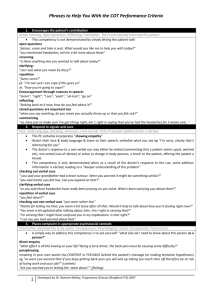
scripts for explanation of diagnosis
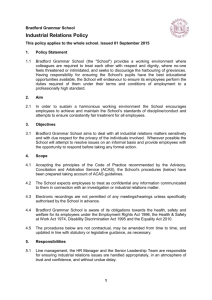
advertisement

Scripts for Explanation of Diagnosis Key points Explanation is not simply you telling the patient about what’s going on and expecting them to be quiet and to listen. It is not unidirectional but Bidirectional. That means it is a two way process. What you say and they say depends on what each of you has said prior to that. Avoid any medical jargon. Think of the patient as a family member or friend. What would you say to them? It really is as simple as that. But somehow, trainees often think they have to ‘dress up’ explanations… and the reality is that you simply don’t. Your job is to explain things adequately, cover anything else the patient wants to know AND check they’ve understood everything. Below are some scripts that you can use for explanation the diagnosis. The second level questions give you an alternative way of asking the first question. Explanation is difficult to summarise in 2 pages. The least I could get it down to is 4, but what’s in these 4 pages is like gold dust! We will look at checking understanding in another document. Look at the next page for the scripts. Learn these scripts ‘off by heart’. Practise saying them with patients. You will eventually add your own flavour to them in time. Dr. Ramesh Mehay, Programme Director (Bradford VTS), 2010 1. Explanation - Signposting Signpost that you’re going onto the explanation and state your diagnosis briefly. 2. Explanation – identifying the patient’s starting point 3. Explanation – building on what the patient already knows What you do here depends on what the patient has told you. Confirm anything which they've said which is right and correct anything which isn't. Try and weave in what they have told you so far into your explanation as much as possible. You will need to put flexibility in your explanation to keep checking what the patient already knows so that you can then continue to build on that. Dr. Ramesh Mehay, Programme Director (Bradford VTS), 2010 A bit more about weaving: try and incorporate the patient’s health belief system in your explanation. By patient’s health belief system I mean their ideas, concerns & expectations. Patients are experts in their own lives and if you want them to accept your diagnosis/explanation of what is going on (especially when it is at variance with theirs), then you need to start off with their perceptions/thoughts. If those perceptions and thoughts are on a different track to yours, you need to explain why you don’t subscribe to their view and then go on to modify their thinking so that it aligns with yours. To be able to do all of this, you need to go back and start from what they told you when you explored their ideas, concerns and expectations. If you do this, the patient is more likely to engage with you and the consultation becomes easy as they understand where you are coming from and start having faith in you. Examples: ‘You mentioned earlier that you were concerned that you might have angina. I can see why you might have thought that, but in fact I think it is more likely to be muscular pain. Let me explain why I don't think it is angina.’ ‘This rash is called psoriasis, and is caused by overactive cells in the skin, but it is probably not affected by what you eat’ (having elicited food concerns earlier). ‘Yeah, I think your right: your irritable bowel syndrome is very likely to be related to the stress you were telling me about earlier’. 4. Explanation – helping the patient to remember what is being said Dr. Ramesh Mehay, Programme Director (Bradford VTS), 2010 Dr. Ramesh Mehay, Programme Director (Bradford VTS), 2010 5. Explanation at appropriate times & the non-verbals Give explanation at appropriate times Explanation happens at various points in the consultation (usually during the middle and the last bit). It doesn’t just happen the once. Therefore, give explanation at the appropriate times – you’ll know when because the patient will say something that tells you more explanation is needed. Patient: ‘so you don’t think I need antibiotics?’ Doctor: ‘In your particular case, having listened to your chest, I don’t. Let me explain why…’ Read the patient’s non verbals People might be able to lie or cover up things with their mouths but their non-verbals always give the game away; the non verbals display ‘the truth’. Read the non-verbals and respond to them. So, if a patient looks confused during your explanation, STOP and say what you see: ‘Mmm… Am I right in saying that I think I’ve confused you a bit?’ ‘Am I right in sensing that you’re still worried about something?’ ‘If you don’t mind me saying, it looks like there’s still something bothering you’ Dr. Ramesh Mehay, Programme Director (Bradford VTS), 2010