The pro-fibrotic effects of all-trans retinoic acid in a normal rat kidney
advertisement
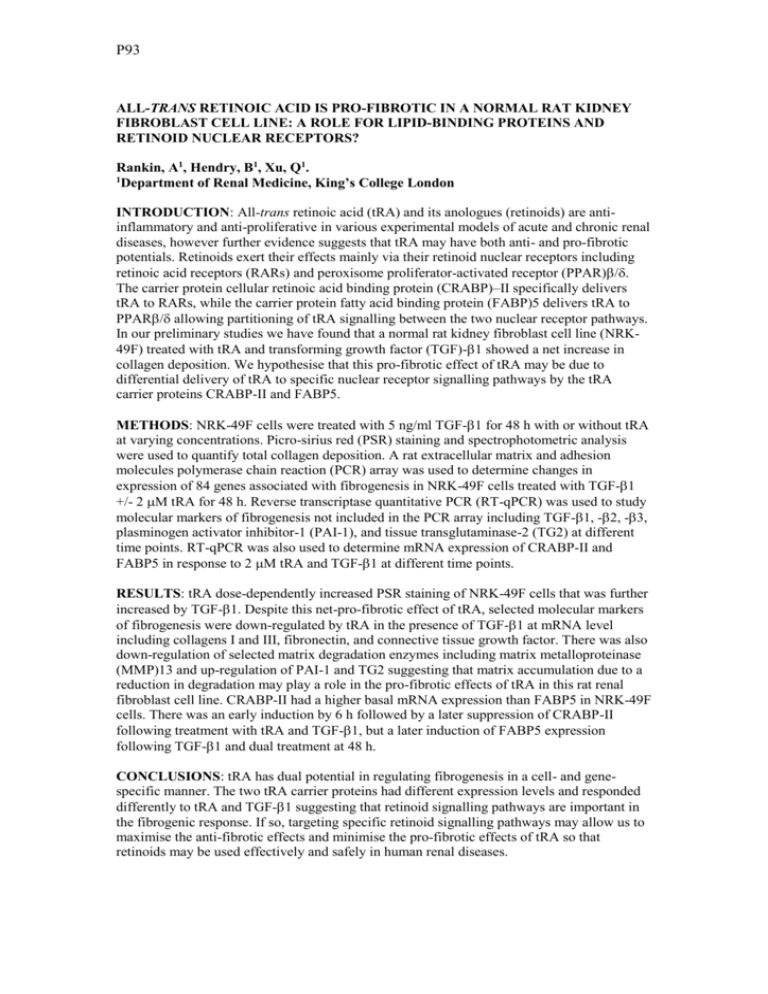
P93 ALL-TRANS RETINOIC ACID IS PRO-FIBROTIC IN A NORMAL RAT KIDNEY FIBROBLAST CELL LINE: A ROLE FOR LIPID-BINDING PROTEINS AND RETINOID NUCLEAR RECEPTORS? Rankin, A1, Hendry, B1, Xu, Q1. 1 Department of Renal Medicine, King’s College London INTRODUCTION: All-trans retinoic acid (tRA) and its anologues (retinoids) are antiinflammatory and anti-proliferative in various experimental models of acute and chronic renal diseases, however further evidence suggests that tRA may have both anti- and pro-fibrotic potentials. Retinoids exert their effects mainly via their retinoid nuclear receptors including retinoic acid receptors (RARs) and peroxisome proliferator-activated receptor (PPAR)/. The carrier protein cellular retinoic acid binding protein (CRABP)–II specifically delivers tRA to RARs, while the carrier protein fatty acid binding protein (FABP)5 delivers tRA to PPAR/ allowing partitioning of tRA signalling between the two nuclear receptor pathways. In our preliminary studies we have found that a normal rat kidney fibroblast cell line (NRK49F) treated with tRA and transforming growth factor (TGF)-1 showed a net increase in collagen deposition. We hypothesise that this pro-fibrotic effect of tRA may be due to differential delivery of tRA to specific nuclear receptor signalling pathways by the tRA carrier proteins CRABP-II and FABP5. METHODS: NRK-49F cells were treated with 5 ng/ml TGF-1 for 48 h with or without tRA at varying concentrations. Picro-sirius red (PSR) staining and spectrophotometric analysis were used to quantify total collagen deposition. A rat extracellular matrix and adhesion molecules polymerase chain reaction (PCR) array was used to determine changes in expression of 84 genes associated with fibrogenesis in NRK-49F cells treated with TGF-1 +/- 2 M tRA for 48 h. Reverse transcriptase quantitative PCR (RT-qPCR) was used to study molecular markers of fibrogenesis not included in the PCR array including TGF-1, -2, -3, plasminogen activator inhibitor-1 (PAI-1), and tissue transglutaminase-2 (TG2) at different time points. RT-qPCR was also used to determine mRNA expression of CRABP-II and FABP5 in response to 2 M tRA and TGF-1 at different time points. RESULTS: tRA dose-dependently increased PSR staining of NRK-49F cells that was further increased by TGF-1. Despite this net-pro-fibrotic effect of tRA, selected molecular markers of fibrogenesis were down-regulated by tRA in the presence of TGF-1 at mRNA level including collagens I and III, fibronectin, and connective tissue growth factor. There was also down-regulation of selected matrix degradation enzymes including matrix metalloproteinase (MMP)13 and up-regulation of PAI-1 and TG2 suggesting that matrix accumulation due to a reduction in degradation may play a role in the pro-fibrotic effects of tRA in this rat renal fibroblast cell line. CRABP-II had a higher basal mRNA expression than FABP5 in NRK-49F cells. There was an early induction by 6 h followed by a later suppression of CRABP-II following treatment with tRA and TGF-1, but a later induction of FABP5 expression following TGF-1 and dual treatment at 48 h. CONCLUSIONS: tRA has dual potential in regulating fibrogenesis in a cell- and genespecific manner. The two tRA carrier proteins had different expression levels and responded differently to tRA and TGF-1 suggesting that retinoid signalling pathways are important in the fibrogenic response. If so, targeting specific retinoid signalling pathways may allow us to maximise the anti-fibrotic effects and minimise the pro-fibrotic effects of tRA so that retinoids may be used effectively and safely in human renal diseases.