Classic microtia reconstruction
advertisement
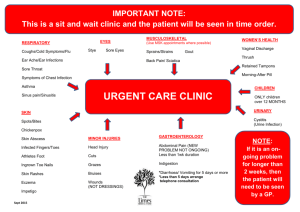
OTOLOGY SEMINAR Ear reconstruction: review and prospects R3 楊宗霖 2002-02-20 Microtia / / / normal external ear anatomy embryology: 4-8 wks: inner ear; 4-14 wks: external ear incidence of microtia - 0.03% (1 in 10000 to 20000) - half of these patients associated with congenital anomalies - right ear, boy (2.5x), unilateral (4x): more / classification: simplified by evaluation external auricle alone - I mild deformity, with slightly dysmorphic helix and antihelix as lob ear, cupped ear - - No need of other tissue in reconstruction II: (atypical microtia) dysplasia: all major structures present to some degree need additional skin and cartilage with or without stenosis of external ear canal III: (classic microtia) dysplasia: few or no recognizable landmarks lobe is often present with anterior position Classic microtia reconstruction Stage I : cartilage implantation / place the framework best fit the face symmetry / three templates made from the radiological evaluation - positioning plate: for the contour of the normal ear - sizing plate: to test the skin pocket where cartilaginous framework is placed - carving template: landmark or the ear / donor: chest site / - use the 6th,7th synchondrosis, expose rib 5-8 rib is harvested with the perichondrium, typically 9 cm in length the framework and helix were then carved recipient site: the ear incision line: anterior-superior margin of the lobe create a thin flap to cover the cartilage flap framework is placed in the pocket insertion silicon drains with vacuum to promote adhesion of non-nourishing flap Stage II: lobe transfer / 2-3 months after stage I procedure / a simple transposition flap into the donor site from inferior border of framework / the lobe is wrapped around the posterior-inferior margin of framework Stage III post-auricular skin grafting / to create post-auricular sulcus / to project the ear away from the surface of the mastoid / post-auricular skin over the mastoid is undermined and advanced into post-auricular sulcus / greater projection with placement of a wedge of rib cartilage turnover the occipitalis fascia from behind the ear Stage IV tragus reconstruction / the aim of the operation is to form a tragus and concha bowl / an composite graft is removed form the contra-lateral concha cymba / incision is made along the posterior border of future tragus, and the composite flap is placed in the place to make some projection / conchal bowl was debulked of scar and redundant skin tag / care for the facial nerve anomalies Management of the hairline / normal hairline is above the apex of the external ear / lower hairline is the most common problems / management depends on how much was involved - if only helix: electrolysis & clipping - if 1/3 or more of the ear: skin graft - better to eradicate the ear with non-surgical method - laser: reduce of epidermal appendage, eliminate the apocrine sweat glands Long-term results / Complications - major is rare - minor as hematoma or infection may loss the graft - scar formation and poor contouring improved with time / Durability of the constructed auricle - most ears retain their form in the following years - no softening or shrinkage of the cartilaginous framework / some report that reconstructed ear in young patients can be expected to grow Physiological and emotional benefit Culture-expanded ear condrocyte transplants / A polymer template was formed in the shape of a human auricle - using a nonwoven mesh of polyglycolic acid (PGA)molded - then immersed in a 1% solution of polylactic acid.(PLA) - template was seeded with chondrocytes from bovine articular cartilage - then implanted into subcutaneous pockets on the dorsa of 10 athymic mice. / Specimens harvested 12 weeks after implantation - Gross morphologic and histologic analysis: new cartilage formation. The three-dimensional structure was maintained after removal of an external stent - The overall geometry of the experimental specimens closely resembled the complex structure of the child's auricle / Both articular and ear sources of chondrocytes have been used in past with success - suspension of ear chondrocytes injected into a subcutaneous location biochemical and histological data with greater similarity to those of native cartilage. - The subcutaneous environment of native ear cartilage accommodates subcutaneously injected ear chondrocyte transplants better than aiticular transplant - the phenomenon is attributable to the local environment in which isolated chondrocytes from different sources are introduced. - Native structural and biochemical cues within the local environment are believed to guide the proliferation of the differentiated chondrocytes. / To construct an autologous cartilage graft, cells must be multiplied in vitro - Culture cells will lose its phenotypes Cells were isolated from the ear cartilage, multiplication in mono-layer culture - Cultured in 10% fetal calf serum, unable to induce re-differentiation. Some seeded in alginate and cultured for 3 weeks in serum-free medium with insulin-like growth factor 1 (IGF-1) and transforming growth factor-beta2 - Chondrocytes from the ears of young, but not adult, rabbits, synthesized significantly more glycosaminoglycan - Using human ear cells, glycosaminoglycan synthesis could also be stimulated by replacing serum with insulin-like growth factor and TGF-beta. / Autogenous cartilage using alternative polymers - Previous successful efforts have used an immunocompromised nude mouse xenograft model by using polyglycolic acid/polylacic acid (PGA/PLA) - Less success in an immunocompetent autogenous animal model is due to inflammatory response. - alternative polymer material, Pluronic F-127 (polyethylene oxide and polypropylene oxide). - Injection of autologous porcine auricular chondrocytes suspended in a biodegradable, biocompatible hydrogel of Pluronic F-127 resulted in the formation of cartilage in the approximate size and shape of a human ear helix. - Final product: cartilage without residual foreign material - Some other new material as polyethylene, scrylic, extrapurified silasic success in limited inflammation & cover with pure elastic cartilage References 1. Cummings CW et al. Otolaryngology Head & Neck Surgery. Mosby Co. 2. Aguilar EF. Auricular reconstruction in congenital anomalies of the ear. Facial Plast Surg Clin North Am. 2001:9;159-69. 3. Spring PM et al. Congenital aural atresia. J La State Med Soc.1997;149:6-9. 4. Aguilar EF 3rd. Auricular reconstruction of congenital microtia (grade III). 5. 6. 7. 8. Laryngoscope.1996;106:1-26. Tanino R, Miyasaka M. Reconstruction of microtia using tissue expander. Clin Plast Surg. 1990;17:339-53. Matsumoto K, Maeda M, Fujikawa M. Staged, laminated, costal cartilage framework for ear reconstruction. Clin Plast Surg. 1990;17:273-85. van Osch GJ, van der Veen SW, Verwoerd-Verhoef HL. In vitro redifferentiation of culture-expanded rabbit and human auricular chondrocytes for cartilage reconstruction. Plast Reconstr Surg. 2001;107:433-40. Arevalo-Silva CA, Eavey RD, Cao Y et al. Internal support of tissue-engineered cartilage. Arch Otolaryngol Head Neck Surg. 2000;126:1448-52. 9. Saim AB, Cao Y, Weng Y et al. Engineering autogenous cartilage in the shape of a helix using an injectable hydrogel scaffold. Laryngoscope. 2000;110:1694-7. 10. Brent B. Technical advances in ear reconstruction with autogenous rib cartilage grafts: personal experience with 1200 cases. Plast Reconstr Surg. 1999;104:319-34