SURFACE ANATOMY OF THE ABDOMEN Part 1
advertisement
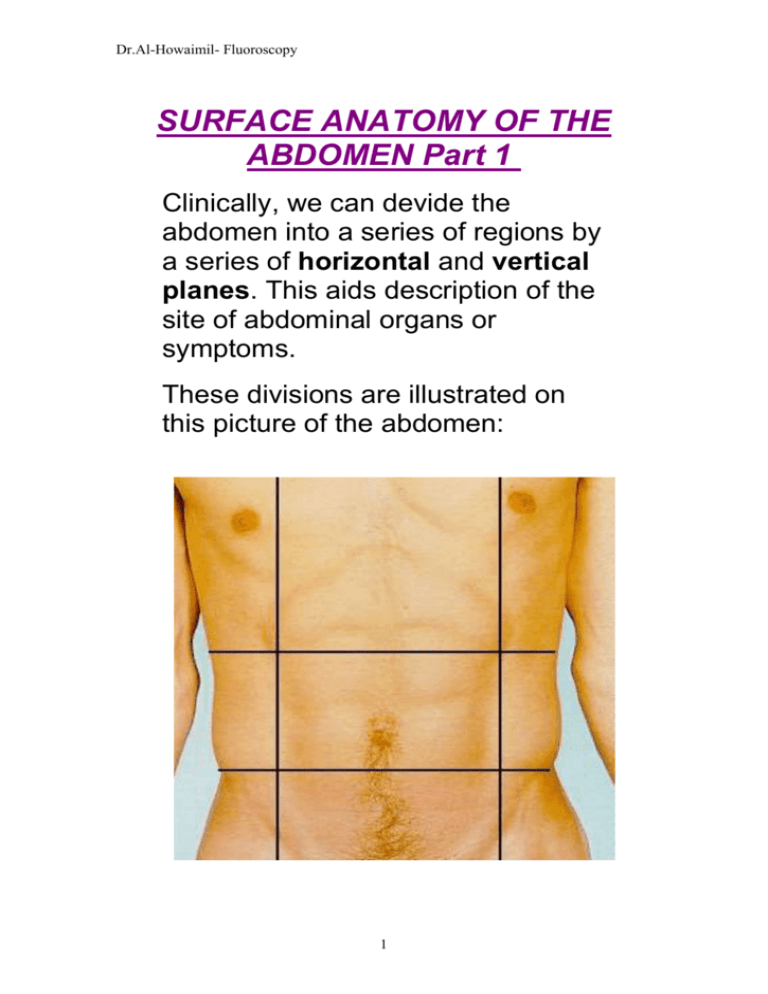
Dr.Al-Howaimil- Fluoroscopy SURFACE ANATOMY OF THE ABDOMEN Part 1 Clinically, we can devide the abdomen into a series of regions by a series of horizontal and vertical planes. This aids description of the site of abdominal organs or symptoms. These divisions are illustrated on this picture of the abdomen: 1 Dr.Al-Howaimil- Fluoroscopy The subcostal plane passes through the lowest parts of the costal margins (SC). It lies approximately at the level of the 3rd lumbar vertebra. It varies with age, lying higher in children. It also lies higher in the supine subject, often level with the 2nd lumbar vertebra. An alternative plane can be drawn through a point halfway between the jugular notch and the pubic symphysis called the transpyloric plane. This passes through the pylorus of the stomach. It should also correspond to the level of the lower border of the first lumbar vertebra. The transtubercular plane passes through the tubercles of the iliac crests (TT). It corresponds with the level of the spinous process of the 5th lumbar vertebra. Another plane often encountered is the supracristal plane which represents a line drawn through the highest part of the iliac crests (SCR). It lies at the level of the 4th 2 Dr.Al-Howaimil- Fluoroscopy lumbar spinous process. The umbilicus often lies just below this plane. When you examine a patient, you must be familiar with the different regions of the abdomen which are used to describe the location of any symptoms, pain, lumps or organs that might be found. For example, if pain is described as being in the right iliac fossa, this is characteristic of appendicitis. If you then examine the patient and find they are acutely tender in this 3 Dr.Al-Howaimil- Fluoroscopy region, you could describe the tenderness as being in the same region ie right iliac fossa. Taken with other signs and symptoms, you arrive at your diagnosis. These regions are described by surface anatomy and you should identify each region on the living subject. Imagine a pair of vertical lines drawn through a point which lies midway between the anterior superior iliac spine and the symphysis pubis. This is called the mid-femoral point. This line also corresponds to the mid-clavicular line. These lines have been drawn in on the illustration of the abdomen. Above the transpyloric plane, right and left hypochondriac regions (HC) are separated by the epigastric region located between them (E). Below the transpyloric plane, but above the transtubercular plane, is the umbilical region (U) in the mid4 Dr.Al-Howaimil- Fluoroscopy abdomen, with right and left lumbar regions (L) on either side. Below the transtubercular plane, the hypogastric region (HY) separates the two iliac fossae or regions. (RIF) - right: (LIF) - left). 5 Dr.Al-Howaimil- Fluoroscopy Dr. Al-Howaimil L: 1 Digestive system: Alimentary canal Accessory organs Alimentary canal: Hollow canal Include: Mouth, pharynx, esophagus, stomach, small and large bowel, rectum, anus. Accessory organs: Salivary gland, liver, biliry tract, pancreas Function of digestive system: 1- intake water, vitamins, mineral, digestive food acarbohydrate b- Lipids c- Protein 2- absorption of essential digestive food 3- Elimination of any use material as solid west product. 6 Dr.Al-Howaimil- Fluoroscopy Contrast media Radiolucent (- ve) air, co2, o2 Radio-opaque (+ ve) barium selphate Ba So4 Barium: Powder, chalk like substance, extremity un-soluble in water. Ba + water = suspension (not solution) Types: A-Thin: 1 part of Ba of 1 part of water Used for internal GIT Motility: Temperature General condition of patient Consistency of preparation B-Thick: 3-4 part of Ba of 1 part of water Used for esophagus Descend slowly and coat mucous Should be consistency of cooked cereal. Ba- contraindication: If any chance to escape into peritoneal cavity If surgery followed radiographic procedure use alternative contrast (water soluble iodinated contrast media eg. Gastroview or Gastrografin because it is easily removed by absorption before & during surgery) Type of Ba: Double: -ve and +ve Single: barium only. Post exam elimination: On the large bowel absorption of water so Ba may become a hardened and solidified and difficult to evacuate so patient may require laxative after exam but if laxative is contraindication, fluid or mineral oil used until stools are free from all erases of white. 7 Dr.Al-Howaimil- Fluoroscopy Barium swallow The abdominal viscera can be made visible on radiographs by the use of a suitable contrast medium, a radio-opaque dye which absorbs the x-rays as they pass through the abdominal structures. Barium sulphate solution is such a radio-opaque substance. The patient is given a glass of a milky white solution (the barium sulphate) which is swallowed. This creates a bolus of 8 Dr.Al-Howaimil- Fluoroscopy medium which passes down the oesophagus into the stomach and then into the duodenum, small bowel and eventually through the whole intestine. A thin coating of barium allows the radiologist and clinician to identify the surface of the gut mucosa. The barium meal is widely used to visualise the oesophagus, stomach, duodenum and small bowel. Introducing barium sulphate using an enema via the anus, a technique called a barium enema, permits the examination of the large bowel. Barium contrast studies can be used to outline the anatomy of the oesophagus as the barium passes through the chest. These examinations are called a barium swallow . The barium can be seen in the oesophagus (1). The oesophagus has walls which normally have longitudinal folds within them. These may be seen as irregular white lines. Swallowing a glass of 9 Dr.Al-Howaimil- Fluoroscopy barium sulphate suspension creates a bolus which passes down the oesophagus in the same way as food would. This fills the lumen and appears as a white shadow (2). The lower end of the oesophagus passes through the diaphragm and enters the stomach (3). The sphincteric action of the diaphragm occludes or closes the oesophagus as it pierces the diaphragm preventing the acidic stomach contents passing backwards up into the oesophagus. 10 Dr.Al-Howaimil- Fluoroscopy Dr, Al-Howaimil L; 2 Barium swallow Radiographic examination to study the form and function of pharynx and esophagus by using C\M Indication: 1. Anatomical anomalies 2. Foreign body obstruction 3. Esophageal reflux 4. Esophageal Artesia 5. Dysphasia. Contraindication: Non Patient preparation: Non Procedure: Patient in erect RAO position, to throw the esophagus clear of spine. Given cup of Ba and start swallow. Spot films are taken. After care: Non Complication: 1. Aspiration, 2. Unsuspected perforation. Infants: To demonstrate a trecho-oesphageal fistula in infants a naso-gastric tube is introduce to the level of the mid-esophagus, C\M injected forced to indicate any fistula .Films are taken at the same time. 11 Dr.Al-Howaimil- Fluoroscopy . The barium can be seen in the oesophagus (1). The oesophagus has walls which normally have longitudinal folds within them. These may be seen as irregular white lines. Swallowing a glass of barium sulphate suspension creates a bolus which passes down the oesophagus in the same way as food would. This fills the lumen and appears as a white shadow (2). The lower end of the oesophagus passes through the diaphragm and enters the stomach (3). The sphincteric action of the diaphragm occludes or closes the oesophagus as it pierces the diaphragm preventing the acidic stomach contents passing backwards up into the oesophagus. 12 Dr.Al-Howaimil- Fluoroscopy L; 3 Barium meal Radiographic examination to investigate upper alimentary tract including esophagus, stomach and duodenum. To detect any abnormal anatomical or functional conditions. Indication: 1- Peptic ulcers, 2- hiatus hernia, 3- gastritis, 4- tumor, 5- divertculae, 6- bezoars, 7- dyspepsia, 8- gastro-intestinal hemorrhage, 9- Partial obstruction. Contraindication: Perforation Patient preparation: Patient must arrive with empty stomach NPO from midnight until the exam time. No smoking or chewing during NPO period Female patient check the LMP & apply 10 day role. C\M: Double contrast (Ba + CO2) Gas producing agents: 1- produce adequate amount of gas i.e 200-400 ml 2- no interference with Ba coating 3- no bubble production 4- rapid dissolution, leaving no residue 5- easily swallow 6- low cost 13 Dr.Al-Howaimil- Fluoroscopy Procedure: Patient is giving a gas producing agents, Then given Barium to drink while he is laying on his left side supported by his elbow to prevent Ba. Not to move quickly to the duodenum and obscuring the greater curvature of the stomach . Then the patient is asked to lay supine with slightly to his right side to bring up the Ba. To the gastro-esophageal junction and the patient screened to check the reflux by asking the patient to cough or swallow water Then injected with bascopan 20 ml or glucagons 0.3 ml to relax the smooth muscle Then asked to roll in Rt side to complete circle and finish in RAO position for good coating . Films are taken. After care: 1- patient is warned about white bowel 2- patient is asked not to leave department until blurred vision is resolved Complication: 1- unsuspected perforation, 2- aspiration , 3- partial obstruction may lead to complete obstruction, 4- Side affect of pharmacological agents. 14 Dr.Al-Howaimil- Fluoroscopy L; 4 Barium follows through or small bowel serious (SBS) Radiographic examination of the small intestine to study the form and function of the 3 components of small bowel. Indication: 1. Pain, 2. Enteritis, 3. Neoplasm, 4. Hemorrhage, 5. Ileus, 6. Malabsorpation. Contraindication: 1. Perforation, 2. Large bowel obstruction Patient preparation: Laxative on evening Metoclopramide 20 min oral before exam to enhance the rate of gastric emptying. Preliminary film: Plain ABD film Procedure: 4 techniques: 1-upper GI- small bowel comp.: Routine upper GI + routine stomach study During upper GI study, patient should ingest 1 full cup of Ba & exact time is recorded. When flouro. of stomach is finished time is recorded 30 min after ingest 1 full cup of Ba PA film of proximal small bowel (around 15 min after finishing upper GI) 1\2 hrs interval films (with centering to iliac crest) until Ba reach large bowel usually 2 hrs 1 hr interval until Ba passes through the ileo-ceacal valve Spot films of ileo-ceacal valve & terminal ileum are taken. Radiologist may need delayed films are order to follow though large bowel usually after 24 hr. 15 Dr.Al-Howaimil- Fluoroscopy 2- Small bowel serious only: Plain ABD film 2 cup of Ba ingested, record the time After 30 min take film high centering to include proximal small bowel 1\2 hrs interval films (with centering to iliac crest) until Ba reach large bowel usually 2 hrs 1 hr interval until Ba is well into ascending colon. 3- Intubations: Nasogastric tube is passed though the patient nose, esophagus, stomach, duodenum, and into jejunum, CM ingested in RAO position and that will help in passing the tube by peristalsis movement and record the time After 15- 30 min films are taken. 1 hr interval when required. 4- Enteroclysis: Patient is intubated under fluoroscopy C\M with special Enteroclysis catheter which pass into the region of duodenal-jejunum junction Ba sulphate is instilled air or methyl cellulose is injected into the bowel to distend it and provide double DC DC dilated the loops of small bowel while increase visible of mucosa. Films are taken. Disadvantage: 1- increase patient discomfort 2- long exam time 3- possible perforation Advantage: Ideal for patient with bowel obstruction and malabsorption After care: Complication: the same as the Ba. Meal 16 Dr.Al-Howaimil- Fluoroscopy L; 5 Barium enema A method of investigation of colon by using C\M to study the form and function of large intestine. Indication: 1. colitis, 2. neoplasm, 3. divertcullum, 4. Volvus. Contraindication: 1. rectal biopsy, 2. colonscopy, or sigmoidscopy 3. sever diarrhea, 4. Inflammation lesions e..g. appendicitis . 5. obstruction Patient preparation: The patient must arrive with empty colon 1. Patient kept to low residue diet for 4 days 2. laxative agent 48 hrs before exam. 3. colon washout 4. NPO 4-6 hrs before exam. 5. Patients undress copletly &wear gown. Procedure: Patient on lat. position with opposite knee flexed, Well lubricated catheter is inserted 10 cm into rectum Patient may injected with with Bascopan, Then patient is Positioned in prone, Enema reservoir is 100 cm over the table and table tilted so head is at an angel 100 Ba runs until reach splenic flexure Air pumped to produce DC Patient rotated, films are taken. 17 Dr.Al-Howaimil- Fluoroscopy After care: 1. patient is warned about white bowel 2. patient is asked not to leave department until blurred vision is resolved 3. Patient must be fit enough to leave department. Safety concerns during Ba enema; 1- review patient’s chart 2- never force an enema tip into rectum 3- the height of enema bag should not exceed 100 cm 4- verify the water temperature of C\M 5- Escort the patient to rest room. 18 Dr.Al-Howaimil- Fluoroscopy BARIUM STUDIES: LARGE BOWEL You should be able to identify the various components of the bowel on these films. Note the caecum (1), ascending colon (2), transverse colon (3), descending colon (4) and the rectum (5). On the right, the ascending colon turns towards the midline. This is called the right colic flexure (6) (also known as the hepatic flexure - so called as it is adjacent to the liver). On the left, the transverse colon turns downwards, creating the left colic flexure (7) (or splenic flexure - so called as it is adjacent to the spleen). 19 Dr.Al-Howaimil- Fluoroscopy BARIUM STUDIES: LARGE BOWEL 2 The sigmoid colon and the rectum can also be examined in the barium enema studies. Views may be taken in the prone postero-anterior position or in lateral or oblique positions. Make sure you understand what these terms mean. The rectum appears well filled with barium (10). Superior to the rectum and hidden by its outline can be seen the sigmoid colon (11). The lower part of the descending colon can also be identified (12). 20 Dr.Al-Howaimil- Fluoroscopy L: 6 Sialography Definition: A radiographic visualization of salivary glands and its ducts * provides both diagnostic and preoperative information in case of salivary glands pathology). Indication: 1- Pain 2- Calculi 3- strictures of ducts ا 4- sialctasis 5- tumor Contraindication: Sever inflammatory of salivary glands ducts History of sensitivity of iodinated contrast media Contrast media: 1- oily: Ethiodol (have slow excretion rate, give a greatest density, but may cause granulomatus tissue. 2- W.S.I .: Renografin (good for routine sialography) Patient preparation: None but check history of allergies Procedure: In case of suspected sialothiasis scout films are required. Determination of salivary ducts by: palpation ducts or sucking on a lemon slice. Ducts are dilated by standard double-ended blunt dilators or lacrimal probes Then ducts canulated (the most preferred; Abbott butterfly set) Wing is secured with hemostat cannula should be refilled with CM to avoid Injection of air bubbles and immobilized The tubing with syringe are taped to 21 Dr.Al-Howaimil- Fluoroscopy shoulder or chest Then CM injection slowly under fluoroscopy -----then Spot films are taken Views: Delayed films are taken to study the function emptying of gland Films: Preliminary films: Parotid gland: 1- AP with head rotated 5 away from the side under investigation 2- Lat 3- Lat-oblique Submandibular gland: 1- infer superior using occulusal 2- lat 3- lat-oblique After injection of CM: 1- infer superior using occulusal 2- lat 3- lat-oblique Post secretary: 1. infer superior using occulusal 2. lat 3. lat-oblique After care: -----None Complication: Pain Damage to duct orifice Rupture of duct Infection 22 Dr.Al-Howaimil- Fluoroscopy L: 7 Maylography A radiographic study of spinal cord and its nerve root branches Indication: Detect any lesion may be presented within spinal canal For example: Space occupying lesions Degenerative disease of central nervous system(CNS) Malformation of the spinal cord. Contraindication: Blood in CSF Arachnoiditis Increase intracranial pressure Lumber puncture performed 2 weeks of current examination Patient preparation: Patient encouraged drinking fluids before exam to decrease incidence of lumber puncture headache Patient maturate before exam To decrease anxiety and to relax patient, sedative relaxant agent may be given 1 hr before exam NPO 4hr before exam. Contrast media: 23 Dr.Al-Howaimil- Fluoroscopy must meet the following requirements: 1- miscible (mixed well with CSF) 2- has good radopacity 3- easily absorbed 4- non toxic 5- inert(non reactive) ----------------------------------------------------------1- oily contrast media 5-6 ml of myodil Advantage: Provides good radiopacity Little complication Disadvantage: Not demonstrate root broches adequately Not absorbed by the body, so must be removed Needle is placed in place, so positioning of patient is difficult Residual oil-based CM is absorbed by the body ---------------------------------------------------------2- WSI c/m 8-10 ml Provides good visualization of nerve root Absorbed quickly Spinal needle can be removed so patient can be positioned Absorption begins 30 min post injection. 24 Dr.Al-Howaimil- Fluoroscopy Procedure: Lumbar puncture method: By injection of CM into subrachnoid space Patient placed in seated or lat-decubitus for injection. Skin is prepared and infiltrated with anesthetic agent Stylist needle inserted into subrachnoid space Stylet removed spinal fluid flows from the needle Site of injection is lower lumbar region, this area reduce the possibility of trauma to the spinal cord Between 2nd -3rd lumber vertebrae (For cervical c3 – c4 or c4-c5 ) Small sample of spinal fluid is collected for laboratory At the same time Blood pressure can be taken after CM is injected (Withdrawing a small amount of spinal fluid and replacing it with equal amount of CM) Patient rotated into prone position and head kept straight i.e. with chine resting on pad and table is tilted so CM move upward and not entering the head) Views: Patient porn position usually 2-3 exposures on 24 * 30 or 35 * 35 and L or R markers should be used Lat view are taken in porn and anterior oblique 25 Dr.Al-Howaimil- Fluoroscopy After care: Patient returned to the word on stretcher Patient lies flat for at least 8 hr Patient trunk raised and supported by billows at an angle of 45 to prevent residue CM from entering the head Pulse and blood pressure are checked and recorded Every ½ hr for next 4 hr then 4 hourly for 24 hr. 26 Dr.Al-Howaimil- Fluoroscopy L: 8 Micturating CystoUrethroGraphy (MCUG) Indication: 1- Vesico-ureteric reflux. 2- Study of the urethra during minctrution. 3- Abnormalities of the bladder. 4- Stress incontinence. Contraindication: 1- Acute urinary tract infection. CM: HOCM or LOCM 150. Equipment: 1- Fluoroscopy unites with spot film. 2- Video recorder. 3- Foley catheter. Patient preparation: The patient micturate prior the examination to empty the bladder. The purpose of MCUG: 1- To demonstrate Vesico-ureteric reflux. 2- To demonstrate Vesico-vaginal or recto-vesical fistula. 3- To demonstrate stress incontinence. Preliminary film: Coned view to bladder. Procedure: 1- TO DEMONSTRATE VESICO-URETERIC REFLUX 1- Patient lies supine on the x-ray table. 2- Using aseptic technique. 3- Insert catheter in to bladder. 27 Dr.Al-Howaimil- Fluoroscopy 4- Residual urine is drained. 5- CM is slowly dripped in and the bladder filling. 6- The catheter should not be removed until no more CM will be drip into the bladder. 7-sopt films are taken during micturation and any reflux recorded. The lower ureter is best seen in to AO position. Boys should micturate with AO position with opposite knee flexed. 8- A full-length view of the Abd. Is taken to demonstrate any reflex of CM that might have occurred unnoticed into the kidneys and to record the post-micturation residue. 2- TO DEMONSTRATE VESICO-VAGINAL OR RECTOVESICAL FISTULA As above, but films are taken in lat position. 3- TO DEMONSTRATE STRESS INCONTINENCE As above, but the catheter is left in situ until the patient is in the erect position. Films should include sacrum and symphysis pubis because bony land marks are used to assess bladder neck descent. Views: 1- Lat bladder. 2- Lat bladder, straining. 3- Lat bladder during micturation. After care: Patient should be warned about dysuria. Complication: DUE TO CM: 1- Adverse reaction may result from obstruction of CM BY the bladder mucosa. 2- CM induced cystitis. DUE TO TECHNIQUE: 1- Acute urinary tract infection. 2- Catheter trauma- may produce dysuria, frequency, haematuria and urinary retention. 3- Retention of a Foley catheter. 28 Dr.Al-Howaimil- Fluoroscopy 29 Dr.Al-Howaimil- Fluoroscopy L. 8 Micturating Cystourethrogram (MCUG) Indications for imaging Vesicoureteric reflux in children - in recurrent UTI Stress incontinence Urethral stricture Bladder dysfunctions Contra Indications Current - urinary tract infection Contrast media allergies - cautionsAnatomy Demonstrated Technique (typical for demonstration of reflux in a child) This is normally a paediatric procedure, therefore all normal paediatric imaging considerations are vitally important in this embarrassing and invasive procedure Some centres give prophylactic antibiotic cover. The patient lies supine on the examination table for catheterisation if not already catheterised outside the department, the patient is catheterised. Bladder catheterisation is an aseptic procedure undertaken by a suitable trained and qualified person. The contrast media warmed to body temperature is slowly infused through the catheter using a "giving set" into the bladder, intermittent pulsed fluoroscopy is used to check the filling and for reflux up the ureters. The contrast media reservoir should be no more than 1 metre above the 30 Dr.Al-Howaimil- Fluoroscopy table to limit the pressure. An alternative to spot films is to video tape the fluoroscopy. 1) Spot films are taken of the bladder, kidneys and ureters to record the normal or abnormal anatomy. 2) When the bladder is considered full or the contrast leaks round the catheter the balloon is deflated and the catheter withdrawn. depending on the age of the patient the patient is asked to micturate into a receiver either erect or supine, suitable privacy and sympathy may be required. 3) Spot films are taken during micturition and any reflux recorded, The patient is rotated into the 30 degree left and right anterior obliques to demonstrate the bladder ureteric junctions, to demonstrate the male urethra the left anterior oblique position is adopted with flexion of the right hip and knee to visualise the whole of the male urethra. 4) A final full length abdominal film is taken to visualise the kidneys. Variations For stress incontinence the film series is taken to include , at rest, straining and micturating in the lateral position, some centres have special sitting fluoro arrangements. For fistulae and bladder tract abnormalities a series of films in AP. lateral and oblique positions may be required. Contrast Media Low strength (approx 25% weight/volume) contrast agent i.e. Hypaque 25% urografin 150, suitable volume to fill the bladder, typical 20 ml in an infant to 500 ml in an adult, the contrast media should be warmed to body temperature. Radiation protection General fluoroscopic dose limiting precautions should be employed. Equipment NursingCatheterisation pack - and aseptic procedure pack.. Sterile towels Skin prep./ wash Sterile lubricant Giving setSelection of Foley catheters 5 -7 gauge French in infants larger in adults. Drip stand Radiographic Fluoroscopy set with spot film or video recording devices. Complications Temporary Dysuria Transient Haematuria from catheterisation. Cystitis 31 Dr.Al-Howaimil- Fluoroscopy Aftercare Non specific, general patient post procedure care. Evaluation of the Image ID and anatomical markers must be present and correct in the appropriate area of the film. Optimal exposure should penetrate all the bone structures and contrast should be low enough to visualise fully the bone and soft tissue structures. Images should be marked with contrast volume and indications of voiding or straining. Radiographs Full length voiding film showing reflux into the right kidney Additional modalities Ultrasound is a useful adjunct RNI may be used to assess renal scarring in cases of proven reflux. Useful Text: A Guide to Radiological Procedures, Chapman & Nakielny 32 Dr.Al-Howaimil- Fluoroscopy L: 8 Arthrography A contrast media study of synovial joints & related soft structures including hip, shoulder, elbow, ankle, wrist, TMJ and knee Knee tech. mostly similar for all joints. Knee arthrography Performed to demonstrate & assess the knee joint & associated soft tissue structures for pathology including joint capsule, menisci, (Collateral, cruciate, minor)ligaments Indication: Traumatic: Tears of joint soft structures capsule Non-traumatic: pathology (Baker’s cyst) Contraindication: Allergy to C\M 33 Dr.Al-Howaimil- Fluoroscopy Contrast media :Double contrast 5 ml of low density CM e.g. Renografin 80-100 cc of CO2, O2 , or air Preliminary film: AP + Lat AP Lat. Procedure: Patient lies supine and pad is placed under popliteal fosse and knee slightly flexed. Skin is cleaned and sterile towel is dropped around the knee Skin infiltrated with local anesthetic and thin walled (19 – 21 gage) needle is inserted into the joint. Fluid from joint is aspirated and 3 ml of 1\1000 adrenaline is injected to reduce the rate of absorption of CM Which is useful in case of sinovitis The CM is injected under fluoroscopic control ,followed by 40 ml of air until supra-patellar pouch is tense (like balloon) then needle is removed 34 Dr.Al-Howaimil- Fluoroscopy Knee extends & flexed several time to distribute the CM Patient turned in prone position and (varus and valgus) being applied until each meniscus is separated by gas Views: Usually 4 views of each quadrate of knee AP + lat with knee flexed to demonstrate cruciatel After care: No special after care but patient should be warned that he may experience discomfort for several days Knee will sequelsh when flexed or straightened. 35 Dr.Al-Howaimil- Fluoroscopy L: 9 T-tube postoperative [delayed] Cholangiography Performed in the radiology department following a cholecystectomy where the surgeon concerns about residual stones in the biliary duct, so he will place a special T tube catheter into CBD (commune bile duct) and extend outside the body. The purpose: 1. Visualize any residual undetected stones 2. Evaluate the status of the biliary duct system 3- Demonstrate the small lesions, strictures or dilatation Contraindication: None C\M: Hypaque Preliminary film: Coned PA of Rt. side of abdomen. Procedure: This Procedure performed between 3rd 10th days following a cholecystectomy Patient lies supine and drainage tube clamped near the patient and cleaned with antiseptic 23 G needle , extension tubing and 20 ml syringe are assembled and filled with CM 36 Dr.Al-Howaimil- Fluoroscopy after removing air bubbles , needle is inserted into tubing between the patient and clamp Films & views: PA RAO LAO After care: Non Complication: Adverse reaction Septicemia 37 Dr.Al-Howaimil- Fluoroscopy Hysterosalpingography: Examination of the female reproductive system using contrast media. Indication: 1. Infertility. 2. Recurrent miscarriages. 3. Following tubule surgery. Contraindication: 1. Pregnancy. 2. Acute pelvic inflammatory disease. 3. Active uterine bleeding. Contrast media: Omnipaque300 Equipments: They are inside a closed sterilized box. 1. Speculum vaginal: 2pices. They come two sizes: large35cm. /medume20cm. 2. Tenaculums: 2pices. Toothed 25cm 3.foceps: 2pices. Sponge 25cm. 4.bowls: 2 25cc 5.towels: 2 6.sterilized pair of gloves. 38 Dr.Al-Howaimil- Fluoroscopy Set of salpingograph: 1.OB-Gyneleechcannula with 2 stylets: sml. /med./large. 2.Cones: small/med./large. 3.three-way stopcock 4.labrcating jell. 5.tray Position: Patient is supine with knees flexed and legs abducted. Procedure: Patient lie supine with knee flexed and places her feet at the end of the table. With sterile towels and technique a vaginal speculum is inserted into the vagina. The vaginal walls and cervix are cleansed with an antiseptic solution. A cannula or ballon catheter is then inserted into the cervical canal. Dilation with a balloon catheter helps to occlude the cervix preventing c/m from flowing out of the uterine cavity during the injection phase. A tenaculum may be necessary to aid in the insertion and fixation of the cannula or catheter. Once cervical placement of cannula or catheter is obtained ,a syringe filled with c/m is attached to the cannula or balloon catheter. Using fluoroscopy the physician slowly injects the c/m into the uterine cavity. If the uterine tubes are open c/m will flow from the distal ends of the tubes into the peritoneal cavity. 39 Dr.Al-Howaimil- Fluoroscopy Films: 1.preliminary film for the pelvic. 2.when the c/m is injected. 3. When it reaches the tubes 4. When c/m reaches the uterus. After care: The patient is tolled that she may have bleeding for1or 2 days and pain. 40