Clinical Pharmacokinetics Of
advertisement

Clinical Pharmacokinetics Of:
Presented by:
Dana Jehad Badawieha
Supervised by:
Dr. Rafiq Abou Shaaban
2000 - 2001
Back
1
Phenobarbital: is along-acting barbiturate used in the treatment of
seizure disorders, insomnia, and anixety. It’s commonly administered
orally, but it may be administered I.M & I.V. It is frequently
administered as the sodium salt, which is approximately 91%, when
phenobarbital is administered parenterally; it’s usually administered
at rate of no more than 50mg/min. to avoid toxicities associated with
the propylene glycol diluent.
Mechanism of action:
Phenoobarbital increases the seizure threshold by decreasing postsynaptic excitation by stimulation post-synaptic GABA-A receptor
inhibitor responses as a CNS depressant.
Administration and dosage:
(1)
for adults, phenobarbital is administered orally at 90-300mg ( in
three divided doses or as a single dose at bedtime)
(2)
For children, typically receive 3-6mg/kg daily in two divided
doses. Adjustment is made as needed.
(1)
Precautions and monitoring effects:
Phenobarbital produces respiratory depression, especially with
parenteral administration.
(2)
Phenobarbital should be used with caution in-patients with
hepatic desease who may need dose adjustments.
(3)
Phenobarbital has sedative effects in adults and produces
hyperactivity in children.
(4)
Abrupt discontinuation of phenobarbital produces withdrawl
convulsions. If the drug must be discontinoued, another
2
GABA-A agonist (e.g., benzodiazepine, and paraldehyde)
should be substituted.
Adverse effects:
The physican should be notified if any of the following adverse
effects occur: sore throat, mouth sores, easy bruising or bleeding,
and any signs of infection.
(One)
CNS effects agitation, confusion, lethargy, and
drowsiness. Patients should avoid alcohol and other CNS
depressants.
(Two)
Respiratory
effects
include
hypoventilation
and
apnea.
(Three)
Cardiovascular
effects
include
bradycardia
and
diarrhea,
and
hypotension.
(Four)
GIT
effects
include
nausea,
constipation. If GI upset is experienced, phenobarbital
should be taken with food.
(Five)
Hematologic effects include megaloblastic anemia
after chronic use ( a rare side effect)
Significant ineractions:
(1)
antiepileptic drugs, such as valproic acid and phenytoin,
increase
the
level
of
phenobarbital
(decrease
metabolism)
(2)
Other drugs, such as acetazolamide, chloramphenicol,
cimetidine
and
phenobarbital
pyridoxine,
furosemide
(decrease
and
ethanol
3
increase
the
metabolism).
decrease
the
level
of
Rifampin,
level
of
phenobarbital (increase metabolism).
Key parameters:
Therapeutic plasm concentrations
10-30mg/L
Bioavailability (F)
>0.9
S ( for Na salt)
0.91
Vd
0.6-0.7L/kg
Cl:
For children
8ml/kg/hr
0.2L/kg/day
For adults
4ml/kg/hr
0.1L/kg/day
fraction free ()
0.5
t1/2:
For children
2.5 days
For adults
5days
Volume of Distribution (Vd)
The volume of distribution for Phenobarbital is approximately 0.7
L/kg8.9
Clearance (Cl)
Phenobarbital is primarily metabolized by the liver; <20% is
4
eliminated bby the renal route. The average total plasma
clearance for Phenobarbital is 4 mL/kg/hr or 0.1 L/kg/day. This
clearance value of approximately 0.1L/kg/day results in the
following clinical observation:
For every 1 mg/kg/day of Phenobarbital administered, a steadystate Phenobarbital level of about 10 mg/L is achieved.
Cpss ave
= (S)(F)(Dose/t)
C1
= (0.9)(1 mg/kg/day)
0.1L/kg/day
= 9 mg/L or ~10 mg/L
This
clinical
guideline
suggests
that
in
adult
patients,
maintenance doses of 2 mg/day/kg should result in steady-state
concentrations of ~20 mg/L. The clearance in children 1 to 18
years of age is approximately twice the average adult clearance).
Therefore,
they
generally
require
maintenance
doses
of
Phenobarbital that are about twice those of the average adult,
therefor, they require maintenance dose of 4 to 5 mg/kg/day will
be needed to achieve steady-state plasma concentrations of 20
mg/L.
Half-Life (T1/2)
The plasma half-life of Phenobarbital is five days in most adult patients, but may be as short as two to three days in some
5
individuals, especially children.
Time to Sample
Phenobarbital has a half-life of approximately five days; as a
result, plasma samples obtained within the first one to two weeks
of therapy yield relatively little information about the eventual
steady-state concentrations. For this reason, routine plasma
Phenobarbital concentrations should be monitored two to three
weeks after the initiation or a change in the Phenobarbital
regimen. Plasma samples obtained before this time should be
used either to determine whether an additional loading dose is
needed (e.g., when plasma concentrations are much lower than
desired), or whether the maintenance dose should be withheld
(e.g., Phenobarbital concentrations are much greater than
desired).
Once steady state has been achieved, the time of sampling
within a dosing interval of phenobartial is not critical; plasma
concentrations can be obtained at almost any time relative to the
phenobarbital dose. As a matter of consistency, how ever, trough
concentration are generally recommend and if phenobarbital is
being adminisered by the intravenous route, care should be taken
to sample at least one hour after the end of the infusion to avoid
the distribution phase.
6
Case# 1: patient with generalized sizures, in which he sustained
head
injuries.
Required
knowing
the
loading
dose
of
phenobarbital with 20mg/L of plasma level.
Case #2: required the maintenance dose with 20mg/L of
phenobarbital concentration.
Case #3 : required the time to achieve a mininmum therapeutic
level of 10mg/L, if not receive the loading dose & the time to
achieve asteady-state level of 20mg/L.
Case #4: patient admitted for poor seizure control, required the
final steady-state concentration on the present regimen
Case #5: patient with seizure disorder secondary required
knowing the phenobarbitone concentratoin.
Case #6: required to know the most appropirate method to
adjust pharmcokinetic parameters if phenobarbital concentration
= 29mg/L
Case #7: required to know a revised plasma concentration,
using anon-steady state continous infusion model
Case #8: epileptic patient developed to hypoalbuminemia
secondary to nephrotic syndrome, required to know if his
7
phenobarbital concentration be affected by decreases in his
albumin concentration or renal function.
Case # 9: patient with chronic renal failure and a seizure
disorder. Required to know the maintenance regimen of the
patient
Case # 10: patient with seizure disorder, required to know the
maintenance dose of sodium phenobarbital that produce a steadystate conc. Of ~20mg/L.
Case #1
A 39-year-old, 70 kg male, developed generalized seizures several
Months after an automobile accident in, which he sustained, head
injuries. Phenobarbital is to be initiated. Calculate a loading dose
of Phenobarbital that will produce a plasma level of 20 mg/L.
Since this is a loading dose problem and there is no existing initial
drug concentration:
Loading Dose =
(Vd) (Cp)
(S)(F)
If F and S are assumed to be 1.0 and the volume of distribution is
assumed to be 0.7 L/kg or 49 L, (o.7 *7):
Loading Dose
= (49 L)(20 mg/L)
(1.0)(1.0)
= 980 mg or ~ 1 gm
8
It may be administered orally, intramuscularly, or intravenously.
Generally, the loading dose is divided into three or more portions
and administered over several hours. It is done as a precaution
against toxicity should a two-compartmental distribution exist or
to avoid cardiovascular toxicity from the propylene glycol diluents
in the injectable dosage form.
Case #2
Calculate an oral maintenance dose, which will maintain a
Phenobarbital concentration of 20 mg/L. how should the dose be
administered?
Since clearance is the major determinant of the maintenance
dose, this parameter must be estimated expected clearance for
patient who is 70 kg:
Clearance Phenobarbital = (0.1/kg/day)(Weight in Kg)
= (0.1 L/kg/day)(70 kg)
= 7.0 L/day
If S and F are assumed to be 1.0, the maintenance dose of
Phenobarbital can be calculated using:
Maintenance Dose
= (Cl)(Cpss ave)(t)
9
(S)(F)
= (7 L/day)(20 mg/L)(1 day)
(1.0)(1.0)
= 140 mg
In practice, the daily dose is usually divided into two or more
portions; however, with a half-life of five days, once daily dosing
should suffice:
t1/2
= (0.693)(Vd)
Cl
= (0.693)(49 L)
7.0 L/day
= 4.85 days or ~5 days
The calculated dose corresponds to an empiric clinical gguideline
which has been used for many years: The Phenobarbital steadystate level produced by a maintenance dose will be approximately
equal to ten times the daily dose in mg/kg:
Maintenance Dose (mg/kg)
= 140 mg
70 kg
= 2mg/kg
According to the clinical guideline, the level in mg/L produced by
this dose will be 20 mg/L (2 X 10).
Case #3
If does not receive a loading dose, how long will it take to achieve
a minimum therapeutic level of 10 mg/L following the initiation of
the maintenance dose? How long will it take to achieve a steadystate level of 20 mg/L?
10
The half-life for Phenobarbital is approximately ffive ddays as
calculated in case 2. If it takes three to five half-lives to approach
steady state, approximately 15 to 20 days will be required to
achieve the final plateau concentration of 20 mg/L. Because the
minimum therapeutic concentration of 10 mg/L is one-half of the
predicted steady-state concentration of 20 mg/L, one half-life or
five days will be required for the Phenobarbital concentration to
accumulate to 10 mg/L.
Kd = 0.693
t1/2
= 0.693
5 days
= 0.139 days-1
Cp1
= (S)(F)(dose/t) (1- e-kdt)
Cl
= (20mg/L)(0.5)
= 10mg
Case #4
A 62-year-old, 57 kg female, was admitted for poor seizure
control. Prior to admission she had been receiving an unknown
dose
of
phenobarbitaL
On
admission,
tthe
phenobarbital
concentration was 5 mg/L, and she was started on 60 mg of
11
phenobarbital Q 8 hr (180 mg/day). Five days later, the
phenobarbital concentration was measured and reported as 17
mg/L. Calculate her final steady-state concentration on the
present regimen.
There are several ways of approaching this case. Since Cpss ave is
defined by clearance, one could use the average clearance for
phenobarbital (0.1 L/kg/day x 57 kg = 5.7 L/day)
and insert this value into:
Cpss ave = (S)(F)(Dose/t)
Cl
= (1)(1)(180 mg/day)
5.7 L/day
=
31.6 mg/L
Another method could be used to estimate the steady-state value.
The concentration of 17 mg/L reported on the fifth day is
assumed to represent the sum of the fraction of the initial
concentration (5 mg/L) remaining at this point in time plus the
accumulated concentration resulting from five daily doses of 180
mg. If half-life for phenobarbital is five days, the fraction oof the
initial concentration remaining after one half-life will be 0.5 and
contribution to the reported concentration at five days will be 2.5
mg/L. The remaining portion of the reported concentration (14.5
12
mg/ L) represents 50% of the steady-state level, which will be
produced by the 180-mg/day dose. Therefore, the predicted Cpss
ave would be 29 mg/L (2 x 14.5 mg/L).
One also could use the empiric clinical guideline discussed in
Question 3 regarding the prediction of Cpss ave from the mg/kg
dose of phenobarbital. In this case the mg/kg dose would be
180-mg/57 kg or 3.16 mg/kg. The predicted Cpss ave would be
31.6 mg/L (3.16 X 10).
Case#5
A 35-year-old, 80 kg male, is being treated for a seizure disorder
secondary to a motor vehicle accident. He has been receiving
200 mg/day of phenobarbital (100 mg BID) for the past 15 days.
The phenobarbital serum concentration jjust before the morning
dose on Day 16 was reported tto be 29mg/L. Calculate the
phenobarbital concentration yyou would have predicted on that
day.
The average pharmacokinetic parameters for N.P. are as follows:
Cl =8L/day (0.1 L/kg/day x 80 kg); Vd = 56 L (0.7 L/kg x80 kg);
Kd = 0.143 days1 and t1/2 = 4.9 days.
Kd
= C1
Vd
13
= 8 L/day
56 L/day
= 0.143 day-1
t1/2
= 0.693
Kd
=
0.693
0.143 day-1
= 4.85 days
Since he has been receiving his Phenobarbital maintenance dose
for 15 days or approximately three half-lives, the phenobarbital
concentration is assumed to be a steady-state level. the steady
state trough level should be approximately 24 mg/L based upon
the calculation below.
Cpss min = (s)(F)(dose)/Vd (e-kdt)
(1 — eKdt)
= (1)(1)(100 mg)/56 L (e-(0.143)(0.5 days))
(1-e-(0.143 day-1)(0.5 days))
= [1.78 mg/L] [0.93]
0.069
= [25.9][0.93]
=
24 mg/L
Case #6.
Considering the measured phenobarbital concentration of
29 mg/L, what method is most appropriately uused to adjust his
14
pharmacokinetic
parameters?
Do
these
patient-specific
parameters suggest that a maintenance ddose adjustment is
necessary
if
the
goal
is
to
maintain
tthe
phenobarbital
concentration at ~25 mg/L?
The measured trough concentration of phenobarbital is greater
than the predicted
concentration;
therefore,
phertobarbital
clearance is likely to be lower than expected. If this is true, then
his phenobarbital half-life is likely to be longer than five days, and
a non-steady-state approach will have to be used to revise his
clearance value.
t1/2 = (0.693)(Vd)
Cl
Although there are a number of models which describes tthe
concentration (Cp2) following the Nth dose:
Cp2 =
(S)(F)(Dose)/Vd (1-e-kd (N) t)(e-kdt2)
(1 — e-kdt)
In order to calculate the concentration at the time of sampling
(Cp2), the elimination rate constant will have to be adjusted first
by reducing the expected clearance value
Kd = Cl
Vd
Unfortunately, there is not a direct solution to this problem, and a
trial and error method must be used to find the clearance value,
15
which will predict the observed phenobarbital concentration of
29 mg/L. For example, if a phenobarbital clearance of 6 L/day,
elimination rate constant of 0.107 days is calculated. This
elimination rate constant results in an expected phenobarbital
concentration of approximately 26 mg/L.
Kd =Cl
Vd
= 6 L / day
56 L
= 0.107 day-1
Cp2= (S)(F)(Dose) / Vd (1-e-kd (N) t)(e-kdt2)
(I — e-kdt))
=
=
=
(1)(1)(100 mg) / 56 L (1-e-(0.107 days-1)(0.5 days))
(1-e-(0.107 days-1)(0.5 days))
(1-e-(0.107 days-1)(0.5 days))
1.78 mg / L (1 — 0.2)(0.948)
(0.052)
25.9 mg/L or ~ 26 mg/L
Further decreasing the phenobarbital clearance to 5 L/day results
in an elimination rate constant of 0.0893 days & when this
elimination rate constant, a phenobarbital cconcentration oof
28.7mg/L is calculated.
Kd =
Cl
Vd
= (5 L / day) / 56 L
=
0.0893 days-1
16
Cp2 = (S)(F)(Dose)/Vd (1-e-kd (N) t)(e-kdt2)
(1 — e-Kdt)
= 1.78 mg/L (0.738)(0.956)
(0.0437)
28.7 mg/L or ~29 mg/L
=
The convergence of the predicted and observed plasma concentration suggests that phenobarbital clearance is approximately 5
5L/day. Assuming that this clearance is reasonably accurate, the
predicted steady-state phenobarbital concentration would then be
approximately 40 mg/L on the current dosing regimen of
200 mg/day as calculated below.
Cpss ave = (S)(F)(Dose/t)
Cl
= (1)(1)(200 mg / 1 day)
5 L / day
=
40 mg/L
If a steady-state concentration of approximately 25 mg/L is desired, a reduction in the maintenance dose to approximately
125 mg/day would be necessary as shown below:
Maintenance Dose = (Cl)(Cpss ave)(t)
(S)(F)
= (5 L/day)(25 mg/L)
(1)(1)
= 125 mg/day
Since revised phenobarbital clearance is based upon a measured
17
drug level obtained at less than two half-lives (i.e., 15 days) after
therapy was initiated, the revision and expected steady-state
concentration must be considered somewhat uncertain.
t1/2 = (0.693)(Vd)
Cl
= (0.693)(56 L)
5L/day
= 7.8 days
While it may be appropriate to reduce the phenobarbital dose,
additional plasma level monitoring will be necessary in 24 to 40
days to ensure that the steady-state concentration is actually
about 25 mg/L on a daily dose of 125 mg.
Case #7.
Calculate a revised plasma concentration, using a non-steady
state continuous infusion model.
A continuous infusion model is usually satisfactory when predicting steady-state phenobarbital plasma concentrations because
of the relatively long half-life and short dosing interval for
phenobarbital.
In this case the equation will have to be used because the
phenobarbital concentration was obtained before steady state
had been achieved.
Cp1 = (S)(F)(Dose/t) (1- e-kdt2)
18
Cl
An important to multiply the duration oof the infusion (t1) by the
infusion rate. This product should equal the total amount of drug,
which has been administered to the patient. For example, in the
infusion rate of 100 mg divided by 0.5 days times duration of the
infusion of 15 days results in a total administered dose of 3000
mg.
Total amount of Drug administered = (Dose/t)(t1)
= (100mg/0.5days)(15days)
= 3000mg.
Early in a regimen; the total amount of drug administered and
the duration of the theoretical infusion are somewhat disparate.
For example, immediately after the administration of the second
phenobarbital dose, a total of 200 mg has been administered,
while the total time elapsed is only one-half day. However,
suggests that only 100 mg have been administered. Wwhile this
problem is most apparent early in therapy, it is seldom an issue
after multiple doses has been administered. This is because a
variation in one dosing interval represents a relatively small
percentage error with respect to the total amount of drug
administered.
The
previously
calculated
clearance
of
5L/day,
and
the
corresponding elimination rate constant of 0.0893 day-1, a
phenobarbital concentration of 29.6 mg/L is calculated.
19
Cp1 =
(I)(1)(100 mg/0.5 days) (I — e–(t) 0.0893) (15 days))
5 L/day
=
40 mg/L (0.74)
=
29.6 mg/L
The similarities between the predicted phenobarbital concentration using the continuous infusion and the intermittent bolus
model suggest that either model could be used, with the continuous infusion model requiring fewer computations.
Case #8.
an epileptic male who has been managed cchronically on
phenobarbital 120 mg/day, has recently-
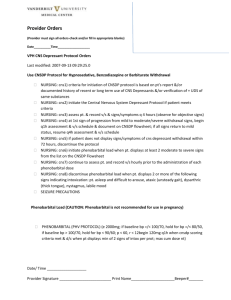
In
this
figure
Plasma
Concentration-Time Curve for the
Accumulation
and
Eventual
Affainment of Steady State for a
Drug Administered With a Dosing
CP
Interval That Is Much Shorter Than
the Elimination Half-Life. The solid
smooth
line
accumulation
represents
pattern
during
the
a
continuous input model. ond the
sow-toothed pattern indicates the
Time
accumulation pattern for a drug
intermittently.. Note
Cp1 = (S)(F)(Dose/t) (1 — e-kdt1administered
)
that the plasma concentrations preCl
dicted by the intermittent Input
Cp2 = (S)(F)(Dose)/Vd (1- e-kd
(N) t)(e-kdt2) to
model ore very similar
(1-e-kdt)
accumulation pattern
of
continuous input model.
20
the
the
Developed hypoalbuminemia secondary to nephrotic syndrome.
Will his phenobarbital concentration be affected by decreases in
his albumin concentration or renal function?
Only 40% to 50% of phenobarbital is bound to plasma proteins;
therefore, alpha (the fraction of phenobarbital that is free) is 0.5
to 0.6 The concentration of a drug that is bound to protein to the
extent of 50% or less is not likely to be significantly affected bby
changes in plasma protein concentrations or protein binding
affinity.
The renal clearance for phenobarbital is probably <20% of the
total clearance in patients with normal renal function and an
uncontrolled urine pH (e.g., the urine pH is not intentionally
adjusted). Therefore, it is unlikely that patients with renal failure
will require significant adjustments in their phenobarbital dosage
regimens.
To summarize, phenobarbital concentrations are not likely to be
significantly affected by his hypoalbuminemia or poor renal
function.
Case #9.
A 25-year-old, 70-kg male with chronic renal failure and a seizure
disorder. He has been maintained oon 660 mg of phenobarbital
BID and has steady-state concentrations of 20 mg/L. Over the
21
past three months, his renal function has progressively worsened
and he is to be started on four hours of hemodialysis three times
weekly. Will he require an adjustment of his maintenance
regimen?
To determine whether a significant amount of drug is lost during
each dialysis period, the three steps outlined in Part I: Dialysis of
Drugs should be examined. First, the apparent volume of distribution for unbound drug should be estimated. Using a volume
of distribution of 0.7 L/kg or 49 L for this
70-kg patient and a free fraction or alpha of 0.5 for phenobarbital,
the apparent unbound volume of distribution for phenobarbital in
is approximately 98 L. Since this is less than the upper limit of
250L for a dialyzable drug, dialysis possibly could remove a
significant amount of phenobarbital.
Unbound Volume of Distribution = Vd
= 49/0.5
= 98 L
Clearance of phenobarbital must be estimated next. The usual
clearance of 0.1L/kg/day, or 7L/day for the 70-kg patient,
represents a total body clearance of approximately 5 mL/min.
This value is low enough (i.e., <500 to 800 mL/min) that dialysis
could significantly increase the total clearance.
Clearance (mL/min) =
[7L/day] (1000ml/L)
1440min/day
=
4.9 mL/min or ~5 mL/min
22
Finally, estimate the drug’s half-life using. The apparent hhalf-life
for phenobarbital of approximately five days is much longer than
the lower limit of one to two hours set in Criterion 3 (i.e.,
hemodialysis is unlikely to significantly alter the dosing regimen if
the drug half-life is very short).
t1/2
=
(0.693)(Vd)
Cl
=
(0.693)(49 L)
7 L/day
=
4.9 days
Since the unbound volume of distribution and Phenobarbital
clearance of R.T. are relatively small, and the half-life is much
greater than the lower limit of one to tWo hours, a significant
amount of phenobarbital could be cleared during a dialysis period.
For this reason, the actual clearance of phenobarbital during
hemodialysis will have to be determined.
The clearance of phenobarbital by hemodialysis has not been
studied extensively; however, the use of hemodialysis in the
treatment of two phenobarbital overdoses indicates that the
clearance of phenobarbital by hemodialysis is approximately
23
3L/hr. If this value is inserted along with the patient’s calculated
clearance (Clpat) of 0.25 L/hr,
Cl
=
(S)(F)(Dose/t)
Cpss ave
=
(1)(1)(60 mg/0.5 day)
20 mg/L
=
6 L/day or 0.25 L/hr
A dialysis replacement dose can be calculated.
Because of the
long half-life and relatively short dosing interval for phenobarbital
Post Dialysis = (Vd)(Cpss
ave)
{1- e-[(Clpat + Clphe)/Vd] (T)}
Replacement
Dose
= (980 mg)(1 — 0.77)
= (980 mg)(0.23)
= 225.4 mg
This replacement dose of approximately 225 mg represents the
amount of drug eliminated from the body during the dialysis
period by both metabolic and dialysis clearance. The vast majority
of the drug eliminated during the four-hour dialysis period
represents drug eliminated by the dialysis route. For this reason,
the total daily phenobarbital dose on days of dialysis would be
24
120 mg (maintenance dose) plus the postdialysis dose
Of ~200 mg.
Standard replacement doses of phenobarbital after dialysis are
frequently in the range of 200 to 300 mg. While this replacement
dose appears to be large when compared to the maintenance
dose, it is not unusual. If there is concern about the size of the
postdialysis replacement dose, one could administer a smaller
dose of 100 to 200 mg after dialysis and continue to monitor the
patient during subsequent dialysis periods to ensure that the
phenobarbital concentration does not continue to decline due to
additional elimination by the dialysis route.
Case #10.
A 5-year-old, 20 kg male, is to be started on phenobarbital for his
seizure disorder. Calculate the maintenance dose of sodium
phenobarbital that will produce steady-state concentration of ~20
mg/L.
In order to calculate, phenobarbital maintenance dose, one would
first assume his clearance to be =2 L/day (0.2 L/kg/day X 10 kg).
This clearance value, while larger than the usual adult value, is
consistent for children. With a target concentration of 20 mg/L,
and a salt form (S) fraction 0of 0.9, a daily maintenance dose
Of~ 40 mg can be calculated.
Maintenance Dose = (Cl)(Cpss ave)(r)
(S)(F)
25
=
(2 L/day)(20 mg/L)(1 day)
(0.9)(1)
=
44.4 or ~40 mg
Depending upon the clinical situation, one dould administer a
loading dose to rapidly achieve therapeutic concentrations or
start the patient on his maintenance dose without a loading dose.
In the latter situation, the urgency of the clinical situation will
determine whether the initial maintenance dose should be
40mg/day or one quarter of the target maintenance dose
(10 mg/day) for the first week, increased by 10 mg/day weekly
until the final maintenance dose of 40 mg/day is being administered. As noted previously, excessive sedation can be a consequence of starting the patient on the full maintenance dose.
Should be monitored for both therapeutic and potential side
effects during this period of dose titration.
Back
26