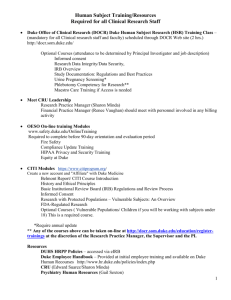
State
advertisement

Template for Simulation Patient Design Developed by Jeffrey M. Taekman, M.D. Duke University Made available through a Creative Commons License http://simcenter.duke.edu/support.html Case Information Section 1: Demographics Case Title: Local Anesthetic Toxicity in Patient with Small Bowel Obstruction/Volvulus Patient Name: Baby Packard Scenario Name: Local Anesthetic Toxicity in Infant Simulation Developer(s): Ellen Wang, Anita Honkanen, Michael Chen Date(s) of Development: 8 – 2011 through 10 - 2011 Appropriate for following learning groups (circle all that apply) Faculty: CME Residents:(PGY) Specialties: Medical Students (yr): Nurse Anesthesia Faculty: Nursing Students (yr): Other: 1 2 3 4 5 Anesthesiology Nurse Anesthesia Critical Care Emergency Medicine 1 2 3 4 CEU 1 2 _____________________ 6 7 Surgery Obstetrics Template for Simulation Patient Design Developed by Jeffrey M. Taekman, M.D. Duke University Made available through a Creative Commons License http://simcenter.duke.edu/support.html Section 2: Curricular Information Educational Rationale: Learning Objectives: (ACGME Core Competencies: Medical knowledge (mk), Patient care (pc), Practice-based learning and improvement (pli), Interpersonal and communication skills (cs), Professionalism (pr), Systems-based practice (sbp)) objective 1: Review of Local Anesthetic Toxicity manifestations and treatments (mk, pc) objective 2: Review Guidelines and regulations for drugs that nurses/surgeons use intraoperatively and medication errors (sbp) objective 3: Review of ischemic bowel and likely repercussions (mk) objective 4: Review resources available for cardiopulmonary support (sbp) objective 5: Understand critical behaviors for effective team performance in ACRM, leadership and communication in a crisis situation (pr, cs) Guided Study Questions: question 1 question 2 etc References used (included PubMed ID when possible): reference 1 reference 2 etc Didactics: powerpoint slide set web site etc Assessment Instruments: Instrument name Template for Simulation Patient Design Developed by Jeffrey M. Taekman, M.D. Duke University Made available through a Creative Commons License http://simcenter.duke.edu/support.html Section 3: Preparation Monitors Required: X X X X X Non-Invasive BP Cuff Arterial Line CVP PA Catheter 3 lead EKG Temperature Probe Pulse Oximeter Capnograph BIS Other equipment required: SimBaby, Anesthesia Machine, IV poles/sets, IV materials/supplies, syringes and needles for sim meds (including emergency drugs, intralipids), airway equipment (mask, ambu, LMA and ETT, laryngoscope blades/handles, stylets), suction, defibrillator, stethoscopes, drapes/surgical instruments, patient’s chart and anesthesia record X X Anesthesia Machine Pumps Brochoscope Defibrillator Hotline Nerve Stimulator Echo Machine and Probe X X ETT LMA Laryngoscope Supporting Files (cxr, ekg echo, assessment, handouts, etc) 1. CXR and KUB of abdomen Time Duration Set-up Preparation Simulation Debrief 20 minutes 10 minutes 20 minutes 40 minutes Template for Simulation Patient Design Developed by Jeffrey M. Taekman, M.D. Duke University Made available through a Creative Commons License http://simcenter.duke.edu/support.html Case Stem Case Stem (one to two paragraphs on pertinent patient and scenario information-this should be the stem for the learner and should include location, physician/help availability, family present, etc.): You are taking over the intraop management of a 13 month old boy, scheduled for urgent ex-lap for volvulus with possible dead bowel. He is a full-term infant, otherwise healthy, with no previous surgeries or procedures, no family history of problems with anesthetics. Not currently taking any medications. No allergies. He had a 2 day history of poor intake, fussiness, with vomiting starting today with abdominal guarding noted on exam with presentation at physicians office. Sent to ED for evaluation; plain films revealed largely distended loop of bowel with proximal bowel distension, but no air in colon. Attempt at reduction in radiology earlier today unsuccessful, with subsequent film revealing free air under the diaphragm. Came to OR with 22 G PIV placed in ED in situ in the left hand. This IV used for RSI with an easy intubation, but relatively poor flow noted after induction. Unable to place second IV after multiple attempts, so surgeons placing central venous line for access. Meds given on induction included etomidate (6 mg), rocuronium (10 mg), fentanyl (25 mcg); 10 mcg phenylephrine given after induction for BP 60/30 with HR 170, 100 mls of NS pushed in with resistance using syringe, IV barely flowing at this time. Cefoxitin, 480mg given. Primary anesthesiologist must leave for family emergency – child involved in MVA while riding bicycle. Background and briefing information for Facilitator/coordinator’s eyes only: Patient in the OR, at beginning of the case, when "hot seat" participant comes in to take over care - original anesthesiologist must leave due to a family emergency. The patient is stable at the time of handoff, intubated, surgeon in the process of finishing line placement. The original anesthesiologist will tell the “hot seat” participant that the original PIV is not working and difficult to place, so the surgeon has just placed a central line. Allowing some time for the “hot seat” participant to get settled, the surgeon will continue with line placement. Once line is secured, the surgeon will flush the line with what should be saline, but is actually bupivacaine and hand off line under drape to anesthesiologist. Will follow quickly with incision. Ectopy will appear on ECG within 30 seconds of line flush, followed by more ECG changes – sinus bradycardia, conduction blocks (prolonged QT, widened QRS), hypotension. Confusion as to reason for dysrhythmias – electrolyte abnormalities second to the dead bowel vs local anesthetic toxicity. At some point (if “hot seat” participant needs prompting), the scrub tech will ask the surgeon what happened to the basin of local anesthetic, which is empty. Recognition of local anesthetic toxicity should prompt a call for intralipids and amiodarone. ECG will progress to ventricular fibrillation with loss of pulses, and CPR should be initiated. Cardiopulmonary bypass should be considered, and perfusion services and cardiothoracic surgery should be called for. Template for Simulation Patient Design Developed by Jeffrey M. Taekman, M.D. Duke University Made available through a Creative Commons License http://simcenter.duke.edu/support.html Patient Data Background and Baseline State Patient History (should follow standard H and P format): Review of Systems: CNS: normal Cardiovascular: normal Pulmonary: normal Renal / Hepatic: normal Endocrine: normal Heme/Coag: normal Current Medications and Allergies: No meds, no allergies Physical Examination: General: mildly obtunded, easily aroused to responsiveness but ill appearing Weight, Height: 12 kg, 79 cm Vital Signs: HR – 155, BP – 75/30, RR – 28, Temp – 38, SpO2 - 98 Airway: WNL Lungs: CTA, shallow respirations Heart: Regular, 2/6 flow murmur, normal heart tones Laboratory, Radiology, and other relevant studies: HCT: 37, WBC: 10, Plts: 122,000, INR: 1.3, Na: 143, K: 3.8, Cl: 106, HCO3: 26 CXR/KUB: clear lung fields, slightly elevated diaphragms, free air under in around bowel loops, distended EKG: not available Template for Simulation Patient Design Developed by Jeffrey M. Taekman, M.D. Duke University Made available through a Creative Commons License http://simcenter.duke.edu/support.html Baseline Simulator State: Vitals: HR: 135, BP: 65/35, PC: 15/4 with TV 90 to 100, RR: 16, ETCO2: 34, Temp: 36 Neuro: anesthetized Respiratory: intubated, ventilated Cardiovascular: SR Gastrointestinal: abodomen prepped/draped, ready for incision Genitourinary: foley catheter in place, less than 5 ml urine output noted Metabolic: afebrile Environmental: OR with circulating nurse, scrub tech, surgeon all present, primary anesthesiologist about to leave after giving hand-off report Template for Simulation Patient Design Developed by Jeffrey M. Taekman, M.D. Duke University Made available through a Creative Commons License http://simcenter.duke.edu/support.html State Patient Status 1. BASELINE: Anesthetized: immediately at handoff Relatively stable after induction and resuscitation with phenylephrine/volume, awaiting central line from surgeon 2. Local anesthetic is injected into central line by surgeon as flush (syringe not labeled, mistaken as flush syringe while tech and circulator completing initial instrument and sponge count) 3. Non perfusing rhythm noted by team Patient stable until LA hits heart, progressive ECG changes – ectopy, morphology changes, runs of V-tach 4. Scrub Tech Student learning outcomes or actions desired and trigger to move to next state Learner Actions: o become familiarized with environment, review patient chart, review patient history, introduce self to team, review plan with surgeon Learner Actions: o note ECG changes, initiate discussion with surgeon, ask to hold on incision/manipulation of bowel if already open abdomen Operator: o maintain VS’s within 10% of baseline Teaching Points: o get complete handoff, communicate with team to develop baseline shared mental model of plan Trigger: handoff complete Operator: o add dysrhythmias, BP changes Teaching Points: o situational awareness – note ECG changes and course of surgery, develop Trigger: surgeon tells anesthesiologist that handing off line under the drapes ECG VFib, no SpO2 ithout effective compressions, no ETCO2 without effective compressions and decreased with compressions Return to perfusing Learner Actions: o initiate code response, call for help, direct team members in appropriate actions, ask for input from team on etiologies – develop differential list Learner Actions: Operator: o VFib, no other vitals unless managed properly, see below Teaching Points: o Manage code, manage OR team Trigger: time from injection at 1 minute, VS’s (ETCO2, SpO2) based on effective chest compressions Operator: Template for Simulation Patient Design Developed by Jeffrey M. Taekman, M.D. Duke University Made available through a Creative Commons License http://simcenter.duke.edu/support.html notes missing syringe of local anesthetic on back table, asks surgeon about why missing, confers with circulator rhythm if appropriate actions taken o o Moves LA toxicity to head of differential if notes communication from rest of OR team Initiates intralipid treatment, calls for backup support/ICU/cardiac for bypass if required o Return to perfusing rhythm Teaching Points: o Communication within team, understanding of LA toxicity and treatments, use of environmental cues (cognitive aids?) Trigger: administration of effective dose of intralipid and continued effective chest compressions for at least 2 minute