Seattle University Student Health Clinic
advertisement

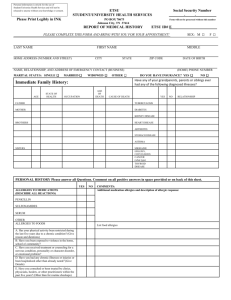
Seattle University Student Health Clinic Health History Form Name: Date of Birth: Last First MI Birth Place: Month Day Year Have you had or do you have any of the following conditions: (please check items you are experiencing or have experienced before and indicate the year of occurrence) Problem acne eczema/psoriasis fungal infections concussion/head injury epilepsy migraine/headaches dizziness/fainting ear infection eye or vision trouble sinusitis allergies/hayfever tonsillitis breast lump asthma pneumonia bronchitis tuberculosis Year Problem positive TB test congenital heart disease heart murmur high blood pressure rheumatic fever anemia other blood disorders bleeding problems acid reflux stomach ulcer intestinal disorder gallbladder trouble hernia hemorrhoids/fissures recurrent diarrhea recurrent vomiting bladder infection Year Problem kidney infection kidney stone liver disease ovarian cyst endometriosis pelvic infection sexually transmitted disease:(chlamydia, gonorrhea, herpes, warts, other) abnormal pap smear testicular problems high cholesterol diabetes thyroid disease broken bones arthritis/bursitis Year Problem Year bone/joint deformity neck injury back injury recurrent back pain knee injury shoulder injury ligament repair depression panic/anxiety attacks sleep problem ETOH/drug dependency anorexia/bulimia mononucleosis hepatitis malaria tumor/cancer chicken pox Other serious illnesses or injuries not listed: Are you receiving treatment for any of the problems noted above? If so please give details: Have you ever had surgery? If so, when and why: Have you ever been hospitalized? If so, when and why: Have you ever received mental health counseling? If so, when and why: Do you take any medications on a regular or intermittent basis? If so, what, why and how frequently: ___________________________________________________________________________________________________ Do you have any drug allergies? If so, what drug and what type of reaction: Do you have any other allergies? (e.g. bee stings): F a m il y Health Histor y: heart attack high cholesterol high blood pressure stroke diabetes Check any disease that has occurred to any blood relative ______ kidney disease ______ ______ breast cancer ______ ______ migraine ______ ______ depression ______ ______ cancer ______ glaucoma arthritis blood disorder other THIS IS A 2-SIDED FORM PLEASE COMPLETE SIDE 2 ______ ______ ______ Social History: Marital status: ____ single ____ married ____ partnered ____ divorced ____ separated ____ widowed Number of children, age and sex Academics: ____ Freshman _____ Sophomore _____ Junior _____ Senior _____ Graduate Program Major: ________________________ Work/Occupation: ______________________ Living situation: _____ Campus housing _____ Off Campus Do you smoke currently or have you ever smoked? _____ Yes _____ No Cigarettes/day _____ Years smoked _____ When quit Do you participate in intercollegiate sports? _____ Yes _____ No If so, what sport? Do you have a daily exercise routine? If so, what do you participate in and how frequently? How many meals per day do you eat? What food groups do you eat? _____ Breads _____ Fruit _____ Vegetables _____ Meat/fish _____ Dairy Do you currently, or have you ever had problems with eating disorders like anorexia or bulimia? _____ Yes _____ No Do you drink caffeinated beverages? If so, how many cups/cans per day? Do you drink alcoholic beverages? If so, what and how much per week? Have you ever been concerned about the amount of alcoholic beverages you drink? Do you have any body piercings or tattoos? _____ Yes _____ No If so, where? Medical Provider comments: Medical Provider signature: _____________________________________________________ Date Patient Rights and Responsibilities Patients have the right to: 1. Change their primary health care providers if they choose. 2. Have their personal privacy respected. 3. Receive an explanation of their diagnosis, treatment, and prognosis. 4. Know the names and positions of people involved in their care. 5. Refuse treatment except where prohibited by law. 6. Participate in all health care decisions. 7. Full confidentiality of their medical records, released only with their authorization unless an exception applies and disclosure is permissible or required. 8. Review any medical records maintained by the SHC. Patients have a responsibility: 1. To provide accurate information about their past health history. 2. To ask questions if explanations or instructions were net understood. 3. To pay all charges that are billed to them. 4. To complete an evaluation form regarding satisfaction with services received. I have read the above Patient Rights and Responsibilities. Signature: _______________________________________________________________ Date: