Multidisciplinary Critical Care Consultation Policy:
advertisement

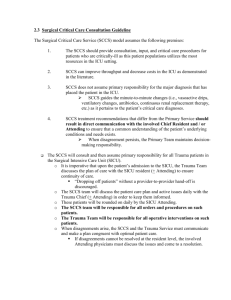
2.1.1 Surgical Critical Care Consultation Guideline The Surgical Critical Care Service (SCCS) model assumes the following premises: 1. The SCCS should provide consultation, input, and critical care procedures for patients who are critically-ill as this patient populations utilizes the most resources in the ICU setting. 2. SCCS can improve throughput and decrease costs in the Intensive Care Unit (ICU) as demonstrated in the literature. 3. SCCS does not assume primary responsibility for the major diagnosis that has placed the patient in the ICU. SCCS guides the minute-to-minute changes (i.e., vasoactive drips, ventilatory changes, antibiotics, continuous renal replacement therapy, etc.) as it pertains to the patient’s critical care diagnoses. The Primary Surgical team is responsible for decisions that involve the major diagnoses 4. SCCS treatment recommendations that differ from the Primary Service should result in direct communication with the involved Chief Resident and / or Attending to ensure that a common understanding of the patient’s underlying conditions and needs exists. When disagreement persists, the Primary Team maintains decisionmaking responsibility. The SCCS will consult and then assume primary responsibility for all Trauma patients in the Surgical Intensive Care Unit (SICU). o It is imperative that upon the patient’s admission to the SICU, the Trauma Team discusses the plan of care with the SICU resident (+ Attending) to ensure continuity of care. “Dropping off patients” without a provider-to-provider hand-off is discouraged. o The SCCS team will discuss the patient care plan and active issues daily with the Trauma Chief (+ Attending) in order to keep them informed. o These patients will be rounded on daily by the SICU Attending. o The SCCS team will be responsible for: Entering all orders Performing all procedures necessary for invasive monitoring (i.e., arterial lines, central venous lines, dialysis lines, etc.) Performing all bedside operative procedures (i.e., percutaneous tracheostomy, percutaneous endoscopic gastrostomy, abdominal washouts, etc.) o The Trauma Team will be responsible for all procedures performed in the Operating Room. o When disagreements arise, the SCCS and the Trauma Service must communicate and make a plan congruent with optimal patient care. If disagreements cannot be resolved at the resident level, the involved Attending physicians must discuss the issues and come to a resolution. The SCCS will consult and provide critical care services for all General or Subspecialty Surgical Service patients admitted to the SICU that: o Require inotropic support and / or invasive monitoring. o Require invasive, non-invasive, or specialty ventilatory management. o Require Continuous Renal Replacement Therapy (CRRT) management. o Are hemodynamically unstable or have active critical care issues. These patients will be rounded on by the SICU Attending of the Week. Each day the SCCS team will discuss the care and issues of the patients that have arisen in order to keep the Primary Service informed. If the Primary Team wishes changes in management or additional therapeutic interventions, these patient care concerns and / or additional written orders must be discussed with the SCCS to ensure continuity and completeness of care. The SCCS will be responsible for all ICU procedures on such patients (see above). The Primary Service will be responsible for for all procedures performed in the Operating Room on such patients. o It is imperative that upon the patient’s admission to the SICU, that the General or Subspecialty Service discuss the plan of care with the SICU resident and / or the SICU Attending to ensure continuity of care “Dropping off patients” without a person-to-person hand-off is discouraged. o The SCCS team will discuss the patient care plan and active issues daily with the General or Subspecialty Service to keep them informed of any and all critical care issues / concerns. o These patients will be rounded on by the SICU Attending of the Week. o When disagreements arise, the SCCS and the General or Subspecialty Service must communicate and make a plan congruent with optimal patient care. If disagreements cannot be resolved at the resident level, the involved Attending physicians must discuss the issues and come to a resolution. The SCCS will be available for consultation and management of all General or Subspecialty Service patients admitted to other ICU’s (MICU, BICU) if requested to do so. o It is the responsibility of the General or Subspecialty Service to consult the SCCS. o Consultation is encouraged in patients who: Require inotropic support and / or pulmonary artery catheter monitoring. Require invasive, non-invasive, or specialty ventilatory management. Require CRRT management. Are hemodynamically unstable or have active critical care issues. o All efforts will be made to transfer these critically-ill patients to the SICU to keep them in one central location to optimize patient contact and care. Consultation at the time of admission for patients not included above is at the discretion of the Primary Service, but critical care issues should be apparent o Simple admission to the SICU for nursing care / wound care / pulse checks / etc. does not require a SCCS consultation. Consultation will be ongoing until critical care issues resolve. In order to avoid confusion and divergent patient care plans, it is imperative that all written orders by the Primary Service be discussed with the SCCS. The SCCS will triage the most critically-ill patients to be physically located within the SICU. This allows constant contact between the SCCS and the patient. If necessary, the SICU Attending may need to triage out less critically-ill patients to provide space for sicker patients. The ultimate authority on which patients will be cared for in the SICU is the SICU Attending.