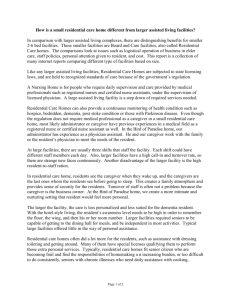
Residential Care for Individuals with Developmental Disabilities
advertisement

Issues in Residential and Community Based Care 1 Legal Nurse Consulting Principles, 3rd Edition Vol. 2 Chapter 22 Issues in Residential and Community-Based Care Laura E. Fox Fox Associates 7950 Kelly Ann Ct Fairfax Station, VA 22039 (703) 250-9369 (work) Lfox98@cox.net Dawn D. Nash American Baptist Homes of the Midwest 8780 75th St S Cottage Grove, MN 55016 (952) 807-8006 (work) (952) 941-8567 (fax) dnash@abhomes.org Dawn D. Nash, RN, obtained her Registered Nursing Diploma from Arthur B. Ancker School of Nursing, in St. Paul, Minnesota. She is currently employed as the Director of Clinical Services for American Baptist Homes of the Midwest in Eden Prairie, MN. She has over 33 years of long term care nurse management and consulting experience. Need Fox’s bio in a format I can read. 1 Issues in Residential and Community Based Care 2 Chapter 22 Residential Care for Individuals with Developmental Disabilities Contents Objectives Introduction Definitions Overview of Residential Care Current Issues Legal/Ethical issues LNC Role Case examples Chapter Summary References Resources Objectives: To define the trends for long term care for individuals with DD To describe two roles of the LNC in assisting attorneys with long term care cases for individuals with DD To identify areas in long term care for individuals with DD that need monitoring by the LNC Introduction Residential care for people with developmental disabilities (DD) requires special expertise and knowledge for the legal nurse consultant (LNC). The LNC needs to know about the unique needs of people with DD, including health care issues. The LNC needs knowledge on the residential care system for people with DD, the various options available, the regulatory agencies, and standards of practice. The residential care system for people with DD is a field unto itself that varies from State to State. Because people with DD are a diverse group, the residential setting needs to be able to provide for individualized needs that are dynamic and changing over the person’s life. The LNC in 2 Issues in Residential and Community Based Care 3 this field needs experience with the medical and legal aspects of long term care specific for individuals with DD. The LNC is often contacted by an attorney when an individual or groups of individuals with DD living in residential care sustain an injury or insult. These injuries may have occurred because the care was believed to be sub-standard. The attorneys often cite nursing home and/or hospital standards of care and are unaware that most people with DD reside in the community and in small group homes that are regulated at the local, state and/or federal level. These standards are not nursing home or hospital standards and the same standards of care cannot be applied. The LNC will need to be aware of the trends in long-term care for individuals with DD, the applicable standards of care, the different types of facilities, and issues that frequently arise. Definitions DD is a broad term that refers to a variety of conditions and describes an individual’s functional limitations in society and daily life. According to the Developmental Disabilities Assistance Act and Bill of Rights Act (2000) a developmental disability is a chronic, severe disability which: -Is attributable to a mental or physical impairment of a combination of mental and physical impairment -Occurs before the individuals reaches age 22 -Is likely to continue indefinitely -Results in substantial functional limitations in three or more of the following areas of major life activity: (i) self care, (ii) receptive and expressive language, (iii) learning, (iv) 3 Issues in Residential and Community Based Care 4 mobility, (v) self-direction, (vi) capacity for independent living, and (viii) economic selfsufficiency; and -Reflects the individual’s need for a combination and sequence of special, interdisciplinary or generic care, individualized supports, or other forms of assistance that are of lifelong or extended duration and are individually planned and coordinated The federal definition of DD is based on an individual’s functional abilities with self-help skills and/or activities of daily living. The federal definition of DD encompasses many different disabilities, which may include cognitive disabilities, physical disabilities or both including but not limited to autism, Down syndrome, cerebral palsy, spina bifida, mental retardation and epilepsy. According to the Administration on Developmental Disabilities, there are approximately 4.5 million individuals with DD in the United States (Administration on Developmental Disabilities, 2008). There is not one standard definition of DD. The federal definition of DD is not uniformly accepted and the States use different definitions for DD based on the federal law. Many States use a diagnosis of mental retardation (MR) as the primary eligibility criteria. The Diagnostic and Statistical Manual of Mental Disorders 4th edition defines MR as sub average general intellectual functioning and significant limitations in adaptive functioning in two skills areas. Sub average intellectual functioning is defined as an IQ of about 70 or below, approximately 2 standard deviations below the mean, starting before the age of 18 (American Psychiatric Association, 2000). By using this definition, only individuals with mental retardation are eligible for services, and individuals with cerebral palsy and/or seizure disorders without the diagnosis of mental retardation may not be eligible for State DD services and supports. In California the Lanterman Act 4 Issues in Residential and Community Based Care 5 defines a developmental disability as starting before the age of 18 (California Lanterman Developmental Disabilities Services Act, 1976). Using this definition, an individual who receives a diagnosis of traumatic brain injury from a motor vehicle accident at age 20 would not be eligible for services and supports through the California DD system. Because people with DD are a diverse group and the definition incorporates many different conditions and disabilities, it is important that the LNC is aware of the individual’s diagnoses and the definition for services where the individual resides. DD is a more specific definition than chronic conditions or the term disabilities (ANA, 2004). People with DD often need a combination of developmentally appropriate, interdisciplinary and individualized supports and services throughout their life. This information will be further needed when the LNC evaluates the level of care and individualized services in the community. Overview of Residential Care For many years, people with DD were isolated from the community and either lived at home or were sent away to large State Institutions often called State Developmental Centers. People with DD were seldom mainstreamed in the community. By the mid-20th century, the focus was on normalization and providing care in the least restrictive environment. Normalization is used “to provide a supportive environment for persons with intellectual and DD to make decisions regarding activities of daily living and to live as close as possible to the norms and patterns in the mainstream of the society in which they reside” (ANA, 2004, p. 53). The concept of normalization and living in the 5 Issues in Residential and Community Based Care 6 least restrictive environment started to replace the idea of segregated institutional settings for people with DD located in the outskirts of the community. A major de-institualization effort took place in the 1980s. This effort was fueled with media investigations exposing poor conditions in institutional settings and resulted in federal class action litigation demanding the people with DD be integrated into community settings. The transition from state institutions to the community varied from state to state (Nehring, 2003: Smith, 2006). Class action litigation continues to be a major force influencing community care options. Olmstead v. L.C. (1999) is considered a landmark Supreme Court ruling in support of community care for people with DD. In this case, two women living in a State institution in Georgia, determined to be appropriate for community care placement, were denied residential placement. The State argued it was unable to afford to provide these services. The decision by the Supreme Court in Olmstead v. L.C. under Title II of the Americans with Disability Act (ADA) of 1990 stated that unnecessary institutional segregation constitutes discrimination that cannot be justified by a lack of funding. States are required to place individuals with DD in community settings when: (1) the state’s treatment professionals have determined that community placement is appropriate; (2) transfer from institutional care to the least restrictive environment is not opposed by the individual; and (3) the placement can be reasonably accommodated, taking into account the resources available to the state and the needs of others with mental disabilities. Olmstead requires the states to address community care in light of ADA integration. The aftermath of the Olmstead decision has resulted in many class action lawsuits for people with DD to receive long-term care services in the community. Litigation also addresses 6 Issues in Residential and Community Based Care 7 the issue of waiting lists that result in a denial of services. In 2006, 42 states reported that 64,990 persons with DD were on waiting lists for residential services (Braddock, Hemp & Rizzolo, 2008). The States cite that these services are not being provided because they lack adequate funds. Other lawsuits are being filed for individuals with DD that challenge the Medicaid services that they did or did not receive in the community. Residential and Community Care Settings There are many available residential and long term care options for people with DD. These settings include State Developmental Centers, often called State Institutions, Intermediate Care Facilities for the Mentally Retarded (ICF/MR), and Home and Community Based Service Waiver Homes (HCBS). These small ICF/MRs and HCBS Waivers homes are often called group homes. Group homes are funded by a variety of sources, however the vast majority are funded by Medicaid, using a combination of federal and State funds. There has been a continual increase in residential out-of-home placements with an increase of 4.8% in 2004-2005 with 536,476 people with DD in residential care (Braddock, et. al., 2008). The large State Developmental Centers were the backbone of the DD model. They offer a centralized model of services provided by the State. However, as the trend in long-term care for individuals with DD shifted to community and small group homelike settings, the State Developmental Centers have been closed or downsized. The individuals remaining have profound DD that require extensive medical care, including 24-hour nursing care, or significant behavioral concerns (Palley & Van Hollen, 2000). Males made up the majority of the population (Pouty, Smith & Larkin, 2007). In 2006, 7 Issues in Residential and Community Based Care 8 42 states continue to have state-operated institutions, while 8 states and the District of Columbia no longer have these state-operative institutional facilities (Braddock et. al., 2008). The majority of people with DD now reside in the small group home settings such as the ICF/MRs and the HCBS Waiver program. The ICF/MR statute was enacted in 1971 from the Social Security Act (PL 92223). It is based on a medical model and requires “active treatment.” The ICF/MRs must comply with federal regulations found at 42 CFR Part 483, Subpart I, Sections 483, 400493.490 and specified in eight areas that include management, client protections, facility staffing, active treatment services, client behavior and facility practices, health care services, physical environment, and dietetic services (wwwcms.hhs.gov). There are currently 7,400 ICF/MRs in the United States serving 129,000 people (Department of Health & Human Services, 2008). Many of these people have MR, are also non ambulatory, have seizure disorders, behavior problems, mental illness, are visually and/or hearing impaired, or have a combination of these conditions. ICF/MRs range in size and may be large facilities or small six bed homes. With the trend for smaller homelike settings, there has been a decline in the larger settings, and a growth in six people or less for ICF/MRs (Braddock et al., 2008). ICF/MRs may be operated by the State, or by private agencies, and may be for profit or non-profit. ICF/MRs are always residential and are regulated by the federal ICF/MR Standards through the Center for Medicare and Medicaid Services. The HCBS Waiver program was designed for people with DD to remain in the community with supports without having to meet all the federal regulations of the ICF/MRs. Congress first authorized the HCBS Waiver program in 1981 as an 8 Issues in Residential and Community Based Care 9 alternative to the ICF/MR program. Section 1915 (c) of the Social Security Act enables State to request a waiver of applicable federal Medicaid requirements to provide community support services for those individuals who would have required institutional care. The residential model is generally limited to four or fewer individuals in the residential home. The program needs to demonstrate cost neutrality, as the cost for Waiver services must not exceed the cost of the institution. The HCBS Waiver is now the principal Medicaid program for people with DD. In fiscal year 2007, the HCBS Waiver exceeded $20 billion and paid for 5.2 times as many people with DD as the ICF/MR Waiver (Lakin, et. al., 2008). The State agencies receive the HCBS Waiver funding for services and private agencies; both for-profit and non-profit agencies provide the direct services. To receive the HCBS Waiver funds, a state submits an application to Health and Human Services (HHS), identifies the target population, identifies the number of people they will serve and list the services that will be provided. Federal regulations specify that the State has (1) adequate standards for all providers of services and (2) assurance that any state licensure of certification requirements for providers of waiver services are met. States must annually report on the implementation, monitoring, enforcement of their health and welfare standards and the HCBS Waiver’s impact on the health and welfare of the individuals. The HCBS Waiver offers a cornucopia of community based services and supports for people with DD that may include case management, habilitation training, various professional therapies, behavior management, etc. These services and supports are determined by the needs of the individual, and they differ between States, and only some 9 Issues in Residential and Community Based Care 10 of the options are funded by each state (Braddock et al., 2008). Regulations are less prescriptive, allowing for “person-centered and person-driven” planning, focusing more on outcomes, rather than meeting a prescribed treatment approach. Oversight of the HCBS Waiver program is often decentralized among a variety of agencies and rarely is one agency accountable for the overall quality of care provided. Some waiver service providers are regulated by state licensing agencies, others by private accreditation organizations and others operate under a contract or other agreement with a state agency with the vast majority provided by non-state agencies (Pouty, et al., 2007). Current Issues The smaller residential settings (ICF/MR and HCBS) are based on the normalization model. Adults with DD have rights and responsibilities, as the general population, however they may need additional supports to live safely and successfully in the community. They work either independently or in sheltered settings or day programs and are not at home during the day. They may have different diagnoses and different strengths and needs for services and supports. The residents have opportunities to interact with the community and work on independent skills. The residents have annual goals often outlined in an Individualized Habilitation Plan or Individualized Service Plan. They have regular visits to physicians and/or specialist. Residents have rights, which often have to be negotiated within the guidelines of the residential home. People with disabilities need to receive services in settings of their choices. Bannerman, Sherldon, Sherman & Harchik (1990) described personal choices as the rights of people with DD to eat too many doughnuts. 10 Issues in Residential and Community Based Care 11 Adults with DD have the same medical issues as the majority of the population. They may have additional concerns and increased health care needs based on their functioning abilities and/or based on their diagnosis. People with DD, as the general population, often struggle with chronic conditions such as obesity, diabetes, high blood pressure, etc., and these issues may be further exacerbated by their functional limitations, for example, if the person is non ambulatory. They also may have extra medical issues, such as individuals with Downs Syndrome, who show physical signs of aging often 20 years earlier, including Alzheimer’s (Service & Hahn, 2003). People with DD have the same age-related impairments and illness as people without disabilities. As our society ages, this population will also age, and will need health care services, including preventative health assessment. The aging of our society directly influences the demand for residential services. As the population ages, there will be an increased need for out-of-home long-term residential care services for all persons, including individuals with DD. Currently the majority of individuals with DD are living at home, with their aging parents (Palley & Van Hollen, 2000: Parish & Lutwick, 2005). It is anticipated that the future demand for services will far exceed the supply. The DD system competes with the general population for services and supports, including the need for care providers and community homes. States have been experiencing an increase in the number of individuals with DD seeking community-based services, and have been unable to keep up with the growing demand (Smith, 2006). It is anticipated this trend will continue. 11 Issues in Residential and Community Based Care 12 Regulations on the Federal and State Level Attorneys who contact a LNC generally want information regarding the standard of care. Frequently the situation that occurs is that a person with DD has a change in their medical condition, which goes unrecognized or is ignored by the residential facility, and by the time the facility responds, the person has sustained an injury or at worst, has died. However, a simple scenario of reporting a change in the medical condition is complicated. For example, if the person with DD has communication difficulties, or is non-verbal, they will have limited ability to communicate a change or discuss symptoms with their care providers. Their care providers will need to look at overt signs, such as weight gain/loss, intake and output including changes with bowel or bladder, fever, etc. They will also need to look at more subtle signs such as grimacing with pain, lethargy, or change in behavior. The care providers will need to know their client and need skills in understanding and interpreting the signs and signals that the individual with DD uses to communicate their wants and needs. As the majority of people with DD live in the group home setting (ICF/MRs and HCBS Waivers), and most are run by private companies that contract with the State, the LNC will need to determine the applicable State regulatory agency. This will assist with identifying the standards expected from the State agency. The LNC may also need to examine the statutes and regulations including those from Medicaid and/or Medicare. Portions of the basic information on laws, regulations and compliance information are found on the website for the Centers for Medicare and Medicaid Services (www.cms.hhs.gov). 12 Issues in Residential and Community Based Care 13 Each State determines the settings and regulations for supporting people with DD. Because services are often de-centralized, it is important for the LNC to be aware that different agencies are involved in the service delivery system. Most residential homes are privately run receiving service funding from the State. Some State agencies include DD in their name, while others may be linked to Mental Health with one State agency that provides the umbrella for services for people with DD, mental health and substance abuse. The National Association of State Directors of Developmental Disabilities Services (NASDDS) provides a list of the State agencies involved in providing services (www.nasdds.org). Another source for obtaining information is the National Dissemination Center for Children with Disabilities (NICHY) that provides information on various state resources, including agencies (www.nichcy.org). Although the system is implemented differently in each state, every state has a designated department to address the needs of people with DD. President John F, Kennedy in the 1960s established the Office of Mental Retardation which later became the Administration on Developmental Disabilities (ADD). The ADD, a Federal agency, is located within the United States Department of Health and Human Services with four grant programs responsible to work with their respective state governments and communities. Each State has a State Council on DD and an associated agency responsible for DD services and supports. Each state has a Protection and Advocacy (P & A) system, with attorneys available to protect the legal rights of individuals with DD. P & A has been involved with class action litigation especially with de-institutionalization and ensuring community based living options and supports are available and accessible. Each state has a University Center for Excellence in DD (formerly called University 13 Issues in Residential and Community Based Care 14 Affiliated Programs) that provide centers for learning, research, and clinical experience for students in the field of DD. Each state has a Project of National Significance, a discretionary program providing funding for national initiatives and technical assistance. Facility Information On the facility level, it will be important to obtain the policies and procedures of the facilities to determine compliance. Facility policies and procedures provide information not only on what the expectations are for the facility but also for the staff. To work in a facility, the staff generally receives some type of training on the DD population, first aid, medication administration, etc. It is important to remember that the direct care staff working in the residential home is generally not medically trained. They are instructed in basic signs and symptoms and taught to report medical changes to their supervisors and/or designated staff. People with DD may have medications for chronic conditions such as seizures, psychotropic medications for behavioral issues, and medications for gastro esophageal reflux. They are often on multiple medications with many potential side effects and adverse reactions. The staff needs knowledge regarding medication and side effects, how to report changes in condition and who to report to when changes occur. In addition, psychotropic medications cannot be used as a chemical restraint, and each resident must have a plan of care to avoid abuse of these medications and a written plan of treatment. 14 Issues in Residential and Community Based Care 15 Medications may be administered by nursing staff or they may be delegated to the direct care staff. Medication administration by non nursing staff varies greatly from state to state. For example, medication aides in Virginia are required to receive a minimum of 32 hours of classroom instruction and pass a written and practical (skill demonstration) exam. The medication aide will then be able to assist with the self-administration of medication to individuals and is not expected to perform any tasks or procedures involving a medication that requires professional training and education such as that in the field of nursing. The training program is taught by a designated licensed health care provider who received training in the medication aide management course approved by the Board of Nursing (Kirkpatrick, 2000). Interestingly, this medication training program is the same program for staff working in assisted living. In the residential setting each resident has a formal chart, but they are quite different from a hospital chart. The residents live there and their care needs are regular and routine. The chart may contain admission information and initial assessment, history, medications, physician’s orders, resident’s rights, individualized habilitation plan or Individualized Service Plan with annual goals, etc. If the resident has been in the facility for many years, the charts are routinely thinned and only current information may be in the chart. Daily notes are often communicated informally in logbooks written for staff coordination. An incident report is written if an unusual incident has occurred, and an action plan should be noted. 15 Issues in Residential and Community Based Care 16 Nursing Standards The LNC will also need to determine the involvement of nursing. Nursing care in all settings and programs are dictated by the need and health status of the individual with DD. In some settings the resident may receive direct and daily nursing care by a licensed registered nurse or a licensed professional nurse, and in other settings they may receive care on a much more episodic nature. Most HCBS Waiver homes are generally structured with minimal nursing oversight. Each State’s Nurse Practice Act determines the scope and practice of nursing care including what functions are performed by nursing and which tasks can be delegated. In addition, there is the ANA Scope and Standards of Practice for Intellectual and DD Nursing (2004). DD nursing encompasses a lifetime of care for people at different ages with different care needs and in various settings. Developmental Disabilities Nursing Practice (Aggen, et. al., 1995;2008) has also established standards of practice. These standards provide direction for the professional nurse in every setting in which people with DD receive nursing services and supports and a general framework for evaluation. Nurses in the field of DD have had the opportunity to become certified since 1994. Certification requires nursing experience (4000 hours working in the field of DD in the last 5 years), ongoing continuing education specific to DD and a peer-reviewed examination. Role of the LNC The LNC may assist the attorney in various ways. As this is a very specialized field, the LNC will need experience in the field of DD and long term care. The LNC may 16 Issues in Residential and Community Based Care 17 be involved in the role of an educator, and build the attorney’s knowledge base about DD, the diverse population, various diagnoses, and specifically an individual’s care needs. In this role, the LNC will discuss the types of the residential care setting for people with DD and how long term care differs from the acute care hospital setting and the nursing home setting. The LNC may be involved as a consultant to examine the case, evaluate the standard of care, obtain information, such as policies and procedures, and assist with determining if the standard of care has been met. The LNC may need to develop a time line to determine the sequence of events including staff involvement to determine negligence or errors of omission. The LNC may be involved as an expert witness with expertise in the field of DD. In this testifying role, the LNC will educate the judge and jury. The LNC may also be involved in class action lawsuits using the expertise and knowledge in the field of DD. Case Examples Medication Administration When the majority of people with DD lived in the large state institutions, service delivery was based on the medical model, and nursing staff were available and responsible for daily assessment and medication administration. People with DD now live in a variety of settings, and there may or may not be a nurse available to administer medications. In addition, many people with DD have self-care deficits, that may include communication difficulties, oral motor difficulties, hand-eye coordination problems, cognitive difficulties, and deficits in fine and gross motor skills (Barks, 1994). These selfcare deficits contribute to their inability to self-administer medications that is 17 Issues in Residential and Community Based Care 18 compounded because of the need for multiple medications with many adverse effects. The area of medication administration is ripe for errors in all settings, including settings for people with DD. Medications are often administered in bubble packs, where daily medication is inserted in a blister from the pharmacy. Medication needs to be checked using the 6 rights of medication administration (the 6th right being right documentation), and medication needs to be checked with the physician order. The person administering medication needs familiarity with the medication, purpose, dose, side effects, etc. This clinical nurse specialist working in a residential ICF/MR setting once received a call from staff working in a residential facility because the staff had administered medication at the wrong time, and the medication was Theragran M (a multi-vitamin). Obviously this was not an area of concern, except for education, as the staff needed education on what medication was being administered, side effects, etc. Another time, this clinical nurse specialist was called when the morning staff administered the same medication that the night staff had (duplicate dose). This medication error occurred because the night staff had not documented the medication doses, and the morning staff administered medication without noticing it was the wrong date and time. The physician was contacted and the individuals were monitored during the day without any further incidents. The results could have resulted in hospitalization, medical appointments and worse as many individuals were on seizure medication with tight therapeutic dose levels. Wrongful Death 18 Issues in Residential and Community Based Care 19 When an individual with DD condition changes resulting in an early death, the LNC may be contacted to determine if there was negligence at the facility. The LNC will need to determine the standards of care and whether or not standards of care were followed. This situation may be further complicated when an individual with DD has a medical condition and that could contribute to the early demise. The LNC will need to examine standards of care, federal, state and local standards, facility records, level of care needs, in addition to knowledge of the individual with DD. A choking incident is often a common liability issue. Individuals with DD often have self-care deficits including oral motor difficulties. Mobility may also play a factor in feeding and medication administration. For example, an individual with spastic quadriplegia cerebral palsy may have difficulty sitting in an upright position and need proper positioning in order to avoid aspiration. If an individual with DD has an injury and/or death related to a choking incident, the LNC will need to evaluate the case for merit. The LNC that reviews the records needs extensive knowledge about DD, understanding of the medical needs, the aging process including physiological and psychological changes, and the special concerns for individuals with DD. The LNC will need knowledge on the difference between normal processes and bodily insult. While the plaintiff attorney will cite neglect and wrongful death due to breach in the standard of care, the defense attorney will often state that death does not necessary mean impropriety and can occur from natural causes, especially as people with DD are classified as a vulnerable population with a reduced life expectancy from the typical population. The following example provided is a clear violation of the standard of care resulting in an untimely and early death (wrongful death) of a young individual. The 19 Issues in Residential and Community Based Care 20 plaintiff, who had cerebral palsy and intellectual disabilities, lived in an ICF/MR in Texas from June 1, 1992 to her death on April 16th, 1998.. When the plaintiff fell in a hallway and defecated on the floor on 4/12/1998, the aide poured a mixture of undiluted bleach and another cleaning compound on the floor, left the plaintiff on the floor for at least an hour, and did not wash the bleach off the plaintiff. The plaintiff was not seen by the facility’s doctor until 17 hours after the incident. She later was diagnosed with extensive chemical burns covering 40% of her body and died from these complications on 4/15/1998. A wrongful death and survival suit for compensatory and punitive damages was filed by her family, later amending it to include ongoing neglect and abuse (Wright v. Res-care, 2002). Abuse and Neglect Individuals with DD are considered a vulnerable population and are at risk for abuse and neglect at all ages. Women with DD are considered at high risk for sexual abuse as they often may be unwilling victims, or at the other extreme, be overly friendly without knowing the effect on others. Training programs and sexuality awareness is taught, but this population is vulnerable to abuse and neglect. The following is a recent example of an assault case. In determining these cases, the issue is often whether the residential home had knowledge of a staff’s violent history, or should have known, and if the residential home exercised ordinary care to protect its residents from the assault. The plaintiff, described in court documents as a severely handicapped person, nonverbal, wheelchair dependent, and legally blind, lived in a residential facility for the 20 Issues in Residential and Community Based Care 21 DD in Rhode Island. She suffered a severe bruise that extended from the vagina to the rectum. She was examined at the hospital, and police were notified, however, there were no criminal charges filed. A civil action was filed alleging intentional and negligent conduct on the staff. The judge found that plaintiffs failed to produce any evidence of assault and there was no negligence as the plaintiffs failed to offer any evidence or expert testimony that the injury was caused by a breach of the standard of care. The plaintiffs appealed and the ruling was affirmed in the Rhode Island Supreme Court (Broadley v. Rhode Island, 2008 ).. In another example, the direct care staff was involved in a criminal charge of elderly and dependent adult abuse. This plaintiff, a 51-year-old individual with DD with limited verbal skills and wheelchair dependent, resided in a residential facility for the DD in California. On May 4, 2004, she was seated in the shower and the water heater broke, causing a scalding and third degree burns over 60 % of her body. The aide did not report this to her supervisor for 2 hours. The plaintiff was airlifted to Santa Clara Hospital and is currently nonverbal and gastrostomy tube dependent reporting a $3,000 per day care in a subacute setting. The aide was arrested for elderly and dependent adult abuse, later pled guilty, served jail time and probation and was banned from working in other healthcare facilities. The case was eventually settled. (Rodriguez v. Res-Care , 2004), Other Case Examples In this case, the staff clearly did not follow the standard of care and were negligent, and their negligence caused injuries to the resident. 21 Issues in Residential and Community Based Care 22 The plaintiff, a 33-year-old-woman with DD, resided in an assistive living facility, called a personal care home, in Pennsylvania. Her mother was contacted and was notified that her daughter was either sick or pretending to be sick. The mother found her daughter screaming and crying with a soiled diaper and diarrhea. The mother cleaned her daughter without staff assistance, and informed the staff her daughter was sick. No one at the Ivy Ridge facility responded. The mother took her daughter to the hospital where she was admitted for viral gastroenteritis, fecal impaction and dehydration. She was discharged three days later. The court, upheld a jury verdict, and found the Ivy Ridge breached its duty of care by neglecting the plaintiff ( Ruta v. Ivy Ridge Personal Care Center, 1995), In a recent case, an individual with DD was scalded during bathing. Interestingly, it was alleged by the defense that the resident had turned on the water of the bath causing his own injury. The 42-year-old plaintiff was described as having severe mental disabilities, was non-ambulatory, non-verbal with cerebral palsy, and resided in a residential facility for the DD in Indiana. He sustained first and second-degree burns to his lower body when placed in a bath of scalding hot water in 2000.. The estate of the plaintiff was awarded $1.5 million in damages on January 2008 to provide for his ongoing care needs. This was considered one of the largest jury verdicts in Madison County’s history (McGrath, 2008)), Chapter Summary People with DD are a diverse group of people with different ages and abilities and they may reside in various residential settings in the community. The LNC in this field 22 Issues in Residential and Community Based Care 23 needs a solid clinical foundation in DD and health care issues in addition to an understanding of the residential setting options, and standards and regulations on the federal, state and local level. This will continue to be a growing field as the population ages, and will provide both opportunities and challenges for the LNC involved in residential care. References Administration on Developmental Disabilities (2008). ADD Fact Sheet. Retrieved on 7/27/08, from http;//www.acf.hhs.gov/programs/add/Factsheet.html Aggen, R.L., Broda, T., Brown, K, Kurlick, M, Lester, N. & Tupper, L. (2008). Standards of Developmental Disabilities Nurses Practice. Eugene, OR: Developmental Disabilities Nurses Association. Aggen, R.L., DeGennaro, M.D., Fox, L., Hahn, J.E., Logan, B.A. & VonFumetti, L. (1995). Standards of Developmental Disabilities Nurses Practice. Eugene, OR: Developmental Disabilities Nurses Association. American Nurses Association (2004). Intellectual and Developmental Disabilities Nursing: Scope and Standards of Practice. Silver Spring, MD; nursebooks.org American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC, American Psychiatric Association. Bannerman, D. J., Sheldon, J. B., Sherman, J. A. & Harchik. A. E. (1990). Balancing the right to habilitation with the right to personal liberties: The rights of people with developmental disabilities to eat too many doughnuts and take a nap. Journal of Applied Behavior Analysis 23, 79-80. Barks, L. (1994). Approaches to medication administration. In Roth & Morse (Ed.) A Life-Span Approach to Nursing Care. (pp. 193-218). Baltimore. Paul H. Brookes. Braddock, D., Hemp, R., & Rizzolo, M.C. (2008). The State of the States in Developmental Disabilities 2008. Washington D.C. Broadley v. State of Rhode Island et, al . 2007-80-Appeal. (PC 97-387). 2008. 23 Issues in Residential and Community Based Care 24 California Lanterman Developmental Disabilities Services Act, (1976). Welfare and Institutions Code, Section 4512 (a). Department of Health & Human Services (2008). Intermediate care facilities for the mentally retarded (ICFs/MR). Retrieved on 7/28/08, from http;//www.cms/hhs.gov/CertificationandComplianc/09_ICFMRs.asp Developmental Disabilities Assistance and Bill of Right Act Amendments (2000). P.L. 106-402 (42 U.S.C. 15002 Sec.102). Kirkpatrick, M. A. (2000). A resource guide for medication management for persons authorized under the drug control act. Virginia Department of Social Services. Commonwealth of Virginia. Lakin, K.,C, Prouty, R., Alba, K, & Scott, N.. (2008). Twenty-five years of Medicaid home and community based services (HCBS): Significant milestones reached in 2007. Intellectual and Developmental Disabilities (46) 4. 325-328. McGrath, S. (2008, January 28). Update: Jury award $1.5 million to man who was scalded. The Herald Bulletin. Retrieved on 3/10/09 from http://www.hearaldbulletin.com/local/local_story_02811829html/resources_prints tory Nehring, W.M. (2003). History of the role of nurses caring for persons with mental retardation. The Nursing Clinics of North America, 38 (2), 351-372. Olmstead v L.C. (98-536), 527 U.S. 581 (1999). Palley, H.A., & Van Hollen, V. (2000). Long-term care for people with developmental disabilities: A critical analysis. Health and Social Work, 25 (3), 181-189. Parish, S. L., & Lutwick, Z. E. (2005). A critical analysis of the emerging crisis in longterm care for people with developmental disabilities. Social Work, 50 (4), 345354. Pouty, R. W., Smith, G. & Larkin, K. C. (2007). Residential services for persons with developmental disabilities: Status and trends through 2006. Minneapolis: University of Minnesota, Research and Training Center on Community Living, Institute on Community Integration. Rodriguez. v. Res-Care. San Mateo County Superior Court Case No. 114740. B (2004). Ruta v. Ivy Ridge Personal Care Center, Inc. 29 Philadelphia 185. (1995). Service, K.P. & Hahn, J.E. (2003). Issues in aging: The role of the nurse in the care of older people with intellectual and developmental disabilities. The Nursing Clinics 24 Issues in Residential and Community Based Care 25 of North America, 38 (2), 91-312. Smith, G. A. (2006). Status report: Litigation concerning home and community services for people with disabilities. Human Services Research Institute. Retrieved 8/27/08, from http:www.hrsi.org/doc/litigations052906 Wright v. Res-Care, U.S. Dist. LEXIS 4507 (5th Cir. June 2, 2002). Resources Issues in Residential and Community Based Care- Developmental Disabilities Administration on Developmental Disabilities (ADD) The Federal agency that is responsible for the implementation and administration of the Developmental Disabilities Assistance and Bill of Rights Act. ADD is located within the United States Department of Health and Human Services and is part of the Department’s Administration for Children and Families. http://www.acf.hhs.gov American Association on Intellectual and Developmental Disabilities (AAIDD) Formerly called the American Association on Mental Retardation, AAIDD is the oldest and largest interdisciplinary organization of professionals involved in the field of intellectual and developmental disabilities. http://www.aaidd.org American Health Care Association (AHCA) AHCA is a non-profit association of state health organizations and represent nonprofit and for profit assisted living, nursing facility, developmentally disabled and sub acute care providers. They focus on providing quality care to elderly and individuals with developmental disabilities in long term care facilities and the services include information, education, legislative, regulatory and public affairs. They also provide information on trends and government financing of long term care. http://www.ahcancal.org ARC The Arc (formerly the Associated for Retarded Citizens) is the largest community based organization for people with intellectual and developmental disabilities. It provides services and support for families and individuals through local and state chapters. http://www.thearc.org 25 Issues in Residential and Community Based Care 26 Centers for Medicare and Medicaid Services (CMS) The United States Department of Health and Human Services administers the Medicare, Medicaid and State Children’s Health Insurance Program. There is extensive information available for lay and health care professionals including laws, regulations, and compliance information. CMS establishes the standards for the operations of facilities that receive funds under the Medicare or Medicaid Program. Information on Home and Community Based programs and ICF/MRs are also available. http:www.cms.hhs/gov Developmental Disabilities Nurses Association (DDNA) DDNA is a national organization for nurses specializing in the field of developmental disabilities. The organization provides education, networking, certification and advocacy and has developed standards for developmental disabilities nursing practice. They offer certification in the field of nursing and developmental disabilities, annual conferences and have local State chapters. http://www.ddna.org/ Easter Seals Easter Seals is a community-based health agency for children and adults with disabilities for over 90 years. They have offices provided services and supports in most States. Easter Seals’ recently was involved in the Living with Autism Study conducted in 2008. www.easterseals.com National Association of State Directors of Developmental Disabilities Services (NASDDDS) A nonprofit organization established in 1964 in order to improve and expand the public services available to individuals with intellectual and other developmental disabilities. They assist State agencies in developing effective service delivery systems. They provide listings of the developmental disabilities State agency and contact information. http://www.nasddds.org National Dissemination Center for Children with Disabilities NICHY is the center that provides information on programs and services for infants, children and youth with disabilities, including information on special education laws, agencies, resources and research. http://wwww.nichcy.org Protection and Advocacy (P & A) P & A agencies are congressionally mandated, legally based disability rights agencies available at the national and state level. They provide legal representation and other advocacy services to all people with disabilities whether they reside at home or in residential facilities. P & A monitors, investigates and attempts to remedy any adverse conditions. http://www.napas.org 26 Issues in Residential and Community Based Care 27 University Centers for Excellent in Developmental Disabilities Education, Research and Service Formerly known as the University Affiliated Programs, these centers were established in 1963 and are located in universities in every state. The University Centers offer an interdisciplinary training team in advanced practice specializing in clinical excellence services, research, and programs in the field of developmental disabilities and help prepare the future generation to be involved in the field of developmental disabilities. http://www.aucd.org United Cerebral Palsy (UCP) Founded in 1949, this national organization mission is to advance the independence, productivity and full citizenship of people with disabilities. State UCP services may include housing, therapy, assistive technology training, early intervention programs, individual and family support, social and recreation programs, community living, state and local referrals, employment assistance and advocacy. http://www.ucp.org Test Questions Issues in Residential and Community Based Care-Developmental Disabilities 1. The LNC in the role of the educator can assist the attorney by: a. Reviewing the Nurse Practice Act b. Obtaining information on policy and procedures c. Detailing the differences between nursing home and community care regulations d. Becoming an expert witness Answer C 2. Trends and growth in long term care for people with developmental disabilities include: a. Home and Community Based Service Waiver Homes b. Intermediate Care Facilities for the Mentally Retarded c. De-population of the State Developmental Centers d. All of the above Answer A 3. The LNC in this field needs knowledge on the various legislative regulations for long term care. A good source is found at: a. Developmental Disabilities Assistance Act and Bill of Rights b. Centers for Medicare and Medicaid Services c. Developmental Disabilities Nurses Association 27 Issues in Residential and Community Based Care 28 d. Easter Seals Answer B 28 Issues in Residential and Community Based Care 29 ASSISTED LIVING Contents Objectives Introduction Overview of the Assisted Living Legal/Ethical Issues Litigation LNC Role in Trial Preparation or as an Expert Witness Chapter Summary References Resources Test Questions Objectives 1. To describe an overview of Assisted Living, including the Assisted Living Facility (ALF) philosophy, services available, and the clients it serves. 2. To list the varied legal and regulatory requirements related to Assisted Living Facilities. 3. To define the LNC role in assisting with an Assisted Living case, or in acting as an expert witness. Introduction The Assisted Living portion of this chapter will focus on residential and community based care issues for individuals who reside in Assisted Living Facilities (ALF). Although Assisted Living residents are generally from the elderly segment of the population, individuals with developmental disabilities also reside successfully in assisted 29 Issues in Residential and Community Based Care 30 living residences. The rationale for separating Assisted Living from the Nursing Home/Long Term Care chapter is that there is a significant difference in the federal and state regulations and the nursing scope of practice for Assisted Living. The LNC must understand this difference when assisting the attorney in cases involving Assisted Living residents. Overview of Assisted Living Historical Perspective Assisted Living is a senior housing concept originally developed in Scandinavia during the 1970s, combining residential housing for the elderly, with personal care services. Assisted Living first emerged in the United States during the mid-1980s. (Thayer, 2003). Initially, there were residential care facilities commonly known as board and care facilities. Board and care facilities provided non-medical care and supervision, and were sometimes located in the private homes of the service providers. (Pratt, 2004). Board and care providers admitted residents who required minimal assistance with Activities of Daily Living (ADLs) and required no nursing services. As the resident's physical condition deteriorated, it would necessitate a transfer to a skilled nursing facility or nursing home resulting in decreased occupancy. To address the decrease in occupancy, many board and care providers began accepting and retaining residents requiring more assistance with ADLs and more than occasional nursing services. (Murer, 1997). Assisted Living ultimately evolved into a long-term care alternative for seniors requiring more assistance than is available in a retirement community, but do not need the intense medical and nursing care provided in a skilled nursing facility. The primary 30 Issues in Residential and Community Based Care 31 goal of Assisted Living then and now is to provide a setting in which individuals obtain those services needed to allow them to live with as much independence and dignity as possible. (Pratt, 2004) Assisted Living environments range from shared one-room accommodations to apartments complete with kitchens and living rooms. For most providers, Assisted Living means providing housekeeping services, meals, laundry, transportation, and limited licensed nursing services and/or oversight, including the administration of medication. (Murer, 1997) Residences may be free standing or housed with other residential options, such as independent living or skilled nursing care. They may be operated by non-profit or for-profit companies. Most facilities have between 25 and 120 units. There is no single blueprint, because consumers' preferences and needs vary widely. (ALFA, 2008) Definition of Assisted Living The National Center for Assisted Living (NCAL) reports that Assisted Living settings have been known by as many as 26 different names, including residential care, personal care, adult congregate care, boarding home, and domiciliary care. (Pratt, 2004) Even government and industry leaders can’t agree on a precise definition. The Centers for Medicare and Medicaid Services (CMS) define Assisted Living as “a type of living arrangement in which personal care services, such as meals, housekeeping, transportation, and assistance with activities of daily living (ADLs), are available as needed to individuals who still live on their own in a residential facility.” In most cases the residents of these facilities pay regular monthly rent, with additional fees for other supportive services. (GAO, 2004) 31 Issues in Residential and Community Based Care 32 The Assisted Living Federation of America’s (ALFA) definition of an Assisted Living residence is “a special combination of housing, personalized assistance and health care designed to respond to the individual needs - both scheduled and unscheduled - of those who require help with ADLs and the instrumental activities of daily living (IADLs). IADLs include using the telephone, getting to locations beyond walking distance, grocery shopping, preparing meals, doing laundry, taking medications and managing money.” (GAO, 2004) Philosophy of Care Assisted Living’s philosophy of care as described by AARP (American Association of Retired Persons) – Assisted Living is the maximization of resident’s personal dignity, autonomy, independence, privacy, and choice; provision of homelike environment; accommodation of resident’s changing care needs and preferences; minimization of the need to move when care needs increase; with the involvement of families and communities. (AARP, 2008). The LNC should understand that unlike other medical models found in most health care settings, assisted living is based on a social model of care, with a holistic approach. Demographics and Scope of Services There are approximately 36,000 state-licensed Assisted Living Facilities housing approximately 900,000 older Americans and individuals with disabilities. (GAO, 2004). The typical assisted living resident is a female, 75-85 years old, who is mobile, but needs assistance with two to three activities of daily living. Of the residents who currently live in Assisted Living Facilities, 81% need help with one or more ADLs, and 93% need help with IADLs. (Podrazik & Stefanacci, 2005). In the 2004 GAO Report, 25% of Assisted 32 Issues in Residential and Community Based Care 33 Living residents required assistance with three or more ADLs and 86% of residents required or accepted assistance with medication. Nearly half of all assisted living residents lived at home prior to moving to the facility, while nearly one third came from another Assisted Living Facility, nursing facility, or a hospital. (GAO, 2004) The average length of stay in an Assisted Living residence is about 27 months. Upon discharge from Assisted Living, 34% of the residents will move into a nursing facility, 30% will have expired, and the remaining will move home or to another location. (NCAL, 2008) While the vast majority of residents are elderly persons with some level of health care needs, Assisted Living is also becoming the environment of choice for those with Alzheimer's or other dementias, with many Assisted Living residences having dedicated Memory Care or Alzheimer's units. Recent studies conducted by the Alzheimer’s Association concluded that at least half of Assisted Living residents have some degree of cognitive impairment, though most of them do not live in specialized dementia units. (Alzheimer’s Association, 2008). Residents in need of end-of life care prefer to have the hospice benefit provided in their Assisted Living residence, although not every state allows hospice residents this right. Finally, it is conceivable that, within the near future, special care for Assisted Living residents will go beyond dementia care to encompass intravenous medication therapies, respiratory therapies and rehabilitation. Legal and Ethical Issues Regulations and Licensure 33 Issues in Residential and Community Based Care 34 The LNC must consider all related federal, state and local regulations related to Assisted Living when conducting a legal review of an Assisted Living case. Skilled nursing facilities have been heavily regulated for decades; it is only in the past few years that Assisted Living Facilities have been regulated to any significant degree. As the Assisted Living focus moves from housing to medical services, it will eventually be viewed and regulated as a health care provider. (Murer, 1997) In most states, Assisted Living is licensed as a “single entity that provides housing and services to residents”. However, in a growing number of states a model of Assisted Living has emerged in which the housing and services are separate. In this model, the building is not licensed, but instead makes arrangements with “licensed service agencies” to provide services to the residents. The “licensed service agency”, also known as a Home Health Care agency is regulated under state and federal law. In the unlicensed housing arrangement, the building is subject to the relevant building codes, fire codes, and other requirements for multiunit housing. The state may also require the building to be registered. Registration involves a much lower level of oversight than licensure and may require only that the building file a registration form, for example, and provide a disclosure statement to residents. (Wright, 2007) An Assisted Living Facility must also comply with the same regulations related to the Fair Housing Act, Occupational Safety and Health Act (OSHA), Life Safety Code, requirements of the Equal Employment Opportunity Commission (EEOC), and the Family Medical Leave Act (FMLA).(Pratt, 2004) The LNC when reviewing a case related to Assisted Living should reference the Federal Acts listed, and also carefully 34 Issues in Residential and Community Based Care 35 evaluate state laws and regulations affecting licensing, resident rights and housing, as applicable. As noted, there are federal laws that impact Assisted Living, but oversight of Assisted Living occurs primarily at the state level. While states vary in their approach to regulating Assisted Living, most have comprehensive regulations in place. In those states, surveyors conduct regularly scheduled inspections. To ensure that Assisted Living Facilities correct the deficiencies cited during the survey, states may require the facility to prepare a formal written plan of correction. In addition, these states may conduct reinspections and impose financial penalties, license revocations, and criminal sanctions. (GAO, 2004) The LNC will benefit from an understanding of the state-specific Assisted Living regulations and definitions when reviewing an Assisted Living case. Research of these regulations can be exhaustive as there is no one central agency or section of state law that encompasses all aspects for all states. The NCAL Assisted Living State Regulatory Review is a resource that is updated annually and is based on the applicable statutes and regulations in each state. It can be a valuable resource for the LNC in researching state specific information related to 21 state specific categories. Staff Requirements/Qualifications/Training Staffing levels are much less controlled by regulation in Assisted Living than in other levels of long term care. Whereas one Assisted Living community may offer care specialized for individuals with dementia, another community may focus on providing services for residents with lower acuity needs. Each facility must have the right number 35 Issues in Residential and Community Based Care 36 of trained and awake staff on duty and present at all times to meet residents’ needs and to carry out the facility’s emergency and disaster preparedness plan. (ALW, 2003) All states require skilled nursing facility administrators to be licensed, but not so with Assisted Living administrators. An increasing number of jurisdictions are requiring their licensure, but there is little uniformity in those requirements. In most states that do license Assisted Living administrators, the requirements are significantly less rigorous than for skilled nursing facility administrators. (Pratt, 2004) Assisted Living Facilities must ensure that personnel working in their facility perform duties only within the scope of that State’s Nurse Practice Act, or other professional licensing or practice requirements. The professional scope and standards of practice as established by the American Nurses Association (ANA), National Gerontological Nursing Association (NGNA), and the American Assisted Living Nurse’s Association (AALNA) should be adhered to in all aspects of Assisted Living nursing functions. In general, staff should be knowledgeable regarding basic changes in aging, geriatric drug pharmacology, falls prevention, incontinence care, ADL skills, communication techniques, dementia care, and recognition of acute illness/delirium. Assisted Living Facilities have a duty to retain staff that is capable of monitoring a resident’s well-being and determining when significant medical, cognitive, and functional changes have occurred and evaluation by a qualified medical professional is necessary. (Podrazik & Stefanacci, 2005) Staff should receive proper orientation and training and performance evaluation to be conducted no less than annually. There is a call for a federal system for criminal background checks and state requirements regarding convictions that would disqualify individuals from providing 36 Issues in Residential and Community Based Care 37 services in Assisted Living Facilities, and recommends the establishment of a national registry of individuals with histories of abuse. (ALW, 2003) Medication Management An important concern in the administration of Assisted Living Facilities is how resident’s medications are managed and administered. Research has shown that Assisted Living residents take an average of 8 medications per day. (ALFA, 2008) Assisted Living regulations span the gamut from requiring all residents to be capable of selfadministration to allowing unlicensed staff to administer some medications under a licensed staff member's supervision. Many states allow staff to assist residents with their medication. "Assistance" being interpreted to include verbal reminders, opening the medication container, placing the medication in the patient's hand and even guiding the resident's hand to his/her mouth. (Murer, 1997) When reviewing an Assisted Living case, the LNC should be familiar with Assisted Living state requirements and the State’s Nurse Practice Act scope of practice guidelines concerning medication administration. Knowledge of state pharmacy laws is also very important. Such issues as drug storage regulations and dispensing requirements could alter the nature of the program. Packaging policies also vary from state to state. (Donovan, 1997) The facility should provide ongoing training of medication assistants on a regular basis to ensure competence. Medication administration policies and procedures are vital to medication administration safety and consistency. (Podrazik & Stefanacci, 2005). One area that has received attention has been training for medication aides. More states are allowing unlicensed staff, providing they are adequately trained, to assist in the administration of medications. 37 Issues in Residential and Community Based Care 38 Licensed nurses are the gate-keepers for the medication program. The nurses' overall responsibility for administration of medication as a licensed professional remains the same as for any setting: receiving medication orders, checking for allergies, ordering medications from the pharmacy, validating correctness of labels, assessing effectiveness, documenting and reporting adverse reactions, and policing the quality assurance component of administration - in short, ensuring that the right medication is given at the right time to the right individual. (Donovan) Determining appropriateness of self-administration of medications by an Assisted Living resident is a nursing process which requires a "judgment call" based on the nurse's education and experience in caring for the geriatric population. The nurse must ensure before a resident can participate in self administration of medications, that he/she first demonstrates competency (mental and physical) in self-administration of medications, and the ability to remain compliant with prescribed drug regimens. This is accomplished through a standardized assessment conducted by the licensed nurse focusing on such abilities as dexterity, comprehension, recall and visual acuity. The assessment is applicable to oral medications, inhalers/nebulizers, dermal patches, topical ointments, and occasionally injections. The medication self-administration assessment should be conducted upon admission, and at a minimum annually or with change in condition and results documented on a standardized form which is maintained in the medical record. More complicated routes of administration, such as suppositories and injections, are generally the responsibility of the nurse unless the resident has demonstrated capability for these. Some residents may have self-administered insulin for many years, but it must be determined that they still have the dexterity to draw up the insulin and 38 Issues in Residential and Community Based Care 39 adequate vision to read the units. For the resident who does not successfully pass the assessment, medications are delivered in the traditional manner and a reassessment is rescheduled. Resident Rights Many states already address to varying degrees, the rights of Assisted Living Facility residents, in ways that are often similar to, if not the same as, rights afforded nursing home residents. Residents of Assisted Living do not check their rights at the door upon moving into an Assisted Living community. To assume that an individual cannot continue to have the same rights to privacy, independence and decision making no matter where they live, is discriminatory. Participation of a guardian or responsible party is facilitated to ensure that the rights of cognitively impaired residents are preserved. The National Center for Assisted Living (NCAL) advocates that residents’ rights should include the right to: ▪ Privacy ▪ Be treated at all times with dignity and respect ▪ Control receipt of health care services ▪ Control personal finances ▪ Retain and have use of personal possessions ▪ Interact freely with others both within the assisted living residence and in the community ▪ Freedom of religion ▪ Organize resident councils Consumer Disclosure 39 Issues in Residential and Community Based Care 40 Consumer disclosure is essential in assisting consumers with understanding the differences among Assisted Living communities and to select the one that best meets the needs of their loved one. The decision to reside in an Assisted Living Facility should be an informed choice with providers fully disclosing their programs, services and fees, so that the resident and family can make an informed choice about where to live. There should be a decision- making process that involves the provider, resident/resident’s family and physician to make the decision. This decision includes end of life planning. Providing consumers with the information and tools they need to make the best choice possible about where to live is also a recent legislative trend. Residency/admission agreements have improved through legislation addressing information that should be included in these agreements. In addition to the admission/residency agreement, many states now require Assisted Living providers to disseminate disclosure documents to prospective residents and families that include information about facility services, costs, policies that impact residents, limitations on care delivery, and the move in and move out processes. (ALFA, 2008) Consumers need this information to not only be complete and accurate, but also presented in a timely way and in a form that they can understand. Consumers rely on facility information that they receive in various ways, including marketing brochures, facility tours, and interviews with providers. Often marketing materials, contracts and other written materials that facilities give consumers is vague, incomplete or misleading. Facility’s written materials often do not contain key information, such as a description of services that are not covered or available at the facility, the staff’s qualifications and 40 Issues in Residential and Community Based Care 41 training, circumstances under which costs might change, assistance residents would receive with medication administration, facility practices in assessing needs, or criteria for discharging residents if their health changes.(GAO, 2004) Residency/Admission Agreement Clearly defined contractual obligations to residents in the written residency/admission agreement are an important first step in preventing or limiting liability in Assisted Living. Residency/admission agreements can be highly state-specific, especially in states that license or otherwise regulate ALFs. In part, the residency/admission agreement is a housing rental contract. Thus, it must comply with federal, state, and local housing and landlord/tenant laws. The housing portion of the agreement covers the type of accommodation, the fee schedule, payment terms, deposits, the period the agreement is in effect, etc. Review of the residency/admission agreement by the LNC is essential in preparation for an Assisted Living case. The second part of the residency/admission agreement pertains to the health-related or other personal supportive services provided. Minimum state licensure requirements must be included, as applicable. Resident rights and responsibilities should also be listed. The facility is legally obligated to deliver the services promised in the residency/admission agreement. (HRC, 1997) Assisted living facilities should provide specific, comprehensive, straightforward information in the residency/admission agreement. The residency/admission agreement should be consistent with oral and written communications made to residents and family members as part of the facility’s marketing program. Residents should have the opportunity for pre-admission review of 41 Issues in Residential and Community Based Care 42 the residency/admission agreement’s terms. The residency/admission agreement should include: ▪ The term of the agreement/contract; ▪ Comprehensive description of services provided for a basis fee; ▪ Comprehensive description of and the fee schedule for services provide on an alacarte basis; ▪ Temporary absence policy; ▪ Process for initial and subsequent assessments and the development of individualized service plans based on these assessments; ▪ Description of all circumstances and conditions under which the Assisted Living Facility may require the resident to be involuntarily transferred, discharged, or evicted; ▪ An explanation of the resident’s right to notice; and the process by which the resident may appeal the decision, and a description of relocation assistance offered by the facility; ▪ A description of the Assisted Living Facility’s process for resolving complaints or disputes; ▪ A list of appropriate consumer/regulatory agencies; ▪ A description of the procedures a resident must follow to terminate the agreement; ▪ Detailed pre-admission disclosures regarding advance directives, specialized programs of care, and end-of-life care. ▪ Requirements related to resident finances (Thayer, 2003) 42 Issues in Residential and Community Based Care 43 ▪ Verbiage to avoid claims of discrimination including range of services offered, facility rules, and extent to which accommodation is available (HRC, 1997) Resident Assessments/Individualized Service Planning For the aging adult, a move to an Assisted Living Facility often signals some medical, cognitive, or functional need which makes a comprehensive assessment crucial. It offers the opportunity to provide optimum interventions designed to maintain independence and prevent existing conditions from deteriorating. All residents entering an Assisted Living Facility should have a baseline evaluation of their physical, medical, and psychological needs completed by a qualified, licensed, independent practitioner. Residents should receive periodic reassessment to determine if care needs have changed. . (Podrazik & Stefanacci. 2005) The foundation of resident centered care is the Individualized Service Plan (ISP), which can also be known as a care plan, service plan or resident goal plan. The ISP is designed to meet the individual needs and preference of each resident. The ISP is developed after an assessment process that takes into account not only what services the resident needs, but what they want as well. The ISP is completed by a licensed nurse, and is prepared in conjunction with the resident, family and staff. (ALFA, 2008) Negotiated Risk Agreements 43 Issues in Residential and Community Based Care 44 The concept of negotiated risk has been suggested as a mechanism for Assisted Living programs to balance resident’s personal autonomy with the provider’s duty to protect residents from harm. Examples in which negotiated risk has been suggested involve situations such as a resident in an ALF repeatedly departing from a medically prescribed diet or failing to take ordered medications. Negotiated risk in Assisted Living has been compared to the legal and ethical doctrine of informed consent. In Assisted Living, however, the prerogative to refuse unwanted interventions applies not to discrete medical procedures, but to ongoing health related, dietary, and residential interventions that compromise an Assisted Living arrangement. Although the theory has not been tested directly in court, proponents of negotiated risk would be available as a defense to a negligent action if a defendant were able to prove that a plaintiff voluntarily and knowingly assumed the risk of certain conduct that might otherwise be deemed negligent. Or, even if the provider was found negligent, liability might be reduced to the degree of the plaintiff’s own contributory negligence. The assumption of risk, however, is predicated upon the resident or a legally authorized surrogate being capable of a deliberate and voluntary choice. Negotiated risk is a new approach to managing resident related risk. It will not provide full protection from provider liability and may be inappropriate if the risk of harm is very high. As one attorney put it, “residents may assume risk in theory, but hold the facility responsible in practice”. Negotiated risk, properly understood and applied, can fill some of the void in providing an analytic tool and mechanism by which providers and residents can assess and accommodate certain unusual situations. 44 Issues in Residential and Community Based Care 45 Negotiated risk, while a useful tool, should play a relatively limited role in day-today operation of the ALF. Providers always have responsibility to their residents – imposed by regulation, licensure and community expectations – which they cannot avoid or “negotiate away”. Likewise, even though the philosophy of assisted living is to promote resident autonomy and choice, resident rights are not unlimited. (Bianculli, 1999) Litigation As with skilled nursing facilities, assisted living residences have the potential for many of the same legal actions related to negligence and medical malpractice. Many of the traditional health and safety risk areas for long-term care related to medication errors, accident or fall injuries, elopement, smoking, and suicide are also evident in assisted living. Also equipment related causes (e.g. wheelchairs tipping, legs collapsing on commodes, safety belts loosening, and unsafe electric wheelchair use) are another risk area. Negotiated risk factors into this area, as many of the assisted living residents want to manage their own actions in spite of the risk involved. Abuse, neglect, and misappropriation of resident funds are another area that has been cited in recent assisted living cases. Additionally, an assisted living facility would also be subject to any aspect of the Fair Housing Act, Occupational Safety and Health Act (OSHA), Life Safety Code, and Americans with Disabilities Act. LNC Role in Trial Preparation or as an Expert Witness 45 Issues in Residential and Community Based Care 46 The LNC participating in an Assisted Living case has many areas of research and review that should be considered. These efforts should include a review of the Assisted Living Facility’s operational processes and policies related to services, environment, consumer protections (including resident rights, contracts, and risk negotiation), and management responsibilities. Services. Resident screening should have occurred before move-in. In addition, each resident should have undergone a comprehensive assessment for health, psychosocial, and cognitive status. This would have ensured that the facility was able to meet the resident's needs and served as a basis for the development of an individualized service plan (ISP). Information from the resident's physician and documents such as guardianship papers, powers of attorney, living wills, and do-not-resuscitate orders also should have been obtained at the time of admission. The individualized service plan should have been developed with the assistance of the resident and/or designated agent. The individualized service plan should have included the scope, frequency, and duration of services and monitoring, and it should have been responsive to the resident's needs and preferences. The individualized service plan should have been reviewed at routine intervals after move-in and annually thereafter, or as the resident's needs or preferences change. Environment. A safe, homelike environment should have been provided for all residents. This environment should support choice, independence, privacy, comfort, and individuality. Life Safety Code review reports conducted by state, county or local authorities should be obtained and reviewed for violation of safety requirements by the LNC. 46 Issues in Residential and Community Based Care 47 Consumer Protections. Residents' records should have been kept confidential and released only with consent. In addition, providers should have ensured residents' choices and the right to autonomy for as long as possible, even if that meant taking some risks. Residents should have shared responsibility for decisions affecting their lives and have been fully informed of their rights and responsibilities. A copy of the Resident Right statement provided to the resident should be obtained and reviewed by the LNC. Contracts and Agreements. The most significant document in the resident’s stay at the Assisted Living Facility is the residency/admission agreement. The LNC and the attorney must review the document signed by the resident assuring that it encompasses all of the facility's commitments and actual practices, including the criteria and procedures for admission, on-site transfers, and discharge. Payment information should be comprehensive and include: rate structure and payment provisions for both covered and noncovered services; an explanation of billing, payment, and credit policies; criteria for determining level of service and additional charges; fees and payment arrangements for third-party providers; provisions for payment during absences; and the facility's policy for residents who can no longer pay for services. The admission/residency agreement is used by the LNC in citing what should have been provided to the resident by the facility when writing reports or testifying. Negotiated Risk. When a resident wanted to engage in potentially risky behavior, such as service refusal, a negotiated risk agreement should have been initiated, following open discussions with management and family members about the consequences of the resident's choice. If the resident's mental or physical condition changed substantially, the 47 Issues in Residential and Community Based Care 48 negotiated risk agreement should have been reviewed. The LNC should obtain copies of the operational policies, procedures and forms related to Negotiated Risk. Staffing. The facility should have maintained sufficient qualified staff members capable of meeting scheduled and unscheduled resident needs at all times. The LNC should obtain copies of the facility staffing patterns for the time period applicable to the case. The facility should have ongoing training for staff on how to monitor changes in residents' physical, cognitive, and psychosocial conditions. In facilities serving residents with dementia, direct-care staff should receive dementia-specific training each year. The LNC should also review the Assisted Living Facility’s orientation and training outlines and attendance documentation, job descriptions, organizational chart, determination of position and skill knowledge, hiring practices, including background and reference checking processes. Advertising. Facilities must be vigilant about advertising specific features if they cannot ensure 100% service or compliance. Quality-of-care claims or "overselling the product" can leave a facility vulnerable to a lawsuit if they cannot be evidenced through documentation. Examples of such claims include: "Meadow Acres Assisted Living provides the best care possible care," "24-hour assistance provided," "around-the-clock support designed to meet the individual personal care needs of residents," "24-hour supervision," "Meadow Acres supports aging in place; no need to ever move again." Advertising or brochures contain verbal statements that promise residents and families services that cannot be delivered. For example, "Our security system will keep your mom from eloping." If the facility does not provide a locked unit, this claim is untrue. (Peterson, 2005). The LNC should obtain copies of all marketing materials for the time 48 Issues in Residential and Community Based Care 49 period of the case, including copies of informational recordings that would be listened to while an applicant was waiting on the telephone for assistance. Statements of deficiencies from past state health department surveys can be used to contradict such statements and can lend support to plaintiff's claims. The LNC can assist the attorney with the review of state survey reports to identify negative resident outcomes that could be blamed on the facility rather than on the resident’s age or preexisting medical problems. The survey reports provide a roadmap for the plaintiff’s liability case at the trial, and for the recovery of compensatory damages. Operational Documents: The LNC should obtain resident care and administrative policies and procedures for operation of the facility related to all services provided by the facility including: ▪ Administrator – continuing education; responsible person designated in absence of the administrator ▪ Admission, transfer, discharge, discharge planning, and referral services ▪ Resident assessments and care plans ▪ Resident records – content and storage ▪ Personal care services – including assistance with ADLs, assistance with seeking health care and associated transportation when indicated, obtaining functional aids or equipment, clothing as well as maintenance of personal living quarters ▪ Nursing, social, dietary and activity services, including: O Protocols to use in the event of serious health threatening conditions, emergencies, or temporary illness. These protocols must include designation of a 49 Issues in Residential and Community Based Care 50 practitioner for each resident and notification of an appropriately licensed professional in the event of an illness or injury of a resident. O Provision for pharmacy and medication services developed in consultation with a consultant pharmacist that include; assisting residents in obtaining medications from a pharmacy, storage of medications, medication administration, disposing of medications that are discontinued or expired, and allowing the resident to be responsible for self-administration based on assessment of the resident’s capabilities with respect to this function. ▪ Fire safety including fire drills, fire evacuation plans and drills Finally the LNC must understand the specific State’s Nurse Practice Act as it related to the scope of practice; delegating medical and nursing services as tasks (especially medication administration and health or crisis interventions); premises of delegation, and supervision by an RN of unlicensed persons performing assisted living tasks. Each person involved in the delegation process is accountable for their own action; supervision is inherent – if an RN decides to delegate, the RN is responsible for supervising the delegate and their actions, whether the RN is physically present or not. The RN may assign an LPN to monitor for the RN but the RN must be available for consultation and direction; and finally per most State Nurse Practice Acts, the functions of assessment, evaluation and nursing judgment can not be delegated. Chapter Summary The LNC can be invaluable in providing the attorney with an overview and understanding of the complex world of assisted living. Being able to articulate the 50 Issues in Residential and Community Based Care 51 differences between long term care and assisted living requirements; having a knowledge-base of the assisted living services and philosophy; and having the ability to analyze the clinical aspects of an assisted living case, are why an LNC would be an essential part of the legal team. References ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ Alzheimer’s Association, website content, www.alz.org. 2008. American Association of Homes and Services for the Aging (AAHSA), Operational Practices in Assisted Living, compiled and edited by Ruth A Gulyas, 1999. American Association of Retired Persons (AARP), website content, www.aarp.org. 2008. Assisted Living Federation of America (ALFA), website content, www.alfa.org. 2008. Assisted Living Workgroup (ALW), US Senate Special Committee on Aging Report, Assuring Quality in Assisted Living: Guidelines for Federal and State Policy, State Regulation, and Operations, April 29, 2003. Bianculli, J., Negotiated Risk in Assisted Living, AAHSA Operational Practices in Assisted Living; Chapter 8, p157-179, 1999. Donovan, J., Managing Medications in Assisted Living, Nursing Homes, July-August, 1997. General Accounting Office (GAO), Assisted Living: Examples of States Efforts to Improve Consumer Protections, GAO Report Number GAO-04-684, May 27, 2004. HRC Volume 3 - Long-term Care 1, Overview of Long Term Care Risks, Published by ECRI, Plymouth Meeting, PA, January 1997. Murer, M., Assisted Living: The Regulatory Outlook; Nursing Homes. July-August 1997 National Center for Assisted Living (NCAL). 2008 State Regulatory Review, 2008. National Center for Assisted Living (NCAL), website content, www.ncal.org. 2008. Peterson, S., Developing Risk Management Protocols In Assisted Living: Assisted Living Has Its Own Litigation Traps For The Unwary, 2005. Podrazik, P. and Stefanacci, R., Negotiating the Complexities of the Long Term Care Continuum, Assisted Living Consult, March/April 2005. Pratt, J., Long Term Care, Long-Term Care: Managing Across the Continuum, Second Edition, 2004 Rubinger, H. and Gardner, R., Assisted Living’s First Steps Toward Uniformity: Assisted Living Workgroup Submits Recommendations To Congress, Continuing Care, July/August 2003. Thayer, J., Written Statement of Jan Thayer on Behalf of The National Center for Assisted Living; Federal Trade Commission/Department of Justice - Hearing on Long Term Care/Assisted Living, For the Hearing Record, Submitted June 11, 2003. 51 Issues in Residential and Community Based Care 52 ▪ Wright, B., AARP Study: #2007-08: Assisted Living In Unlicensed Housing: The Regulatory Experience Of Four States, April 2007. Resources ▪ ▪ ▪ ▪ ▪ Assisted Living Federation of America (ALFA), www.alfa.org. - The Assisted Living Federation of America (ALFA) monitors legislative and regulatory proposals in all 50 states. The information is updated weekly and is an excellent way for ALFA to stay on top of what is being proposed across the country. In addition, ALFA continues to be a resource for best practices and examples of successful laws and regulations. U.S. Senate Special Committee on Aging – www.senate.gov. Assisted Living Workgroup (ALW) 381-page report, entitled Assuring Quality in Assisted Living: Guidelines for Federal and State Policy, State Regulation, and Operations Center for Excellence in Assisted Living (CEAL) – www.theceal.org. ALW report to congress in April 2003, recommended that a National Center for Excellence in Assisted Living (CEAL) be formed and funded to serve as an ongoing source of information and guidance to states regulating assisted living. American Assisted Living Nurses Association (AALNA), www.alnursing.org. American Nurses Association (ANA) www.nursingworld.org. Test Questions 1. Which of the following services would be available in an Assisted Living facility? a. Medication administration b. Hospice care c. Assistance with ADL’s d. All of the above 2. Which of the following statements about assisted living regulatory requirements is NOT true? a. All assisted living administrators are licensed by the state b. An assisted living facility must comply with OSHA and Life Safety Code c. Most states have regulations in place regarding assisted living facilities and services d. Medication can be administered by unlicensed staff 52 Issues in Residential and Community Based Care 53 3. Select the answer that would NOT describe a staff member’s roles and responsibilities in an assisted living facility. a. Nurse Practice Act b. Job description c. Federal Nursing Home regulations d. Individualized Service Plan 4. Which of the following would be an essential element when reviewing an Assisted Living case? a. Admission/residency agreement b. Marketing materials c. Individualized Service Plan d. All of the above Answers: 1.d ; 2.a ; 3.c; 4.d 53
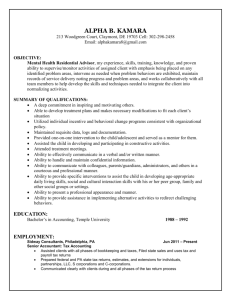
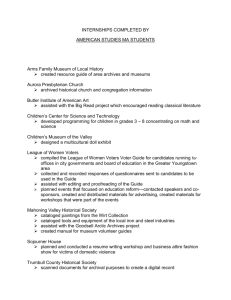
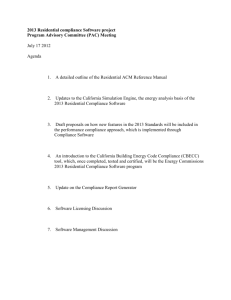
![[Agency] recognizes the hazards of lead](http://s3.studylib.net/store/data/007301017_1-adfa0391c2b089b3fd379ee34c4ce940-300x300.png)