Adverse Event Review

DEPARTMENT: Quality Management
PAGE: 1 of 3
EFFECTIVE DATE: January 1, 2003
POLICY DESCRIPTION: Adverse Event Review
REPLACES POLICY DATED:
REFERENCE NUMBER: QM.IRB.005
SCOPE: All Company-affiliated facilities engaged in human subject research overseen by an
Institutional Review Board (IRB).
PURPOSE: To provide guidance for IRB activities and development of local Standard Operating
Procedures (SOP) regarding adverse events related to human subject research.
POLICY: Each facility must develop SOP that outline the review of adverse events occurring in a research study at the institution and the review of cooperative research information in safety alerts provided by the sponsor to the individual principal investigators (PIs) and published on the FDA website.
PROCEDURE:
The IRB must develop a local SOP that reflects a specific structure for the process of reviewing adverse events and which clearly defines the responsibilities of all parties, including the sponsor and
PI, in communicating event information. Information may come from a variety of sources that include, but are not limited to: safety monitoring alerts from the sponsor to the PI, PI outpatient information, FDA Medwatch system, and an onsite occurrence reporting system.
The IRB must clearly define the timing of required reports, and the content that such reports must include, and the form they must take.
Internal events must be reviewed as they relate to the study and, if appropriate, the institution’s peer review process should be utilized. Complex cases may require more review than submission of a
PI’s case summary When an adverse event occurs, the IRB and/or the facility must consider performance improvement opportunities, sentinel event determinations, risk management, and proactive patient safety initiatives such as use of the failure, mode, effects and criticality analysis
(FMECA). When deemed necessary, referrals to the appropriate committee or leader(s) must occur.
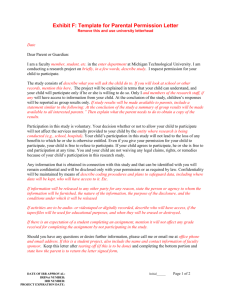
The IRB must communicate reporting expectations to the PI at the time such individual is oriented regarding local IRB policies. Such expectations must be restated with each protocol approval.
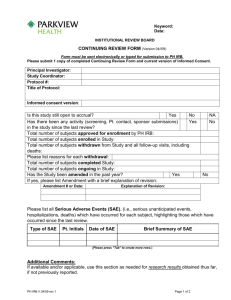
Review of events is a component of the continuing review and may be more frequent depending on the risk determination by the IRB or the level of severity of the event.
Review Process:
1.
Promptness of review should depend on the severity of the event. The institution may choose to stratify severity of events and how quickly they should be reviewed and analyzed by the
IRB. This should be defined in the local SOP.
2.
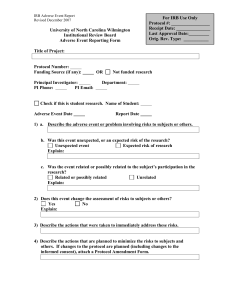
Questions to consider when reviewing an event include at a minimum: a.
Date and Time of onset of adverse event. b.
Was the event/problem from this institution, or another participating site if a multi-
10/2002
DEPARTMENT: Quality Management
PAGE: 2 of 3
EFFECTIVE DATE: January 1, 2003
POLICY DESCRIPTION: Adverse Event Review
REPLACES POLICY DATED:
REFERENCE NUMBER: QM.IRB.005 center sponsor or study? c.
Was the event/problem deemed mild, moderate, severe, or fatal? Will need date of death, including copy of the death certificate and autopsy report. d.
Was the event/problem expected or unexpected? e.
Was the event/problem related to the research intervention?
It helps to specify with descriptives such as:
Causative: probable, inconclusive, and unlikely;
Study Related: definitely, probably, possibly, probably not related to the study. f.
What was the outcome? Is it resolved, ongoing or did the subject die? g.
Based on this event, will additional monitoring of other patients be performed in the study to detect similar problems early? If yes, please describe. h.
Are the possibility, severity and specificity of this event described in the consent form, protocol, and investigator brochure for this study? i.
Will the consent procedures be revised as a result of this event? If yes, attach the new version of the consent form. j.
Will patients already enrolled in the study be informed about the possibility of this adverse event? If yes, how? k.
Name and date of individual submitting the report.
3.
Clinical detail should also be made available to the IRB for review; such detail may include the following: a.
Title of protocol, IRB #, IND or IDE number, Sponsor. b.
Name of drug/device/procedure. c.
Medication details, if applicable. d.
Device parameters, if applicable. e.
Procedure report, if applicable. f.
Duration of therapy and dates of administration. g.
Date of onset and time. h.
Clinical description of events including signs and symptoms, diagnostic tests performed surrounding event with dates and times. i.
Treatment initiated for the event. j.
Outcome of the event. k.
Has this type of event been reported before? l.
Could it occur again? This patient or others? m.
Time frame related to treatment, within 30 days, more than thirty days after treatment began more than thirty days after treatment stopped.
IRBs are responsible for ensuring that reports of unanticipated problems involving risks to human subjects or others are reported to the appropriate government agency. This reporting must be accomplished by the investigator reporting the event to the sponsor. Such reporting requirement must be included in PI orientation and approval letters.
10/2002
DEPARTMENT: Quality Management
PAGE: 3 of 3
EFFECTIVE DATE: January 1, 2003
POLICY DESCRIPTION: Adverse Event Review
REPLACES POLICY DATED:
REFERENCE NUMBER: QM.IRB.005
The IRB meeting minutes must clearly reflect the comprehensive review of each adverse event, list data analyzed or considered, reflect discussions and approval vote or other actions taken. The IRB must analyze all events from all available sources, such as local patient events and the safety monitoring reports from the sponsors, in aggregate to determine the safety of the protocol.
Events occurring to federally-funded research human subjects must be reported in accordance with the Terms of Assurance that can be accessed at http://ohrp.osophs.dhhs.gov/humansubjects/assurance/filasurt.htm.
The annual report to the governing body must contain sufficient evidence of adequate adverse event review and analysis by the IRB to support the continuation or termination of each research protocol.
REFERENCES:
Reporting of unanticipated problems, 21 CFR 56.108(a)(b)
Data monitoring committee, 21 CFR 50.24 (a)(7)(iv)
Authority for third party observer for the consent process, 21 CFR 56.109(f)
Degree of risk, FWA, 45 CFR 46.103(b)
Reporting unanticipated problems, 45 CFR 46.108
Review of research and degree of risk. 45 CFR 46.109(e)
FDA Guidance for Continuing Review
OHRP Guidance – July 11, 2002
VA-ORCA Best Practice Guidelines
NCQA Accreditation Standards
Policies
IRB Guidance Policy, QM.IRB.001
IRB Protocol - Initial and Continuing Review Policy, QM.IRB.002
Informed Consent IRB Review Policy, QM.IRB.003
Development of Local Standard Operating Procedures Policy, QM.IRB.004
Use of Non-Local, Cooperative and Multi-Institutional IRBs Policy, QM.IRB.006
Recruitment of Vulnerable Subject Populations Policy, QM.IRB.007
10/2002