Calculating and Allocating Drug Costs
advertisement

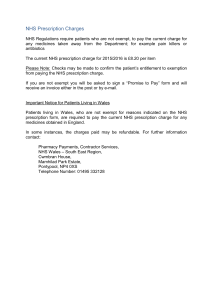
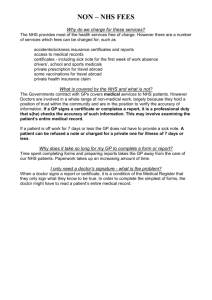
Calculating and Allocating Drug Costs (last updated September 2006) Introduction The purpose of this information and diagram is to illustrate the main features of how drug costs are calculated and recharged to prescribers. There are links to more detailed explanations where appropriate. This information is intended to be used as a resource by NHS staff who are interested in the drugs charging process. NHS Prescription Services has a system to calculate reimbursements and remuneration to all dispensers of drugs that are registered in England. This only applies to drugs that are issued on a prescription (FP10) form and does not include private prescriptions or non-prescription medicines. The prescriber of the medicine is captured as part of the information on the FP10 form and this allows the information to be viewed on both a dispenser and prescriber basis. GUIDANCE Pharmaceutical Price Regulation Scheme (PPRS) The prices of branded medicines and the profits that manufacturers are allowed to make on their sales to the NHS are regulated by the Pharmaceutical Price Regulation Scheme (PPRS). This is an agreement between the Department of Health (DH) and the branded pharmaceutical industry represented by the Association of the British Pharmaceutical Industry (ABPI). The PPRS is a voluntary, non-statutory scheme which indirectly controls the prices of branded licensed medicines to the National Health Service in the UK by regulating the profits that companies can make on these sales. It does not cover products that can't be prescribed under NHS Pharmaceutical Regulations, standard branded generics, in-vitro diagnostics or unlicensed products supplied on a 'named patient basis'. The purposes of the scheme as stated in the agreement are: to secure the provision of safe and effective medicines for the NHS at reasonable prices; to promote a strong and profitable pharmaceutical industry capable of such sustained research and development expenditure as should lead to the future availability of new and improved medicines; encourage the efficient and competitive development and supply of medicines to pharmaceutical markets in this and other countries. Follow this link for further information click here Supply and Reimbursement of Generic Medicines From 1st April 2005 the Department of Health (DH) reduced the Drug Tariff price of drugs which are readily available by introducing a new Category M. The scheme applies to all generic licensed NHS medicines dispensed in the community in England that previously qualified to fall under category A of the Drug Tariff. The price of category M products in the drug tariff is based on a calculation which incorporates the volume-weighted, average price charged by manufacturers Purchasing and Supply Agency The NHS Purchasing and Supply Agency (PASA) was set up as an agency of the Department of Health to oversee, modernise and improve supply management across the NHS in England. Currently contracting is undertaken by regional/divisional pharmacy purchasing groups, representing a partnership between trusts and PASA. These contracts include the particular delivery arrangements offered by the manufacturer. Where there is no contract for a product, trusts may put in place a prime wholesaler agreement and use this to achieve discounts. Alternatively, they may simply purchase their supplies from one or more wholesalers. PASA is currently leading a project to improve the supply chains for pharmaceutical products into the NHS. Association of British Health-Care Industries (ABHI) The Association of British Health-Care Industries (ABHI) is the trade association for the medical systems industry. The Part IX Drug Tariff forum of the ABHI has agreed with the Department of Health and NHS Prescription Services the formula for calculating price increases for devices and appliances in Part IX of the Drug Tariff. Statement of Financial Entitlement (SFE) and General Medical Services (GMS) Contract The SFE covers remuneration of General Medical Practitioners and sets out the payments. Click here Under the terms of the General Medical Services (GMS) contract which came into force in April 2004 a PCT receives a cash-limited sum for GMS services as part of its total allocation. PCTs will allocate resources in three main ways: A global sum to cover running costs Quality payments to reward standards Enhanced services payments for practices which expand the range of services they provide Local Pharmaceutical Services Local Pharmaceutical Services (LPS) provide an opportunity to develop integrated local arrangements which address and meet local priorities and needs. Service providers will be rewarded in a manner and at a level agreed by the PCT and the LPS provider. The new arrangements provide an alternative legal framework for the provision of pharmaceutical services under locally agreed contracts. The primary legislation for Local Pharmaceutical Services (LPS) is set out in the Health and Social Care 2001. The Act enables PCTs to develop new ways of contracting for and delivering pharmaceutical services. In addition it allows provision, within the LPS contract, of a broader range of services than are traditionally associated with pharmacy. Pilot schemes are in progress currently and a PCT must reimburse the LPS provider in accordance with the rates and conditions specified in the Drug Tariff. The PCT will remunerate the LPS provider in respect of the provision of piloted services. The amount or level of remuneration and the timetable for its payment is a matter to be agreed between parties to the agreement. Where NHS Prescription Services is to handle the payment of the remuneration on behalf of the PCT, notification by the PCT of the amount to be paid must be made within the timetable that the NHS Prescription Service specifies. National Pharmaceutical Contract The new pharmacy contract reflects the vision for a diverse and flexible community pharmacy service. The framework offers choice to PCTs in the services they commission from community pharmacy to meet local needs and priorities. Benefits for patients and the NHS include: Improved patient choice and convenience in accessing medicines. Management of long term conditions Reducing health inequalities and improving public health Improved patient safety Sustained achievement of the 24/48-hour access target Supporting GPs and other primary care staff Supporting the delivery of nGMS Better value for money The framework categorises services into essential, advanced and enhanced, with a focus on quality and outcome in all cases. Essential services are defined as those services that must normally be provided by all community pharmacy contractors under the new arrangements (e.g. dispensing, repeat dispensing, disposal of medicines). Activities to be undertaken as part of each essential service and standards of delivery have been specified. Advanced services are those which require accreditation of the pharmacist providing the service and/or specific requirements to be met in regard to premises, such as consultation areas. An example is medicines use review (where a pharmacist periodically, systematically discusses with a patient their medicines, to check how things are going and identify issues of compliance or any problems the patient may have with their medicines). Enhanced services can be commissioned by PCTs, according to the needs of their local population. Examples include minor ailment schemes, needle exchange and supervised methadone for drug misusers, smoking cessation clinics and supplementary prescribing. Reimbursement & Remuneration The Drug Tariff outlines what will be paid to contractors for NHS services provided. This includes reimbursement (the cost of the drugs, appliances etc which have been supplied against an NHS prescription form) and remuneration (what is paid as part of the dispensing contract e.g. professional fees/allowances etc). The total sum is paid each month for the products and services supplied as part of the contractors NHS contract. It can differ slightly, depending on the type of dispensing contractor. Follow this link for further information drug tariff guidance There are four main groups for which payments are made: Pharmacists Appliance Contractors Dispensing Doctors Personally Administered GP claims NHS Prescription Service calculates both the reimbursement and remuneration that each group should be paid based on the drug tariff as described above. NHS Prescription Services makes the actual payments to only the first two of this group and passes information to the relevant PCT to make payments to GP's. Figure 2. shows the elements of payment for each different group Actual Cost Basic Price Discount Container Other fees On Cost Allowance Pharmacist Appliance Contractor Dispensing Doctor Personal Administration Figure 2. Remuneration Pharmacists Pharmacists submit all prescriptions they have dispensed monthly to NHS Prescription Service, sorted into the chargeable group (where patients have paid a prescription fee), the non-chargeable group and then by prescriber. The basic price of the drug which is reimbursed is calculated based on an interpretation of the drugs dispensed and reference to the cost of that drug in that particular month. Figure 3 shows the basis of payment for the different items which can be reimbursed on an FP10 prescription. Figure 3. Reimbursement The reimbursement cost of the drug (known as the Net Ingredient Cost, NIC) is discounted based on a sliding scale depending on the size of the batch of prescriptions submitted in that particular month. This is designed to reflect the level of discount a dispenser would be expected to achieve from suppliers. The discount does not include any zero discount products as a contractor will not have been able to obtain a discount on these items. A container allowance is paid in line with rules set down in Part IV of the Drug Tariff. This is also included in the cost of drugs. The remuneration element is also calculated in line with the Drug Tariff rules. There are a range of fees paid depending on what has been dispensed and also some fees based on the number of prescriptions in the monthly batch. Any charges collected from patients are netted off the overall payment due as the Pharmacist retains these. Locally Authorised Payments are authorised by the relevant PCT and are communicated by the PCT to NHS Prescription Service through a secure web connection. There are a standard range of payments that can be made as well as payments that are specific to the PCT. These payments need not necessarily cover the same period as the prescriptions. Pharmacists are paid on the first day of the second month following that in which they submitted their prescriptions. The following table shows an example: April May June 1st July Prescriptions dispensed Prescriptions batch sent to NHS Prescription Services Pricing finished Payment made. To ease cash flow problems for Pharmacists an advance is paid at the start of the previous month and then recovered when the prescriptions are paid. This advance is calculated on the following basis: The average cost of prescriptions from the previous months pricing is paid for the current month's submission and uplifted by 1%. The account value is reduced to 80% and in addition appropriate local payments or deductions are included. For further information see "Your monthly dispensing payment" Appliance Contractors Appliance contractors are also paid reimbursement and remuneration in line with the Drug Tariff. Most of these products are subject to VAT and therefore, because the NHS is deemed to be the final consumer, VAT is paid on services and products supplied by appliance contractors. Appliance contractors are not paid an advance as the smaller number of claims allows NHS Prescription Service to process these within a month and pay on the 1st of the month following submission. The system for remuneration and reimbursement of appliance contractors is currently under review as it has remained unchanged for many years. Currently, the bulk of remuneration comes in the form of "oncost" on the price of a product. Remuneration is not subject to any overall total as in pharmacy (the global sum). The NHS price for the product is the list price. Unlike for pharmacies there is no recovery of any discount which may be available to the appliance contractor. Dispensing Doctors The basic premise is that these payments are calculated in a similar fashion to those for Pharmacists, however, there are some notable differences (e.g. dispensing doctors are not paid a container allowance). From April 2006 all dispensing doctors have to be VAT registered. The amounts payable in relation to the provision of drugs and appliances are calculated using the following information: Basic Price (Drug Tariff Part II, Clause 8, 10, 11, 13 & Part VII) Discount Scale (3.17 - 11.18%) (SFE, Annex G, Part 1) VAT Allowance (SFE, Paragraph 17.3 (c)) Dispensing Fees (SFE, Annex G, Part 2) Out of pocket expenses (Drug Tariff Part II, Clause 12) The following document has been produced to act as guidance for dispensing practices on what endorsements are required for reimbursement: Dispensing Endorsement Guidance for Dispensing Practices Another difference for dispensing doctors is that payments are made by PCTs from their nondiscretionary funds. Therefore there is no need for any additional payments authorised locally to be submitted to NHS Prescription Services. Personal Administration GP Claims Claims for personal administration can be infrequent and not on a monthly basis similar to other prescriptions, therefore there are no advance payments. The prescriptions are processed during the month they are received and information is sent to the PCT payment site for payments to be made. The payment is calculated similarly to dispensing doctors. There are several vaccines that doctors "personally administer" in high volumes such as influenza vaccination. The GP practice claims payment for these specific High Volume Vaccines using the form FP34D Appendix for Dispensing Doctors and FP34PD Appendix for Prescribing only Doctors. Local Supply or National FP10 Routes Many PCTs are considering the local supply of drugs as part of the Pharmacy in the future initiatives. Such schemes can have significant patient benefits but there are issues that PCTs will need to address before the final decision is taken. The list below identifies some of the issues that arise with such schemes. VAT - Some schemes may not allow for the zero rating of drugs supplied via an FP10. This should be checked with the local Customs & Excise office. National - The national reimbursement price is based on a ‘basket’ of supplier prices. Care needs to Pricing be taken to examine efficient purchasing is maintained for the whole NHS. A good deal done locally may adversely effect the national supply ‘price’. Legislation - The Medicines Act and Pharmaceutical regulations apply to the supply of all drugs. Ensure that the proposed scheme does not infringe any legislation. Fees and - Most fees are currently funded from central budgets not the prescriber. Schemes Charges approved by the DH may be able to access these funds Other Costs - Provision may need to be made for costs of distribution, administration and collection of patient charges as well as accounts currently paid to Appliance Contractors. VAT The following guidelines are intended to give an overview of the VAT position on dispensing drugs. It is not the purpose of NHS Prescription Service to offer specific VAT advice nor should any reliance be placed on the following statements without further investigation. Supply of drugs Generally the supply of drugs under NHS arrangements is a mixture of exempt and zero-rated supplies. The tax rate is affected by such things as to who and from whom the drug is supplied and the nature of the drug or appliance. Where drugs or appliances are supplied by a GP to a patient whom the GP is authorised to provide NHS pharmaceutical services, the supply is zero-rated. Zero-rating, however, does not apply to drugs or appliances supplied to other NHS patients or private patients. In certain circumstances the supply will be standard-rated. Supply of services The provision of pharmaceutical advice and medical treatment are exempt services, provided certain conditions are met. VAT and Pharmacy Contract Payments HM Revenue and Customs has issued guidance (VAT info sheet 04/06) to assist community pharmacy contractors to determine the VAT liability of the supplies they make when providing essential and advanced services under the national pharmacy contract. Where appropriate, it will also show the link between payments and their corresponding services, to assist pharmacies in valuing their supplies. In particular HMRC gives specific guidance regarding the Practice Payment and pharmacies will need to apportion the practice payment to reflect the different liabilities of the activities it supports. The Department of Health will advise the Pharmaceutical Services Negotiating Committee what proportion of the practice payment relates to each activity, and notify PSNC whenever those weightings change. Further information can be found on the HMRC website http://www.hmrc.gov.uk and the PSNC website http://www.psnc.org.uk Reimbursement of costs NHS Prescription Services reimburses the cost of drug supplies excluding VAT on the assumption that a contractor will recover any VAT on standard-rated supplies through the normal process. For dispensing doctors who all now have to be VAT registered an allowance is made for personally administered drugs and appliances which are standard-rated. This is not a VAT payment but a payment of an allowance to cover the net VAT incurred by the dispenser for these products. VAT registration Information for GPs on how to register for VAT, information about the VAT treatment of good and services they provide and advice about how much VAT can be recovered on purchases is available at the following link VAT recovery If VAT registered you are entitled to deduct input tax incurred on costs used in making taxable supplies. Input tax relating to the exempt supplies is not normally deductible. If the input tax relates to both taxable and exempt supplies, normally only the input tax related to the taxable supplies can be deducted. Under these circumstances you are said to be partially exempt for VAT purposes. Guidance on partial exemption and related calculations can be found in VAT Notice 706 ‘Partial Exemption’ Other related information VAT Notice 701/31 ‘Health and Care Institutions’ provides further information on this related subject in respect to hospitals and other care institutions and may contain some useful guidance. This information has been provided for general information and does not constitute advice. NHS Prescription Services does not take any responsibility for any loss as a result of the information provided and recommends that specialist VAT advice should be sought prior to making decisions regarding the VAT treatment of any transaction or your own VAT affairs. Home Oxygen Therapy Service Oxygen suppliers are now responsible for delivering an integrated oxygen service (i.e. cylinder, concentrator and liquid). The supplier will provide the home oxygen service ordered by clinical staff on a Home Oxygen Order Form (HOOF). The supplier will provide the equipment that best meets the clinical needs of the patient as indicated on the HOOF. The supplier is also responsible for arrangements for the payment of patient's electricity costs associated with use of equipment supplied. Each oxygen service supplier will be able to access NHS Prescription Services’ website and submit oxygen payment claims at any time within the first 10 calendar days of the month following that in which the home oxygen service has been provided. Part X of the Drug Tariff gives a guide to the Home Oxygen Therapy Service arrangements which have been in place since February 2006. The PCT where oxygen supply has taken place as part of the Home Oxygen Service is responsible for payment of that service and all costs are charged back to that PCT. Prescribing Information A full list of the paper and electronic reporting systems are available at the following link Information services. User defined reports are available to PCTs via the electronic systems. Prescribing information is drawn from the prescriber details found on each prescription. The only information that is available at this level concerns the reimbursement cost of the drug as some of the remuneration elements are based on the batch of prescriptions not the individual script. However, even at the reimbursement level the cost of a prescription is not always apparent. The cost of a drug to the NHS varies dependant upon where it was dispensed due to the discount scale. For performance management purposes it is important to reflect the cost of the same drug equally across all prescribers. Therefore two methods are employed; the first is to ignore discount and report the Net Ingredient Cost (NIC); the other is to average the discount claimed in a particular month across all drugs. Calculation of this average is not available when all the reports are produced and therefore can be the average of the previous month. The first method of showing NIC only is used in reports; the second method is used in budget reports, such as Prescribing Monitoring Documents (PMD). The costs of the same drug can vary therefore between months as the average discount shifts each month. Reports that show previous months data such as PMD use the latest average discount calculated for the month in question. Hospital Prescribing NHS Prescription Service also reimburses prescriptions that are prescribed by a NHS Trust but dispensed in a community pharmacy. The method of reimbursement is exactly the same as any other type of script, the differing treatment lies in the recharging to the prescriber. The drug cost is discounted by the average discount of the previous month and then a fee is calculated as accurately as possible on the particular script (no allowance is made for fees that relate to the size of the batch). If the prescription attracted a patient charge this would be offset against the charge. This treatment means that the full cost of the prescription (as opposed to the drug element only) is recharged to the prescriber. NHS Prescription Services invoices this recharge directly to the NHS trust. Drugs Bill Charging The total cost of drugs in any month is charged back to the prescriber on the basis of the cash paid out in that particular month. The payments in any one month are made up of the 80% advance and the balance of the previous months account. Therefore the charge is calculated on 80% of the drug cost (NIC less discount) for the current month and 20% of the previous month. Other costs that are not part of the performance reporting but are part of the drugs charge e.g. VAT, dentists prescribing etc. are prorated to PCTs on the basis of their share of the total drugs cost. The NHS Prescription Service produces a monthly schedule along with the Itemised Prescribing Payment (IPP) reports to the DH to enable them to charge individual PCT cash limits for this expenditure. The methodology for charging the drugs bill costs to PCT is in the NHS finance Manual under PCT detailed guidance