Relationship Between Renal Function and Extracorporeal
advertisement

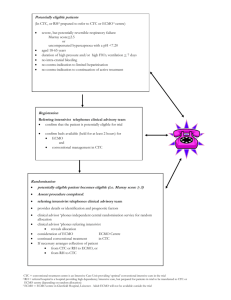
A- ARF quoted without specification F- 05 : Hemofiltration F- 08 : cardiovascular complications E- 03 : chronic heart failure E- 03 : Pulmonary oedema Relationship Between Renal Function and Extracorporeal Membrane Oxygenation Use: A Single-Center Experience Punkaj Gupta, Jacob Carlson, Dennis Wells, Patrick Selakovich et al. Journal : Artificial Organs Year : 2015 / Month : April Volume 39 Pages 369–374 DOI: 10.1111/aor.12379 Keywords: Extracorporeal membrane oxygenation; Renal function; Pediatric cardiopulmonary support; Intensive care unit ABSTRACT The effects of extracorporeal membrane oxygenation (ECMO) support on renal function in children with critical illness are unknown. The objective of this study was to investigate the impact of ECMO on renal function among children in different age groups. We performed a single-center retrospective observational study in critically ill children ≤18 years supported on ECMO for refractory cardiac or pulmonary failure (2006–2012). The patient population was divided into four age groups for the purpose of comparisons. The Acute Kidney Injury Network's (AKIN's) validated, three-tiered staging system for acute kidney injury was used to categorize the degree of worsening renal function. Data on patient demographics, baseline characteristics, renal function parameters, dialysis, ultrafiltration, duration of mechanical cardiac support, and mortality were collected. Comparisons of baseline characteristics, duration of mechanical cardiac support, and renal function were made between the four age groups. During the study period, 311 patients qualified for inclusion, of whom 289 patients (94%) received venoarterial (VA) ECMO, 12 (4%) received venovenous (VV) ECMO, and 8 (3%) received both VV and VA ECMO. A total of 109 patients (36%) received ultrafiltration on ECMO, 58 (19%) received hemodialysis, and 51 (16%) received peritoneal dialysis. There was a steady and sustained improvement in renal function in all age groups during the ECMO run, with the maximum and longest-sustained improvement occurring in the oldest age group. Proportions of patients in different AKIN stages remained similar in the first 7 days after ECMO initiation. We demonstrate that renal dysfunction improves early after ECMO support. Irrespective of the underlying disease process or patient age, renal function improves in children with pulmonary or cardiac failure who are placed on ECMO. COMMENTS Mechanical circulatory support in the form of extracorporeal membrane oxygenation (ECMO) is an invaluable tool in the care of children with severe refractory cardiac and/or pulmonary failure .However, many patients on ECMO develop renal dysfunction and acute kidney injury, leading to increased mortality. ECMO, first introduced clinically in 1972, has since been applied as a means of cardiopulmonary support for patients with potentially reversible cardiac and/or respiratory failure in whom conventional medical strategies have been exhausted. End-organ perfusion in adults with critical illness can be improved with the implantation of mechanical cardiac support devices such as ventricular assist devices (VADs) However, the effects of ECMO on end-organ function in children with critical illness are unknown. The primary aim of this study was to compare the effects of ECMO on renal function in critically ill children of different age groups. A secondary aim of this study was to study the effect of ECMO on renal function in children with compromised renal function. They used their AKIN classification defining 3 stages of AKIN: Stage 1 was defined as an increase in plasma creatinine ≥0.3 mg/dL or to ≥150% to 200% (more than 1.5-fold to twofold) from baseline. Stage 2 was defined as an increase in plasma creatinine to ≥200% to 300% (more than twofold to threefold) from baseline,stage 3 was defined as an increase in plasma creatinine to >300% (more than threefold) from baseline or to a level of ≥4.0 mg/dL, with a rise of at least 0.5 mg/dL, or as need for renal replacement therapy. During the study period, 109 patients (36%) received ultrafiltration on ECMO, 58 patients (19%) received CVVHD or other HD, and 51 patients (16%) received peritoneal dialysis. A total of 289 patients (94%) received VA ECMO, 12 (4%) received VV ECMO, and 8 (3%) received both VV and VA ECMO. Overall mortality at hospital discharge was 127 (41%). Overall ICU LOS from start of ECMO was 32 days (IQR 17–63 days), and ICU LOS after end of ECMO was 23 days (IQR 8–52 days). The most common reasons for use of dialysis included worsening renal function, electrolyte disturbances, and/or fluid overload. There was a mortality difference in patients receiving dialysis compared with patients receiving no dialysis (67% vs. 30%, P < 0.001). Renal dysfunction improved early after ECMO support (VA or VV) was instituted. Despite differences in their underlying disease processes, a sustained and steady improvement in eGFR was observed in patients receiving ECMO in all age groups, with the maximum improvement occurring in older patients. To conclude, renal dysfunction improves early after extracorporeal membrane oxygenation support. Irrespective of the underlying disease process or patient age, renal function improves in children on ECMO with pulmonary or cardiac failure. The current study demonstrates that renal function improves with use of renal replacement therapy. These results were consistent among all age groups and did not vary with the underlying disease process. The small size of the study has not allowed the demonstration of superiority of any of the tested dialysis techniques. Pr. Jacques CHANARD Professor of Nephrology