Trichinella Trypanosoma Miscellaneous Filaria Center for Disease Control and prevention 1600 Clifton Road,N.E. Atlanta, Georgia U.S.A. 30333 Control and prevention 1600 Clifton Road,N.E Atlanta, Georgia U.S.A. 30333 NIH Filaria form (must be completed by ref.physician) Laboratory of ParasiticDiseases National Institute of Allergy & Infectious Diseases National Institutes of Health Building 4,Rm 126 Bethesda,Maryland U.S.A. 20892 Special Bact. PHL 14. Tetanus antitoxin titre Reference Bacteriology 15. Toxoplasma IgG Total Toxoplasma IgM PHL form 97-44(08/99) Serology PHL 16. VDRL (CSF) PHL General Serology PHL 17. Electron microscopy PHL General Virology PHL Tel. (416) 422-3000 18. Parvovirus Ab IgG, IgM PHL General Serology PHL 19. Histoplasma Antigen in Urine 20. Multi-Resistant Organism for MiraVista Diagnostics 4444 Decatur Blvd., Suite 300 Indianapolis, IN 46241 1-866-Mira Vista (647-2847) Phone: 317-856-2681 Special Research Microbiology UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 73 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Multiple Combination Bactericidal Test Room 3043B Children’s Hospital of Eastern Ontario, 401 Smyth Rd. Ottawa, ON K1H 8L1 UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 74 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Appendix III - Daily Work-Up for Architect Bench 1. ‘Log on” in Architect 2. Run daily/Weekly Maintenance in the morning, also run all the controls. - Don’t forget to replace and clean the filter under the architect. - Do not need to put septum in 0.5% Javex bottle used for Daily Maintenance, empty content when procedure done. 3. Back up weekly: a. Files to Architect: - f:drive-‘System’, ‘Utilities’, ‘F4-create back up’ and ‘Done’. b. QC and Test results to CD - ‘Results’,‘Stored Results’,‘Select All’,‘Archive’, must remove ‘√’ - delete records after archive before next step. - Insert CD into CD Drive. Follow instruction on screen. When finished press ‘Done’. Remove CD from CD Drive. Label archive date on front of CD cover. 4. Do architect inventory every Friday afternoon. 5. Document Laminar flow hood (MIBCT4) cleaning in 'mic'-go 'RESULT'-'Worklist”- Virology Architect. 6. Load specimens. Do in-house specimens first, then do the GW CMV Avidity specimens. GW specimens can be run throughout the evening and night shift. 7. Post and verify all QC in the LIS. 'Lab'. 8-Interface Menu i. -Architect-enter ii. 'Open' is highlighted-enter iii. Choose Result File Date that you want to post QC-enter iv. Press 'L' for 'Look'-F12 v. QCs are designated with a 'O' before sequential number. You must go into each QC and post result by pressing 'SHIFT & +' at the same time. Pop up will tell you the result was posted. vi. Press F5 twice to go to next QC result, continue until all QC result are posted. 8. If a new Control lot is opened, must update in Architect-follow ' To enter New Control Lot #' procedure. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 75 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual 9. QC rule violation: a prop up screen will alert us. a. 1-3s: repeat with new aliquot-if still fail- do Calibration. b. 1-2sd is a warning-check yesterday's QC printout sheet,and see if it was the same violationc. 1-2sd is OK, but 2 -2sd in two days is a rule violation-do calibration. d. If 2 controls are 1-2sd, do calibration. 10. Architect must be on 'running' mode overnight, so that all the solutions will be flushed regularly. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 76 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Appendix IV - Entering and Verifying Serology Refer-Out Results Refer-out Reporting Bench Workflow and Notes: Bench Workflow: 1. Check the fax machine at the secretary’s desk. If the secretary is not in, separate the received PHL reports. Separate out all the serology reports from the rest and keep any abnormal positive and results in a separate pile as well. Preliminary reports are NOT ENTERED unless they are abnormal positive results and can be filed immediately in the Iron Mountain box under the secretary’s desk. Also, check the fax machine in Virology beside John’s office for reports. Replenish paper if a fax machine is out. 2. Phone, enter and verify all significant positive results first. These tests include 9VD (ONLY if RPR is REACTIVE, and not previously positive), 9TSC/9HIV, 9HTLV, 9PARM). Positive reports get filed in the Positive PHL report binder in the Virology Lab (shelf beside the sink). Reports not from PHL (NML, CDC etc.) get filed in the black binder on the cabinet behind Lily. 3. Enter and/or verify any Amended reports or problem reports solved but awaiting to be finalized. 4. Check pending samples WEEKLY. Use the 9SERO worklist to find pending results. Fax PHL lists of pending reports and tests to be re-faxed. This is done by creating a document including patient’s first & last name, HCN, LIS order #, Date of collected and which tests are pending. 5. Proceed to enter and verify all other reports. Report all tests done by PHL, order the tests if not already ordered. If a final report is received and there are pending tests in the LIS order other than HTLV and HIV (e.g. Parvo IgM, HSV IgM etc.) call PHL to ensure test was ordered. If the test was ordered but is not being done by PHL enter as: “Not tested by PHL”. If a report has any discrepancies regarding patient information, call PHL immediately to verify and refax an amended report. 6. Tests done on the Architect which were sent to PHL for confirmation (9HCA, 9VD, 9TSC, 9HTLA) order the “9” sendout test codes if not already ordered and enter results under these codes. 7. Report all titres for tests in LIS EXCEPT HBsAb titres. 8. File all PHL reports by bench side into Iron Mountain boxes with the exception of the significant positive reports and non PHL reports (e.g. CDC, NML etc.). If a report page contains only Historical Data, KEEP IT and file it, attach it to the other report pages if you have them. 9. When Flu subtyping is done by NML. Enter the subtype under the Isolate Comment F8 window. Indicating subtyping is done by NML. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 77 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual NOTES: 1. When notifying PHL to send amended reports, keep the original in the PENDING RESULT folder. After receiving an Amended Report, match it up with the original report, shred the original and file the Amended report. 2. When calling PHL, they will only look up 2 reports at a time. Do not wait until there are more than 2 reports before calling for queries. Call PHL immediately as you come across the reports. Entering and Verifying Verbal Reports. Stat results from PHL are called to the laboratory before a faxed report is sent. These results must be called, entered and verified immediately. 1. Receiving the call: Record verbal PHL results on the green “Refer-out Test – PHL Verbal Results Recording Form” QPCMI17001a sheet. Ensure to fill in all sections including the patient’s First and Last name, LIS# and PHL# and the result. Read back information and results to verify correct records. 2. Enter the results: Open order entry. Search the order by entering the LIS number provided. Match the patient information provided with that in the LIS. Click the Result Tab. Enter each result using the options in the keypad. Do NOT free text results. Select “\” to enter canned messages and the PHL (or other site) number. If there are special notes/interpretations/comments inquire whether they should be added in the canned message field. DO NOT enter “Verbal Report” in the canned message field. Document in the call window that you received a verbal report from PHL and who you spoke with. DO NOT VERIFY AT THIS STAGE. Save. If the test was previously verified (e.g. as “sent to PHL”) a pop-up window will appear warning a modification of verified results. Use this as a double check, and accept results by clicking “OK”. 3. Verify the result With the verbal report still in front of you, go back into order entry to check and verify the result. Double check all the patient information and check them off the report as you do so. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 78 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Open the results tab. Check results. Open the canned message (click “ \ “) and ensure the entire message is there, no letters missing or extra letters at the beginning or end of the comment, that the canned message is not entered twice and ensure the PHL number is correct - check every number. Verify the test result after the result and canned message is checked, by hitting “ [ “ key on the test Initial and date the PHL Report. 4. Calling the result. After verifying the result call the result to ward or ordering physician. Provide all the information including the patient’s MRN, date of collection of sample and result. Make sure results are read back. In order entry, order 8call or 8calo for units. In the call window document the phone call including the name of the person taking the result. File the verbal results recording form in Virology. There is a “PHL Verbal Reports” binder. Entering and Verifying Serology Refer-Out Results Procedure Refer-out test results for blood specimens can only be recorded in the LIS using SCC lab module. When the reports come back from a reference laboratory, the result, reference lab number and reporting date are entered. Enter results by PRIORITY: 1. Positive Results 2. Pending Results (problem reports solved but awaiting to be finalized) 3. Prenatal Results 4. Non-Prenatal Results PROCEDURE: 1. Log on to “SOFTLAB”, open ORDER ENTRY. 2. Search by Order number, ensuring “Open in Edit Mode” is checked, and click Find or press Enter to launch search. If no order number is indicated on the PHL report, look for the order by using the HCN, MRN or Last name/First name with DOB. If an order is found and has the same collection date, use this order. If no order is found but the patient is in the LIS and Dr. Mazzulli is the provider (e.g. fertility clinic), create a new order. A new visit can be created with the referring doctor if necessary. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 79 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual If a report does not have Dr. Mazzulli as the Provider but the report has an LIS order number, the report can be entered. If no patient is found in the LIS and/or Dr. Low is not the provider, write on the report “patient not found” and forward the report to the sectary for mailing. 3. Match the patient information Compare the first and last name, Date of Birth, MRN, HCN. (All information) Ensure you chose the correct order when searching with an MRN/HCN etc. by matching the collection date of the sample in the LIS and the date on the report and the auxiliary number if provided and the sample from UHN. If the patient has a different last name, verify under “Show Linked Patients” in Order Entry to see if the last name has been changed. If the last name on the report is not present, call PHL to correct the last name. If the last name is present, accept the report. Call PHL to verify any other discrepancies and to re-fax an amended report immediately as you come across these reports. Do not batch them together for later. PHL will fix and refax a maximum of 2 reports per phone call. File reports with discrepancies waiting for amended results in the ‘Pending Results’ folder. 4. Enter results When entering results, only have the ONE report you are entering in front of you. Click the Result Tab after you have matched the patient information. Enter each result using the options in the keypad. Do NOT free text results. Enter results in the order they appear on the printed report as to not miss or skip any results (as opposed to test order in the LIS). Select “\” to enter canned messages and the PHL (or other site) number. If there are special notes/interpretations/comments inquire whether they should be added in the canned message field. If there are many tests in an order you can copy and paste the PHL # comment and paste it after the canned messages in each test results you. DO NOT VERIFY AT THIS STAGE. Save. If the test was previously verified (e.g. as “sent to PHL”) a pop-up window will appear warning a modification of verified results. Use this as a double check, and accept results by clicking “OK”. Initial and date the report Check and Enter reports and put them aside before verifying. After 5 reports have been checked and entered take the pile and start verifying those 5 results one at a time. Do not enter a result and verify reports immediately (one by one). 5. Verifying Results DO NOT VERIFY ANY RESULTS WIHTOUT THE REPORT INFRONT OF YOU. Take the pile of 5 reports just entered, one at a time, check results through order entry by the order number. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 80 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Double check all the patient information and check them off the report as you do so. Open the results tab. Check results in the order appearing on the PHL report. Ensure the correct result is entered for each test. Open the canned message (click “ \ “) for EACH test and ensure the entire message is there, no letters missing or extra letters at the beginning or end of the comment, that the canned message is not entered twice and ensure the PHL number is correct - check every number. Verify individual test result after the results and canned message is checked one by one, by hitting “ [ “ key on EACH test as checked. Initial the PHL Report and file in the box provided. All positives should already have a call made. Double check the positive results have been called before verifying these results. . File positive results in the appropriate section in the positive results binder. 6. Pending results Check pending list weekly at a minimum. Log on to SOFTLAB, double clicking Resulting Worklist icon. Fill out the screen as follows: - Under “Template” enter: 9SERO - Status as Pend + Nonver. - Change order# range to include several months - Check: Received only, hit OK to search. Pending results must be faxed to PHL with sample information to get the report re-faxed. DO NOT ENTER OR VERIFY ANY PENDING RESULTS IN THIS WORKLIST. Orders that have been received and sent to PHL with no results received need to be faxed to PHL so they may re-fax us the results back. If there are old orders with some results entered but some tests still pending PHL can be faxed the same way as above but only include tests that are pending. If there are orders that have been entered but not verified DO NOT VERIFY. The information from these orders must be sent to PHL to get a re-fax of results as well before verification can occur. In these cases, send a fax to PHL with the following information. A table in excel or word can be created to include all the pending orders. Send the fax with a cover page to: 416235-6552. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 81 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Last Name First Name DOB HCN (if no HCN provide mrn) LIS order # Date of collection Missing tests 1. 2. 3. Keep a copy of faxed results in the pending results folder and follow up on these reports. If an order has a pending test (e.g Parvo IgM/HSV IgM) that was sent to PHL but not done confirm by telephone if it is being done. Result as appropriate. If the test is not being done, result the test as “Not tested by PHL” PHL can be called for inquiries or re-faxes at their customer service phone number, but will only deal with a max or 2 UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 82 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Appendix V - Autoverification Process I. Introduction To document the autoverification process. Autoverification is the process by which the computer performs the initial verification of test results. Any value, that falls outside of the defined criteria, must be assessed by a technologist before release of results. II. Procedure 1. The laboratory has a policy signed by the laboratory director approving the autoverification procedure. 2. The results of autoverification is thoroughly tested, appropriately documented and signed by the section head/designee before implementation. 3. If changes are made to the autoverification rules initially chosen and documented, the process is reverified as to its accuracy. 4. The autoverification process is checked yearly. AUTOVERIFICATION FOR THE ARCHITECT INSTRUMENT POLICY: The Architect instrument performs the following tests for the Serology department: f. Hepatitis B Surface Antigen g. Hepatitis B Surface Antibody h. Hepatitis B Core Antibody i. Hepatitis A IgM Antibody j. Hepatitis B Core IgM Antibody k. Hepatitis Be Antigen l. Hepatitis Be Antibody m. Hepatitis C Antibody n. Rubella Antibody o. EBV VCA IgG p. EBV EBNA-1 q. Cytomegalovirus Antibody: CMV IgG, CMV IgGR ,CMV IgM and CMV Avidity r. Transplant Screen UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 83 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Autoverification will occur as follows: TEST NAME SOFT RESULT TEST CODE Hep B Surface Ag 8HAG NEGATIVE TRANSLATION ACTION Negative Autoposted Autoverified Hep B Surface Ag 8HAG REACTIVE Review? NOT Autoposted NOT Autoverified Hep B Surface Ab 8HAB REACTIVE POSITIVE Hep B Surface Ab 8HAB NEGATIVE Negative Hep B Surface Ab 8HAB GZ-NEGATIVE Neg Autoposted Autoverified Autoposted Autoverified Not Autoposted Not Autoverified Hep B Core Ab 8HBC REACTIVE REACTIVE Hep B Core Ab 8HBC NEGATIVE Negative Hep A IgM Ab 8HAV REACTIVE REACTIVE Hep B Core IgM Ab Rubella 8HBCM REACTIVE POSITIVE 8RUB NEGATIVE Negative Rubella 8RUB GRAYZONE Negative Not Autoposted Not Autoverified Autoposted Autoverified Not Autoposted Not Autoverified Not Autoposted Not Autoverified Autoposted Autoverified Autoposted Autoverified REFLEX TESTS 8HBC Hep B Core Ab 8HBC2 8HBC2 8RUB2 UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 84 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual TEST NAME RESULT EBV VCA IgG SOFT TEST CODE 8EBV TRANSLATION ACTION EBV VCA IgG 8EBV REACTIVE REACTIVE EBV VCA IgG 8EBV EQUIVOCAL EQUIVOCAL EBV EBNA-1 8EBNA NONREACTIVE NONREACTIVE EBV EBNA-1 8EBNA REACTIVE REACTIVE EBV EBNA-1 8EBNA EQUIVOCAL EQUIVOCAL CMV IgG CMV IgGR CMV IgG CMV IgGR CMV IgG 8CMS 8CMG 8CMS 8CMG 8CMS 8CMG NONREACTIVE NONREACTIVE CMV IgM 8CMM CMV Avidityy 8CMVA NONREACTIVE NONREACTIVE REACTIVE REACTIVE GRAYZONE 6.00-15.00 AU/mL (low Level) NONREACTIVE Negative REACTIVE Positive <50 % Low Avidity >60% High Avidity REFLEX TESTS Autoposted Autoverified Autoposted Not Autoverified Autoposted Not Autoverified Autoposted Autoverified Autoposted Not Autoverified Autoposted Not Autoverified Autoposted Autoverified Autoposted Autoverified Autoposted Autoverified Autoposted Autoverified Autoposted Autoverified UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 85 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Appendix VI - Shipment of Samples to HSC 1. Fill out a HSC requisition. (Molecular tests require a colour coded UHN/MSH refer out Requisition to HSC Molecular Microbiology, Lab no. and tech initials) 2. Put specimen and requisition in biohazard bag, and then in a brown paper bag. 3. Put ‘Hospital for Sick Children, Microbiology Receiving,3rd Floor Atrium, Rm3676’ sticker on brown bag. 4. Put labeled brown bag into blue specimen container, and send to ‘TG specimen management’. 5. Enter in LIS as ‘specimen send to HSC’ and finalize. 6. Also enter in serology send out binder. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 86 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Appendix VII - Looking Up Previous Hepatitis Results in EPR 1. Log on ‘EPR’. 2. Enter’ user ID’ & ‘Password’. s. Click on ‘All UHN Patients’. t. Enter ‘MRN # in ‘Patient ID’, press ‘Enter’. u. Click on ‘any visit’, then click on ‘Goto Selected visit’. v. Click on ‘Chart Review’, ‘Continue?’,Click on’ (y) yes’. w. Click on ‘Hepatitis Profile’, click on ‘OK’. x. All previous Hepatitis test results will be displayed, e.g. HBsAg, HBsAb, HBcAb IgM, HBeAg, HBeAb, HC Ab, and HAAb IgM. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 87 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Appendix VIII - Printing of Pending List 1. Log on ‘Lab’. 1. Enter ‘ID’ &’Password’. 2. ‘3’-Results 3. ‘View/Enter Results by Sel Tests’. 4. Select tests by ‘Template’,’Enter’. 5. Enter ‘8SERO’ under ‘Template’, ‘Status- pend +nonver’. 6. From order( enter last month’s lab #) to’ leave it blank’.’F12’. 7. ‘F9’ to print. Choose either ‘TC2RVIR’ or ‘TC3R MIC’ printer to print. 8. Look up each record, and find out why the results are still pending. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 88 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Appendix IX – Donor Serology and Molecular Tests List Donor Serology and Molecular Testing at Mount Sinai Hospital Donor Serology and Molecular Testing at Mount Sinai Hospital for TGLN Donor Serology and Molecular Testing for at MSH Living Donors UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 89 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Appendix X – Movement Throughout Containment Zones Policy: All specimens and potentially infectious materials transported throughout the hospital must be done in accordance with the policy for Transportation of Dangerous Goods and Material. Purpose: This policy ensures the safe transportation of specimens and dangerous materials to minimize potential biohazard and safety risk to the public and to the staff handling the materials. Responsibility: Management and employees Procedure: When transporting specimens and potentially infectious materials, they must be appropriately contained. To pick up or drop off serology specimens, follow the steps outlined. 1. Whether picking up or dropping off samples, retrieve the designated transportation cart located beside the technicians. This cart is CLEAN and should be wiped with alcohol before leaving the laboratory. 2. Ensure the cart is stocked with all necessary supplies including: Virox wipes, lab coat, paper towel, biohazard garbage bags and gloves of various sizes. 3. The designated grey box located beside the architect will be used to transport the specimens. While in transit, the lid should be kept on at all times. 4. Capped specimens should be placed in plastic racks and these racks can be secured into the large grey box for transport. Secure the lid onto the grey box and place onto the clean trolley. 5. After removing lab wear and washing hands, proceed outside the laboratory. Do no use patient elevators to transport samples. 6. Do not manipulate the box or samples in any way while in transit. Should a spill occur, refer to the materials on the cart of clean up. Discard waste in biohazard garbage bag provided, secure in box and bring back to the laboratory for disposal. 7. At the outside location, using gloves, transfer specimens from the grey box to the designated location. Discard gloves after use and wash hands. 8. Upon returning to the laboratory, remove specimens and return the cart and grey box to their locations and refill any materials used. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 90 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual To drop off virology dangerous chemical waste, follow the steps outlined. 1. Waste must be transported to the MSH Autopsy Suite on the 6th floor, room 6-311-4. A chemical waste disposal form must be filled out and emailed to Salim before the waste is transported and delivered. The waste should be brought down only at 3:30pm. See Lilly or Linda for Salim’s email. 2. When transporting waste throughout containment zones, retrieve the designated transportation cart located beside the technicians. This cart is CLEAN and should be wiped with alcohol before leaving the laboratory. 3. Ensure the cart is stocked with all necessary supplies including: Absorbant pads, Virox wipes, lab coat, paper towel, biohazard garbage bags and gloves of various sizes. 4. Ensure the chemical waste containers lids are properly secured and place containers on designated cart. After removing lab wear and washing hands, proceed outside the laboratory. Do no use patient elevators to transport samples. 5. Do not manipulate the containers in any way while in transit. Should a spill occur, refer to the materials on the cart of clean up. Discard waste in biohazard garbage bag provided, secure in box and bring back to the laboratory for disposal. Chemical spill kits are available if a spill occurs inside the 6th floor laboratories. 6. At the outside location, using gloves, transfer containers to the designated location. Discard gloves after use and wash hands. 7. Upon returning to the laboratory, clean and return the cart to its location and refill any materials used. UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 91 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Record of Edited Revisions Manual Section Name: Serology Page Number / Item Date of Revision Annual Review Molecular Testing - HBV DNA-Reporting Added Para. AxSym System-Reporting Results HBsAg AxSym - CMV IgG Antibody (x) AxSym – Quality Control External Controls AxSym - Added Failed QC AxSym HbsAg Surface Antigen - Pt. Samples Appendix V (f) Added Steps HCV-RNA PCR Reporting – Positives Annual Review Page 6 – Interpretation of Results – OD changed for Positive and Interdeterminate. Page 6, 15 – Run external control – include QC and instrument problems Page 8 – re-centrifuge cloudy, previously frozen, reconstituted samples. Page 8 - Refer to Abbott Operation Manual vol. 1&2 for specific maintenance procedures Page 13, 14 – report to MOH added Page 13, 14 – centrifuge before repeating Page 16, file log and external control out of range Page 48 – store VDRL samples for 3 months after testing Page 51 – 56 VZV Vidas revised Page 57 – WNV IgG not currently in use Page 61 – WNV IgM not currently in use Page 67 - Molecular Testing - Chlamydia Trachomatis & Neisseria gonorrhoeae Page 67 – urine but not more than 60 mL added Page 68 – specimen not lysed…added Page 68 – tubes may be blotted Page 70 – handling samples after lysing Page 71,72 Procedure change Page 72, interpretation of result - change MOTA score Page 73, reporting – indeterminate Page 76 – do not vortex working master mix Page 76 – specimen dilution protocol Page 77 – 80 procedure and reporting changed May 12, 2003 October 10, 2003 October 28, 2003 October 28, 2003 October 28, 2003 October 28, 2003 January 22, 2004 January 15, 2004 April 02, 2004 May 26, 2004 Signature of Approval May 20, 2005 Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli May 20, 2005 Dr. T. Mazzulli May 20, 2005 Dr. T. Mazzulli May 20, 2005 Dr. T. Mazzulli May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 92 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Page Number / Item Date of Revision Page 81 – QC procedure changed Page 93 – procedure changed Page 86 – 88, instrument instructions Page 90 – WNV RT-PCR Page 92 – lysis buffer Page 93 – General Precaution section revised Page 94-100 – procedure revised Page 101 – schedule revised Page 105 – shipping to St. Joseph’s Page 121 – shipping to HSC Annual Review Page 128 – Updated decontamination procedure Page 6 – C. difficile toxin indeterminate range changed Page 13 – HBc IgM reporting guide changed Page 15 – MV, Rubella reporting Annual Review Added links to TGLN Procedures Annual Review Added Labour and Delivery STAT HBsAg and HIV Instruction Added Immuncor Capture-CMV Assay Revised Document numbers Added Ortho ELISA Assays for HBcore, HCV, HTLVI/II for Donor Testing Annual Review Report positive C. difficile toxin as an ISOLATE in the LIS Serology Referred Out Test Results Entry Phrases added Replaced HBsAg, HIV 1/2 HBcAb, HCV Ab, HTLV I/II Ab donor serology sections Added Aspergillus Galactomannan Antigen Detection Assay Annual Review Architect System added C. difficile Toxin EIA edited with Premier kit Annual Review Remove C. difficile toxin EIA Syphillis screen added to Architect System Modified RPR for Cadaver donors Updated Axsym procedure Signature of Approval May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 May 20, 2005 June 2, 2005 December 29, 2005 December 29, 2005 May 29, 2006 May 29, 2006 March 21, 2007 June 8, 2007 March 19, 2008 Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli July 14, 2008 July 14, 2008 July 14, 2008 Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli July 14, 2008 September 16, 2008 Dr. T. Mazzulli Dr. T. Mazzulli March 09, 2009 November 18, 2009 Dr. T. Mazzulli Dr. T. Mazzulli November 18, 2009 Dr. T. Mazzulli November 18, 2009 May 17, 2010 May 17, 2010 May 17, 2010 January 10, 2011 January 31, 2011 January 31, 2011 January 31, 2011 Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 93 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Page Number / Item Date of Revision Updated VZV procedure Updated Appendix II Updated Architect procedure Removed Appendix III – Send out procedure to St. Joseph Hospital, Hamilton ON Replaced Appendix III - Daily work-up for Architect Bench Moved PCP DFA from Virology Section Annual Review Architect system – added HTLV Removed HTLV for TGLN Added to Table of Contents Donor Serology and Molecular Testing at Mount Sinai Hospital for TGLN Architect system – added CMV IgM and CMV avidity Annual Review Edited CMV Avidity testing procedure Added Appendix XI and XII – CMV Avidity workflow Edited Architect system Edited EBV serology Edited Autoverification procedure Removed AxSYM HHsAg confirmation Edited Immucor CMV procedure Updated Cadaver serology procedure Edited Syphilis Screen RPR Serology procedure Updated Architect daily workflow Added George Washington CMV avidity confirmation algorithm Updated Appendix IV – Entering and Verifying Refeerout Serology Results Updated EBV Serology, reference added Annual Review Edited George Washington CMV avidity confirmation algorithm Added George Washington Anti-HCV algorithm Updated TGLN Call Back procedure Updated Architect section Updated Appendix IV – refer-out tests reporting Update Architecht, Axsym, DONOR, Immucor, appdx3, appdx 5 Signature of Approval January 31, 2011 January 31, 2011 May 31, 2011 May 31, 2011 Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli May 31, 2011 Dr. T. Mazzulli May 31, 2011 May 31, 2011 June 20, 2011 June 20, 2011 July 15, 2011 Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli March 20, 2012 March 20, 2012 September 12, 2012 September 12, 2012 September 30, 2012 September 30, 2012 September 30, 2012 September 30, 2012 September 30, 2012 September 30, 2012 September 30, 2012 September 30, 2012 January 28, 2013 Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli February 12, 2013 Dr. T. Mazzulli February 28, 2013 April 18, 2013 April 18, 2013 Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli April 18, 2013 May 21, 2013 May 31, 2013 May 31, 2013 September 17, 2013 Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli Dr. T. Mazzulli UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 94 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Page Number / Item Date of Revision Addition Appendix XII, modify appendix I and III, delete appendix VII Edit Appendix XII, include chemical waste transport. Moved GW in its own section. Add reporting/ receiving section. Update Appendix XII include easy mag transport EBV VCA IgG/EBV EBNA-1 IgG addition to architect manual. GW HC flowchart update, GW confirm algorithm update GW HCV flowchart update, Appendix update, Axsym manual update – remove CMV Appendix III update Removal of Axsym manual. Addition of Donor section to Architect Manual. Note addition to STAT needlestick incident reporting Annual review Remove Evolis donor manual, replace with Gw hcae evolis manual Update Architect manual. Removal of Evolis donor testing Fix headers/footers Indeterminate CMV Immucor interpretation added. TGLN section removed and copied to standalone TGLN call back procedure. Link to this manual created. GW procedure: CMV Avidity Troubleshooting added: diluting sample when CMV IgG is too high to calculate avidity Donor testing RPR to 8VD -Wash buffer filling replaced with ARM procedure. -Added under Donor/Recipient Serology reporting: Reporting REACTIVE results for Alberta Donors only: - If repeat results support the initial Reactive result, enter repeat results in the result comment and verify results. - If repeat results DO NOT support the initial result, type “Note” at result area, enter initial result and repeat results in the comment and verify results. -Donor/Recipient resulting divided into Ontario living donor and non-ontario &cadaveric donor sections Hep C Ab, HIV , HTLV and VD for living donor: Repeatedly positive report as ‘reactive’ with comment “Repeatedly reactive, sent to PHL for further testing” Annual Review Signature of Approval October 30, 2013 Dr. T. Mazzulli January 15, 2014 January 27, 2014 Dr. T. Mazzulli Dr. T. Mazzulli March 11,2014 Dr. T. Mazzulli March 14, 2014 March 27, 2014 Dr. T. Mazzulli Dr. T. Mazzulli April 4, 2014 May 28, 2014 Dr. T. Mazzulli Dr. T. Mazzulli October 24, 2014 Dr. T. Mazzulli May 1, 2015 Dr. T. Mazzulli May 1, 2015 Dr. T. Mazzulli June 17, 2015 Dr. T. Mazzulli August 7, 2015 Dr. T. Mazzulli October 15, 2015 Dr. T. Mazzulli UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc Policy # MI/SER/v48 Page 95 of 116 Microbiology Department Policy & Procedure Manual Section: Serology Manual Page Number / Item Date of Revision Remove 8HAG (replace with 8HAGX) Remove 8HBEB, 8HBEG tests Update 8HAGX positive reflex procedure/resulting table Removed flowcharts for 8HAGX algorithm Update 8HAGX confirmation interpretation table Added description of reagents used in Working Wash solution for CMV Immucor. Remove Alberta Only reporting for Donors Add donor storage instructions Updated Donor reporting table p.3 Immucor CMV for wash solution added phrase: ‘Mark ‘ Date Made’ on Working Wash Solution bottle.’ p.4 Immucor CMV: step 8: changed from wash gently 5 times to gently 6 times. p.4 Immucor CMV: Interpretation of results for Donors removed: ‘Donor samples received from the architect bench (8HAGX) for Capture-CMV testing must be resulted and verified under both 8CMSE and 8CMS’ p.4 Step 11 inserted RCF specific to ImmuSpin centrifuge programming. p.5 Immucor CMV: QC changed external controls from Run Virotrol I /ViroTorch to ViroTorch/ ViroTorch-M. p.5 Immucor CMV: Reference updated with version: 9/10 October 29, 2015 Signature of Approval Dr. T. Mazzulli UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT NOTE: This is a CONTROLLED document for internal use only. Any documents appearing in paper form are not controlled and should be checked against the document (titled as above) on the server prior to use. D:\533562715.doc