Becoming an expert consumer of Medical Statistics
advertisement
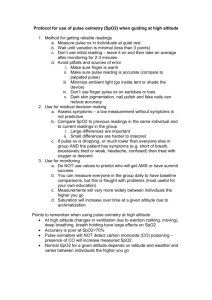
FPIN Journal Club DIAGNOSTIC STUDY WORKSHEET SPEAKER NOTES Article: Pulse oximetry for newborns: Should it be routine? Original Article Citation: Ewer AK, Middleton LJ, Furmston AT, Bhoyar A, Daniels JP, Thangaratinam S, Deeks JJ, Khan KS; PulseOx Study Group. Pulse oximetry screening for congenital heart defects in newborn infants (PulseOx): a test accuracy study. Lancet. 2011;378:785-794. Author: Corey Lyon, MD – University of Colorado, Department of Family Medicine 1. What question did the study attempt to answer? Patients – Newborn infants >34 weeks Intervention – Pulse oximetry on right hand and either foot within 24 hours of delivery Comparison – Composite of echocardiogram and follow up if pulse oximetry <95% Outcome – critical or major heart defects. Did the study address an appropriate and clearly focused question Yes No ----What is the accuracy of pulse oximetry for screening major congenital heart defects in asymptomatic newborn babies----2. Determining Relevance: a. Is the diagnostic test feasible and common to your practice? Yes No --- This test is readily available in the hospital setting and would be very low cost--b. Is the proportion of patients with the target illness comparable to the patient group seen by family physicians? Yes No ---- Definitely relevant, because FPs care for newborns.--c. Did the authors study a clinically meaningful Yes No and/or a patient oriented outcome? --- Yes, many FPs care for newborns in the hospital setting and early detection of congenital heart disease could elicit a promp referral in the hospital setting.--- 3. Determining Validity: a. What test is being evaluated Pulse oximetry with hypoxemia: described as a pulse ox <95% in either the baby's hand or foot. The study stated that these parameters were chosen because in prior studies higher thresholds were used and treatable disorders were missed. b. What is the reference standard with which the test being evaluated is compared? Echo and follow-up were used to identify immediate- and late-presenting congenital heart defects. If SaO2 <95% and abnormal clinical exam, the newborn underwent echo. If pulse ox <95% and normal clinical exam, repeat pulse ox in 1-2 hours; if still <95%, the newborn underwent echo. The echo and pulse ox were done within 72 hours of each other. c. The test and reference standard are measured independently (blind) of each other? Yes No Unclear --- Echo and follow-up were used to identify immediate- and late-presenting congenital heart defects.--d. Did the patient sample include an appropriate spectrum of patients to whom the diagnostic test will be applied in clinical practice? Yes No Unclear ---Newborn babies--e. Patients for testing are selected either as a consecutive series or randomly, from a clearly defined study Yes No Unclear --- Asymptomatic NB infants >34 weeks were recruited prospectively and included NB infants in whom congenital heart defects were suspected antenatally after ultrasound.--f. Results are reported for all patients that are entered into the study Yes No Unclear 4. What are the results? ---Of 20,055 newborns screened, 53 had major congenital heart disease (24 critical, 29 serious). The prevalence was 2.6 per 1000 live births.(53/20,055 = 0.0026 = 2.6 per 1000 live births)--a. What is the estimated sensitivity of the test being evaluated? (state 95% CI) Sensitivity = proportion of results in patients with the disease that are correctly identified by the new test; In other words, a sensitive test has very few false negatives: Sensitivity of pulse ox was 75% (95% confidence interval [CI], 53.29-90.23) for critical cases and 49.06% (95% CI, 35.02-63.16) for all major congenital heart defects. b. What is the estimated specificity of the test being evaluated (state 95% CI) Specificity = proportion of results in patients without the disease that are correctly identified by the new test; In other words, a specific test has very few false positives The specificity of pulse ox for critical cases was 99.12% (95% CI, 98.98-99.24) for critical cases and 99.16% (95% CI, 99.02-99.28) for all major congenital heart defects). ***Teaching point: Likelihood ratios: These ratios tell you how much the odds of a disease increase when a test is positive (LR+) or how much the odds of a disease decrease when a test is negative (LR-) - Likelihood ratios are independent of prevalence - Can be calculated from the sensitivity and specificity (formulas below) - Positive Likelihood ratios – How likely is the disease present if a test is positive o It should be > 1, the higher the better o LR + > 10 is an ideal test o LR+ < 2 is no change - Negative Likelihood ratios – How likely is the disease not present with a negative test o It should be < 1, the lower the better o LR- < 0.1 is an ideal test o LR- > 0.5 is no change c. What are the likelihood ratios for the test being evaluated? LR+ = sens / (1-spec) - LR+ > 10 indicates a large change in likelihood, < 2 indicates no change in likelihood LR+ = 0.75/ (1-0.99) = 75 for critical cases LR+ = 0.49/(1-0.99) = 49 for all major cardiac defects LR− = (1-sens) / spec - LR− < 0.1 indicates a large change in likelihood, > 0.5 indicates no change in likelihood LR− = (1-0.75)/0.99 = 0.25 for critical cases LR− = (1-0.49/0.99) = 0.51 for all major critical cases ----Pulse oximetry identifies cases of critical congenital heart disease; early detection is an additional advantage The authors estimate that in a population of 100,000 newborns, approx 120 would have critical CHD and 90 of those 120 would be detected by pulse oximetry. 843 false positives – You would need 10 echos to detect one patient with critical CHD--5. Applying the evidence a. Will the results help me in caring for my patients Yes -- FPs care for newborns --b. If the findings are valid and relevant, will this change your current practice? Yes c. Is the change in practice something that can be done in a medical care setting of a family physician? Yes d. Can the results be implemented? Yes --- Pulse oximetry is inexpensive, and non-invasive e. Are there any barriers to immediate implementation? Yes --- Echocardiography may not be readily available; early d/c may lead to earlier screening, which may increase the number of false positives. f. How was this study funded? The National Institute for Health Research Health Technology Assessment program funded the study. No No No No No